Abstract
The study was aimed at determining the vascular expression of oncofetal fibronectin (oncfFn) and tenascin-C (oncfTn-C) isoforms in renal cell carcinoma (RCC) and its metastases which are well-known targets for antibody-based pharmacodelivery. Furthermore, the influence of tumour cells on endothelial mRNA expression of these molecules was investigated. Evaluation of vascular ED-A+ and ED-B+ Fn as well as A1+ and C+ Tn-C was performed after immunofluorescence double and triple staining using human recombinant antibodies on clear cell, papillary and chromophobe primary RCC and metastases. The influence of hypoxic RCC-conditioned medium on oncfFn and oncfTn-C mRNA expression was examined in human umbilical vein endothelial cells (HUVEC) by real time RT-PCR. There are RCC subtype specific expression profiles of vascular oncfFn and oncfTn-C and corresponding patterns when comparing primary tumours and metastases. Within one tumour, there are different vessel populations with regard to the incorporation of oncfTn-C and oncfFn into the vessel wall. In vitro tumour-derived soluble mediators induce an up regulation of oncfTn-C and oncfFn mRNA in HUVEC which can be blocked by Avastin®. Vascular expression of oncFn and oncTn-C variants depends on RCC subtype and may reflect an individual tumour stroma interaction or different stages of vessel development. Therefore, oncFn or oncTn-C variants can be suggested as molecular targets for individualized antibody based therapy strategies in RCC. Tumour-derived VEGF could be shown to regulate target expression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Angiogenesis is a crucial step in tumour progression. In tumour vessels, the perivascular extracellular matrix (ECM) contains oncofetal isoforms of tenascin-C (oncfTn-C) and fibronectin (oncfFn) not detectable in quiescent endothelium (Neri and Bicknell 2005; Eble and Niland 2009). Isoforms of Fn and Tn-C are generated by alternative splicing (Schwarzbauer 1991; Orend and Chiquet-Ehrismann 2006). Large variants containing up to nine extra domains in case of Tn-C or the extra domains A and/or B in case of Fn are expressed during embryogenesis and tissue reorganization processes like wound healing and tumour growth (therefore named as “oncofetal”). The restricted appearance in adults makes them promising structures for antibody-based targeted pharmacodelivery in tumour therapy (Schliemann and Neri 2010). To exploit the oncfFn and oncfTn-C variants in targeted drug delivery, knowledge on their expression pattern in tumours is of substantial clinical interest. Differences in their occurrence and vascular distribution in various tumours and tumour subtypes have been shown recently (Berndt et al. 2010). Humanised small immunoprotein (SIP) format antibodies against several oncofFn and oncfTn-C splice variants already exist. The antibody L19, targeting the extra domain B of fibronectin (ED-B+ Fn), is already subjected to clinical evaluation as radio or immunoconjugate (Carnemolla et al. 2002; Santimaria et al. 2003; Neri and Bicknell 2005; Johannsen et al. 2010). The SIP format antibody F8, targeting the fibronectin extra domain A (ED-A+ Fn), could be shown to accumulate in tumour vessels, too (Villa et al. 2008). The existence of large Tn-C isoforms in a lot of tumours has been known for nearly two decades (Borsi et al. 1992; Hindermann et al. 1999; Berndt et al. 2006). Their preferential vascular expression could be shown more recently (Brack et al. 2006). A recombinant antibody recognizing the splicing domain A1 of Tn-C (F16) conjugated to IL2 in combination with chemotherapeutic agents led to tumour growth reduction in a breast cancer xenotransplant model (Mårlind et al. 2008) and to size reduction in a glioblastoma xenotransplant model (Pedretti et al. 2010). The antibody is currently evaluated in clinical phase Ib trials in combination with doxorubicin or paclitaxel. Furthermore, an antibody against the splicing domain C of Tn-C (G11) binds selectively in tumour vessels and atherosclerotic plaques (Berndt et al. 2006; Silacci et al. 2006; von Lukowicz et al. 2007; Berndt et al. 2010).
Because of the obvious occurrence of oncofFn and oncfTn-C variants in association to vascular structures in renal cell carcinoma (RCC), this tumour entity is a good candidate for targeted pharmacodelivery using the mentioned SIP antibodies (Berndt et al. 2010). Promising results in clinical phase I trials suggests the activity of L19-IL2 in patients with mRCC (Johannsen et al. 2010). Although crucial for planning individual treatment strategies, there is no information on the differential expression and histological distribution of the vascular antigens recognized by the above mentioned antibodies in RCC subtypes and metastases. Therefore, we examined the blood vessel associated expression of A1+ and C+ Tn-C as well as of ED-A+- and ED-B+ Fn isoforms in clear cell, papillary and chromophobe RCC. Furthermore, we compared their distribution pattern in clear cell RCC primaries and metastases in human and in RCC orthotopic xenograft models. To analyse the impact of tumour-derived factors on vascular expression of oncofetal Fn and Tn-C, the mRNA expression of the Tn-C A1 domain and of the Fn EDA and EDB domains was assessed in human umbilical vein endothelial cells (HUVEC) after stimulation with conditioned medium of different RCC cell lines prepared under hypoxic conditions.
Materials and methods
Tissue material and cells
Frozen tissue samples of 9 clear cell RCC (ccRCC), 10 papillary RCC (pRCC), and 9 chromophobe RCC (chRCC) as well as 9 pairs of RCC primary tumours and metastases (8× ccRCC, 1× pRCC) (from bone, lung and liver) were available for analyses. Diagnosis was performed on the corresponding paraffin-embedded tissue according to the WHO classification criteria of 2004. Ethical approval was obtained from the Local Research Ethic Committee of the Friedrich Schiller University, Jena.
Two pairs of human RCC xenografts and synchronous metastases were obtained by orthotopically implanting 1 × 106 RXF393 or SN12K1 cells in the kidney of 6- to 8-week-old female NCr-nu/nu mice (Harlan Correzzana, Italy) as described (Naito et al. 1986; Frey et al. 2010). Kidney bearing tumour and lung nodules were snap frozen and stored at −80°C. Animal experiments were conducted in conformity with institutional guidelines that are in compliance with national and international laws and policies.
The RCC cell lines A498 and Caki1 were used for the generation of conditioned media. The VHL mutation status was assessed by sequencing all coding exons using primers and method as described previously (Tong et al. 2006). For detection of larger deletions, a MLPA analysis using the P016B kit from MRC Holland (MRC-Holland, Amsterdam, The Netherlands) was done.
Primary human umbilical vein endothelial cells (HUVEC) were isolated as recently described (Heller et al. 2001). Experiments were performed according to the Declaration of Helsinki and were approved by the local research ethics committee. Cells were detached from umbilical veins with 0.01% collagenase and grown in M199 (Biochrom AG, Berlin, Germany) containing 17.5% FCS, 2.5% human serum, 680 μM l-glutamin, 25 μg/ml Heparin, 7.5 μg/ml endothelial mitogen (Hycultec GmbH, Beutelsbach, Germany) and 100 μM Vitamin C. For experiments, cells of the first and second passage were used.
Immunofluorescence
To visualise oncfFn and oncfTn-C variants, we used recombinant human biotinylated SIP-format antibodies: F8 recognising ED-A+ Fn (mouse and human), L19 targeting ED-B+ Fn (mouse and human), F16 against the A1-domain (human) and G11 recognising the C-domain (mouse and human) of Tn-C. They were detected applying the streptavidin and tyramide-Alexa488-based TSA Kit (Invitrogen GmbH, Darmstadt, Germany). Association of the matrix proteins to vascular structures in human tumours and xenografts was analysed by co-staining of the blood vessel specific antigen CD31 as recently described (Berndt et al. 2010).
To investigate the vascular deposition of F8 and F16 accessible antigen in relation to one another, an immunofluorescence triple staining was performed. The first SIP was detected by tyramide-Alexa488 signal amplification. The visualization of the second SIP antibody was done by Cy3-coupled streptavidin (Dianova GmbH, Hamburg, Germany). Then, for vessel staining, the CD31 antibody JC70A (DAKO Deutschland GmbH, Hamburg, Germany) and an Alexa633-conjugated goat-anti-mouse IgG (Dianova GmbH, Hamburg, Germany) was applied (detailed protocols are available on request).
For immunfluorescence analysis, the confocal laser scanning microscope LSM 510 (Carl Zeiss Jena GmbH, Jena, Germany) was used. The semiquantitative evaluation of vessels positive for oncfFn and oncfTn-C variants was performed using the following expression score examining the whole section: 0 = no staining of CD31 positive vessels, 1 = only few CD31 positive vessels are stained, 2 = about 50% of CD31 positive vessels are stained or heterogeneous staining pattern with the occurrence of completely detected vessels, and 3 = nearly all vessels are positive.
Stimulation experiments
To investigate the impact of RCC derived mediators on ED-A+-, ED-B+ Fn- and A1+ Tn-C mRNA expression in endothelial cells, HUVEC were stimulated with RCC-conditioned media generated under hypoxic conditions. For generation of RCC-conditioned media, cells were cultured 3 days in M199/0.05% HSA (Sigma-Aldrich Chemie GmbH, Munich, Germany) with 1% oxygen in a HERAcell 150i incubator (Thermo Fisher Scientific GmbH, Dreieich, Germany). Medium was collected, centrifuged at 2,000 rpm for 5 min and sterile filtered. Medium was kept at −20°C until use. After starvation of HUVEC in M199/0.05% HSA for 3 h, 500 μl of the hypoxic RCC-conditioned medium was added. To analyse the role of tumour-derived VEGF, 100 ng/ml of Avastin® (F. Hoffmann-La-Roche AG, Basel, Swizerland) was added. Stimulation was stopped for RNA isolation after 1, 5 or 16 h by adding the RLT buffer from RNeasy Mini Kit (Qiagen GmbH, Hilden, Germany). For control, cells were cultivated in starvation medium without additives. Experiments were performed in triplicate and results were given as mean value and standard error of mean.
RT-PCR
Total RNA was isolated from HUVEC using the RNeasy Mini Kit and oncfFn and oncfTn-C rtRT-PCR was performed using the QuantiTect SYBR® green one step rtRT-PCR Kit (both Qiagen GmbH, Hilden, Germany) on a iQ™5 cycler (Bio-Rad Laboratories GmbH, Munich, Germany). GAPDH served as housekeeping gene. Primers used were: ED-A+ Fn forward: 5′-GGAGAGAGTCAGCCTCTGGTTCAG-3′, ED-A+ Fn reverse: 5′-TCTGCAGTGTCTTCTTCACC-3′ (Mighell et al. 1997), ED-B+ Fn forward: 5′-TACCGCATCACAGTAGTTGC-3′, ED-B+ Fn reverse: 5′-CAGGTGACACGCATGGTGTCTGGA-3′ (Mighell et al. 1997), A1+ Tn-C forward: 5′-AGCTTCCAAGAAACACCACTTC-3′, A1+ Tn-C reverse: 5′-CCATCCCAGCCAACCTCA-3′, GAPDH forward: 5′-GGAGTCAACGGATTTGGT-3′, GAPDH reverse: 5′-GTGATGGGATTTCCATTGAT-3′ (Giannelli et al. 2005). Cycling conditions were: reverse transcription at 50°C for 30 min, followed by the initial PCR activating step at 95°C for 15 min, and 40 cycles of 94°C for 15 s, annealing for 30 s, 72°C for 40 s. Results were expressed as fold change of the non-stimulated controls (2−ΔΔCt/ΔΔCt data analysis method). Experiments were performed in triplicate and results were given as mean value and standard error of mean.
Results
Vascular expression of oncfFn and oncfTn-C variants in RCC subtypes
As shown by double immunofluorescence, there were remarkable differences in vessel associated oncfFn and oncfTn-C deposition between RCC subtypes. Within a large number of tumours of one subtype, the expression patterns are highly constant. The most consistent expression pattern could be revealed in ccRCC. ED-A+ and ED-B+ Fn as well as A1+ Tn-C were detectable in all specimens at high abundance around vascular structures. Vascular C+ Tn-C could never be shown (Figs. 1a–d, 2a). Figure 3a, b demonstrates ED-A+ Fn and A1+ Tn-c deposition in ccRCC on vascular level at higher magnification. In pRCC, ED-B+ Fn and ED-A+ Fn are only rarely expressed in blood vessels. In contrast, Tn-C isoforms are vascularly expressed at high level (Figs. 1e–h, 2b). In chRCC, only vascular ED-A+ Fn was regularly detectable at high abundance while ED-B+ Fn is present only rarely. Tn-C splice variants usually exist, but differ in quantity (Figs. 1i–l, 2c).
Immunofluorescence detection of oncofetal fibronectin and tenascin-C variants in clear cell RCC (a–d), papillary RCC (e–h), and chromophobe RCC (i–l) using the recombinant antibodies F8, L19, F16 and G11 (green oncofetal matrix proteins, red CD31). Histopathology is demonstrated in H&E stained corresponding frozen sections (m–o). (scale bars 100 μm)
Results of the semiquantitative evaluation of the vascular deposition of oncofetal fibronectin and tenascin-C variants in RCC subtypes a ccRCC (nine cases), b pRCC (ten cases), c chRCC (nine cases). Evaluation of the immunoreactive scores is explained in “Materials and methods”. IHC Immunohistochemistry
a, b Immunofluorescence double staining for CD31 (antibody JC70A, red) and for EDA+ Fn (antibody F8, green) (a) or for CD31 (antibody JC70A, red) and A1+ Tn-C (antibody F16, green) (b) in a representative ccRCC at higher magnification (nuclei stained with DAPI in blue, bars 100 μm). c, d Immunofluorescence triple staining for CD31 (blue), A1+ Tn-C (green) and EDA+ Fn (red) in ccRCC demonstrating a heterogeneous incorporation of EDA+ Fn and A1+ Tn-C in the vascular ECM (c) and vessel wall stratification with regard to these proteins (EDA+ Fn colocalized with endothelial cells, A1+ Tn-C deposited in the perivascular rim) (d) [scale bars 50 μm (c) and 20 μm (d)]
As demonstrated by JC70A/F8/F16 triple fluorescence staining, different vessel populations with respect to antigen expression are distinguishable (Fig. 3c): (1) vessels negative for both, (2) vessels showing only ED-A+ Fn or A1+ Tn-C, and (3) vessels showing both. Vessel walls positive for both oncfFn and oncfTn-C splice variants show a stratified patterning with F8 accessible antigen deposited in association to the endothelium and F16 accessible antigen being perivascularly organized (Fig. 3d).
Vascular expression of oncfFn and oncfTn-C variants in RCC primary tumours and corresponding metastases
In human RCC, there is an obvious correspondence in the vascular expression patterns when comparing primary tumours and metastases. As expected for ccRCC, F8, L19, and F16 accessible antigens are expressed in large amounts in primary tumours (Figs. 4a–d, 5) and, to a larger extend, also in metastases (Figs. 4e–h, 5).
Immunofluorescence detection of oncofetal fibronectin and tenascin-C variants in a human primary ccRCC (a–d) and its corresponding bone metastasis (e–h) as well as in a RXF393 orthotopic xenograft on nude mice (i–l) and its corresponding lung metastasis (m–p) (green oncofetal matrix proteins, red CD31; scale bars 100 μm)
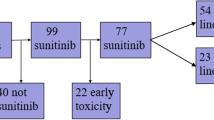
Results of the semiquantitative evaluation of the vascular deposition of oncofetal fibronectin and tenascin-C variants in primary RCC and their metastases. The graph presents the number of cases assigned to the different IHC scores. Evaluation of the immunoreactive scores is explained in “Materials and methods”. In general, there are comparable expression patterns in primary tumours and corresponding metastases. IHC immunohistochemistry
In the murine RCC, xenograft models a comparable vascular expression of the extra domains A and B of Fn and A1 of Tn-C could be shown using the antibodies F8, L19 and F16. Because the antibody F16 only detects human A1+ Tn-C, at least this Tn-C isoform must be derived from the carcinoma cells themselves. Also here, vascular expression patterns are the same in both primary tumours (Fig. 4i–l) and metastases with only quantitative differences (Fig. 4m–p).
Regulation of oncfFn and oncfTn-C mRNA expression in HUVEC by RCC-derived factors
To examine the relevance of RCC-derived factors for ED-A+-, ED-B+ Fn- and A1+-Tn-C mRNA expression in endothelial cells, stimulation of HUVEC with A498- and Caki1-conditioned media generated under hypoxic conditions was performed. Mutation analysis revealed the loss of one copy of the VHL gene in A498. Furthermore, a homozygous deletion of 4 bp (TGAC) in exon 2 was present which leads to a frame shift and therefore to a truncated VHL protein version with loss of function (confirmation of the results presented by Shinojima et al. 2007). In Caki1, only a homozygous substitution A > T in the 3′UTR was found and predicted to be a polymorphism (http://www.MutationTaster.org) with no alteration of protein function.
There is a general increase in ED-A+-, ED-B+ Fn- and A1+ Tn-C mRNA expression in HUVEC with the highest up regulation after 16 h independent of the medium used for stimulation. The up regulation after 16 h is up to twofold higher for A498 in comparison to Caki1-conditioned medium with a pronounced effect on A1+ Tn-C (Fig. 6a, c). The addition of the anti-VEGF antibody Avastin® to A498 medium completely blocked the stimulatory effect (Fig. 6b), while in case of Caki1 medium there was only a partial inhibition of oncfFn and oncfTn-C mRNA expression (Fig. 6d).
Changes in oncofetal fibronectin and tenascin-C mRNA expression in HUVEC due to 1, 5, and 16 h stimulation with A498 or Caki1-conditioned medium harvested under hypoxic conditions (a, c). Results are given as fold changes compared to unstimulated control. There is a general increase in mRNA expression in HUVEC after 16 h incubation with conditioned medium but showing quantitative and qualitative differences. The mRNA induction after application of A498 hypoxic medium is completely blocked by Avastin® (b) while there is only a partial reduction in case of Caki1 hypoxic medium (d). (experiments were performed in triplicate; white EDA+ Fn, grey EDB+ Fn, black A1+ Tn-C; error bars indicate standard error of the mean)
Discussion
Angiogenesis-related vascular matrix proteins are well established target structures for antibody based targeted pharmacodelivery (Neri and Bicknell 2005). As recently published, 15/18 (83%) of mRCC patients showed stable disease after two cycles of the antibody conjugate L19-IL2 targeting ED-B+ Fn with a median progression-free survival of 8 months (Johannsen et al. 2010). Furthermore, it could be shown that the immunocytokine F8-IL2 improves the therapeutic efficacy of Sunitinib in a RCC xenograft model (Frey et al. 2010). Therefore, knowledge on the differential vascular expression of the target proteins in RCC subtypes and metastases and their regulation could help stratify patients for targeted delivery therapy and is therefore of high clinical relevance.
Here we are able to demonstrate that the oncofFn and oncfTn-C vascular expression pattern differs in between different RCC subtypes, but profiles are highly consistent within a great number of tumours of the same subtype and when comparing primary tumours and the corresponding metastases. This finding could also be evidenced in mRCC xenograft models used for treatment experimental. The findings are very important for treatment strategy: systemic therapy for RCC patients is used in metastatic situation and is mainly directed against metastasis because nephrectomy is still standard of care. Metastases show the same vascular ECM structures, that is why vascular based targeted drug delivery in metastatic lesions might be individually adapted on the basis of the expression pattern in primary tumours.
All three subtypes show an abundant vascular deposition of ED-A+ Fn and A1+ Tn-C. In contrast ED-B+ Fn is detectable always in vessels supplying ccRCC tissue, sometimes in high amounts but less or even not at all in pRCC and chRCC vasculature. C+ Tn-C is only marginally expressed around RCC vessels, so targeting this isoform with the antibody G11 would not be effective in RCC therapy. These differences may be caused by tumour specific liberation of pro and/or anti angiogenic factors (Eble and Niland 2009; Saharinen et al. 2010). Indeed, RCC subtypes differ in their genetic background affecting the VEGF signalling pathway. A mutation affecting the VHL gene in a large portion of ccRCC and a resulting up regulation of HIF1 target genes is well-known (Brauch et al. 2000). In contrast, in pRCC there is an increase of onconeuronal cerebella degeneration-related antigen 2 (Cdr2) that leads to the suppression of HIF1 transcription activation (Balamurugan et al. 2009). With respect to this situation, it is necessary to carefully select patients for an antibody-based pharmacodelivery using the antibodies described here. Individual quantitative and qualitative differences in vascular ED-B+ Fn may also be a reason why only 15 out of 18 of the L19-IL12-treated patients with advanced RCC in the clinical trial reported by Johannsen et al. (2010) responded with a stabilisation of disease.
By fluorescence triple staining applying the clinically relevant antibodies F8 (ED-A+ Fn) and F16 (A1+ Tn-C), we are able to demonstrate an intratumoural heterogeneity of vasculature concerning oncfFn and oncfTn-C composition in ccRCC. This might reflect different states of vessel maturation or may be the result of a heterogenic distribution of growth factors and/or hypoxic areas. In line with this, a sequential occurrence of oncofFn isoforms, the generation of special fibronectin fragments as well as the fibronectin fibrillogenesis are important for the regulation of endothelial cell proliferation, recruitment of pericytes as well as vascular smooth muscle cells and thereby for the establishment of a functional vascular system during embryogenesis or wound healing processes (Astrof and Hynes 2009; Zhou et al. 2008). For oncTn-C variants, a migration promoting role could be shown for endothelial cells during processes of tissue remodelling (Zagzag et al. 2002; Ballard et al. 2006; Orend and Chiquet-Ehrismann 2006). In that context, the process of alternative splicing of Tn-C is of functional importance since different splicing domains could be shown to induce different effects: a angiogenesis promoting role for the fibrinogen-homologue globular domain and a angiogenesis inhibiting role for the A2 domain (Schenk et al. 1999; Saito et al. 2008).
Stable expression pattern of vascular oncfFn and oncfTn-C on one hand and the occurrence of different vessel subpopulations on the other hand lead to the suggestion that a combination of oncfFn and oncfTn-C targeting antibodies may improve the therapeutic efficacy. Furthermore, as already demonstrated by a combination of a recombinant SIP antibody and a monoclonal antibody (Berndt et al. 2010), a stratified organization of the vascular ECM concerning oncfFn and oncfTn-C targetable antigens could also be evidenced by use of two “therapeutic” SIP format antibodies. Thus, it might be possible to specifically attack endothelial cells via intraluminal targeting of oncFn and perivascular cells such as pericytes and myofibroblasts by targeting of oncTnC alone or in combination.
In vitro, we are able to show that indeed oncfFn and oncfTn-C mRNA expression in endothelial cells are up-regulated by RCC-conditioned medium. This effect is more pronounced using conditioned medium of A498 cells with a VHL loss of function mutation in comparison to Caki1-conditioned medium. This difference could be explained by the known overexpression of VEGF in A498 cells. The prominent role of VEGF is also supported by the fact that mRNA expression is completely blocked by Avastin® when added to A498-conditioned medium. In contrast, in case of Caki1-conditioned medium there is only a partial inhibition of mRNA synthesis by Avastin® indicating an additional role of further angiogenesis related cytokines in ECM protein regulation which must be the object of further studies. These differences in the cytokine spectrum of both cell lines may also be the reason for varying mRNA expression patterns supporting the in vivo results of different but stable immunohistochemical expression pattern in RCC subtypes. A comparable impact of the VEGF/VEGFR system on the expression of ED-B+ Fn expression could recently be evidenced in a human endometrial adenocarcinoma xenograft model (Coltrini et al. 2009). In any case, the relevance of VEGF in the up regulation of potential target structures should be taken into consideration if anti-VEGF therapy and targeted drug delivery on the basis of vascular matrix proteins are combined.
References
Astrof S, Hynes RO (2009) Fibronectins in vascular morphogenesis. Angiogenesis 12:165–175
Balamurugan K, Luu VD, Kaufmann MR, Hofmann VS, Boysen G, Barth S, Bordoli MR, Stiehl DP, Moch H, Schraml P, Wenger RH, Camenisch G (2009) Onconeuronal cerebellar degeneration-related antigen, Cdr2, is strongly expressed in papillary renal cell carcinoma and leads to attenuated hypoxic response. Oncog ene. 28:3274–3285
Ballard VL, Sharma A, Duignan I, Holm JM, Chin A, Choi R, Hajjar KA, Wong SC, Edelberg JM (2006) Vascular tenascin-C regulates cardiac endothelial phenotype and neovascularization. FASEB J 20:717–719
Berndt A, Anger K, Richter P, Borsi L, Brack S, Silacci M, Franz M, Wunderlich H, Gajda M, Zardi L, Neri D, Kosmehl H (2006) Differential expression of tenascin-C splicing domains in urothelial carcinomas of the urinary bladder. J Cancer Res Clin Oncol 132:537–546
Berndt A, Köllner R, Richter P, Franz M, Voigt A, Berndt A, Borsi L, Giavazzi R, Neri D, Kosmehl H (2010) A comparative analysis of oncofetal fibronectin and tenascin-C incorporation in tumour vessels using human recombinant SIP format antibodies. Histochem Cell Biol 133:467–475
Borsi L, Carnemolla B, Nicolò G, Spina B, Tanara G, Zardi L (1992) Expression of different tenascin isoforms in normal, hyperplastic and neoplastic human breast tissues. Int J Cancer 52:688–692
Brack SS, Silacci M, Birchler M, Neri D (2006) Tumor-targeting properties of novel antibodies specific to the large isoform of tenascin-C. Clin Cancer Res 12:3200–3208
Brauch H, Weirich G, Brieger J, Glavac D, Rödl H, Eichinger M, Feurer M, Weidt E, Puranakanitstha C, Neuhaus C, Pomer S, Brenner W, Schirmacher P, Störkel S, Rotter M, Masera A, Gugeler N, Decker HJ (2000) VHL alterations in human clear cell renal cell carcinoma: association with advanced tumor stage and a novel hot spot mutation. Cancer Res 60:1942–1948
Carnemolla B, Borsi L, Balza E, Castellani P, Meazza R, Berndt A, Ferrini S, Kosmehl H, Neri D, Zardi L (2002) Enhancement of the antitumor properties of interleukin-2 by its targeted delivery to the tumor blood vessel extracellular matrix. Blood 99:1659–1665
Coltrini D, Ronca R, Belleri M, Zardi L, Indraccolo S, Scarlato V, Giavazzi R, Presta M (2009) Impact of VEGF-dependent tumour micro-environment on EDB fibronectin expression by subcutaneous human tumour xenografts in nude mice. J Pathol 219:455–462
Eble JA, Niland S (2009) The extracellular matrix of blood vessels. Curr Pharm Des 15:1385–1400
Frey K, Schliemann C, Schwager K, Giavazzi R, Johannsen M, Neri D (2010) The immunocytokine F8-IL2 improves the therapeutic performance of sunitinib in a mouse model of renal cell carcinoma. J Urol 184:2540–2548
Giannelli G, Bergamini C, Fransvea E, Sgarra C, Antonaci S (2005) Laminin-5 with transforming growth factor-beta1 induces epithelial to mesenchymal transition in hepatocellular carcinoma. Gastroenterology 129:1375–1383
Heller R, Unbehaun A, Schellenberg B, Mayer B, Werner-Felmayer G, Werner ER (2001) l-ascorbic acid potentiates endothelial nitric oxide synthesis via a chemical stabilization of tetrahydrobiopterin. J Biol Chem 276:40–47
Hindermann W, Berndt A, Borsi L, Luo X, Hyckel P, Katenkamp D, Kosmehl H (1999) Synthesis and protein distribution of the unspliced large tenascin-C isoform in oral squamous cell carcinoma. J Pathol 189:475–480
Johannsen M, Spitaleri G, Curigliano G, Roigas J, Weikert S, Kempkensteffen C, Roemer A, Kloeters C, Rogalla P, Pecher G, Miller K, Berndt A, Kosmehl H, Trachsel E, Kaspar M, Lovato V, González-Iglesias R, Giovannoni L, Menssen HD, Neri D, de Braud F (2010) The tumour-targeting human L19-IL2 immunocytokine: preclinical safety studies, phase I clinical trial in patients with solid tumours and expansion into patients with advanced renal cell carcinoma. Eur J Cancer 46:2926–2935
Mårlind J, Kaspar M, Trachsel E, Sommavilla R, Hindle S, Bacci C, Giovannoni L, Neri D (2008) Antibody-mediated delivery of interleukin-2 to the stroma of breast cancer strongly enhances the potency of chemotherapy. Clin Cancer Res 14:6515–6524
Mighell AJ, Thompson J, Hume WJ, Markham AF, Robinson PA (1997) RT-PCR investigation of fibronectin mRNA isoforms in malignant, normal and reactive oral mucosa. Oral Oncol 33:155–162
Naito S, von Eschenbach AC, Giavazzi R, Fidler IJ (1986) Growth and metastasis of tumor cells isolated from a human renal cell carcinoma implanted into different organs of nude mice. Cancer Res 46:4109–4115
Neri D, Bicknell R (2005) Tumour vascular targeting. Nat Rev Cancer 5:436–446
Orend G, Chiquet-Ehrismann R (2006) Tenascin-C induced signaling in cancer. Cancer Lett 244:143–163
Pedretti M, Verpelli C, Mårlind J, Bertani G, Sala C, Neri D, Bello L (2010) Combination of temozolomide with immunocytokine F16-IL2 for the treatment of glioblastoma. Br J Cancer 103:827–836
Saharinen P, Bry M, Alitalo K (2010) How do angiopoietins Tie in with vascular endothelial growth factors? Curr Opin Hematol 17:198–205
Saito Y, Shiota Y, Nishisaka M, Owaki T, Shimamura M, Fukai F (2008) Inhibition of angiogenesis by a tenascin-C peptide which is capable of activating beta1-integrins. Biol Pharm Bull 31:1003–1007
Santimaria M, Moscatelli G, Viale GL, Giovannoni L, Neri G, Viti F, Leprini A, Borsi L, Castellani P, Zardi L, Neri D, Riva P (2003) Immunoscintigraphic detection of the ED-B domain of fibronectin, a marker of angiogenesis, in patients with cancer. Clin Cancer Res 9:571–579
Schenk S, Chiquet-Ehrismann R, Battegay EJ (1999) The fibrinogen globe of tenascin-C promotes basic fibroblast growth factor-induced endothelial cell elongation. Mol Biol Cell 10:2933–2943
Schliemann C, Neri D (2010) Antibody-based vascular tumor targeting. Recent Results Cancer Res 180:201–216
Schwarzbauer JE (1991) Alternative splicing of fibronectin: three variants, three functions. Bioessays 13:527–533
Shinojima T, Oya M, Takayanagi A, Mizuno R, Shimizu N, Murai M (2007) Renal cancer cells lacking hypoxia inducible factor (HIF)-1alpha expression maintain vascular endothelial growth factor expression through HIF-2alpha. Carcinogenesis 28:529–536
Silacci M, Brack SS, Späth N, Buck A, Hillinger S, Arni S, Weder W, Zardi L, Neri D (2006) Human monoclonal antibodies to domain C of tenascin-C selectively target solid tumors in vivo. Protein Eng Des Sel 19:471–478
Tong AL, Zeng ZP, Li HZ, Yang D, Lu L, Li M, Zhou YR, Zhang J, Chen S, Liang W (2006) von Hippel-Lindau gene mutation in non-syndromic familial pheochromocytomas. Ann N Y Acad Sci 1073:203–207
Villa A, Trachsel E, Kaspar M, Schliemann C, Sommavilla R, Rybak JN, Rösli C, Borsi L, Neri D (2008) A high-affinity human monoclonal antibody specific to the alternatively spliced EDA domain of fibronectin efficiently targets tumor neo-vasculature in vivo. Int J Cancer 122:2405–2413
von Lukowicz T, Silacci M, Wyss MT, Trachsel E, Lohmann C, Buck A, Lüscher TF, Neri D, Matter CM (2007) Human antibody against C domain of tenascin-C visualizes murine atherosclerotic plaques ex vivo. J Nucl Med 48:582–587
Zagzag D, Shiff B, Jallo GI, Greco MA, Blanco C, Cohen H, Hukin J, Allen JC, Friedlander DR (2002) Tenascin-C promotes microvascular cell migration and phosphorylation of focal adhesion kinase. Cancer Res 62:2660–2668
Zhou X, Rowe RG, Hiraoka N, George JP, Wirtz D, Mosher DF, Virtanen I, Chernousov MA, Weiss SJ (2008) Fibronectin fibrillogenesis regulates three-dimensional neovessel formation. Genes Dev 22:1231–1243
Acknowledgments
The authors are grateful to Claudia Seliger, Beate Ziegenhardt, Valentina Scarlato and Elke Teuscher for excellent technical assistance. The research leading to the results has received funding from the European Community’s Seventh Framework Programme (FP7/2007-2013) under grant agreement no Health-F2-2008-201342 (ADAMANT).
Conflict of interest
Dario Neri is a co-founder and shareholder of Philogen, the company which owns the rights over the F8, L19, F16 and G11 antibodies.
Author information
Authors and Affiliations
Corresponding author
Additional information
K. Galler and K. Junker contributed equally to the study.
Rights and permissions
About this article
Cite this article
Galler, K., Junker, K., Franz, M. et al. Differential vascular expression and regulation of oncofetal tenascin-C and fibronectin variants in renal cell carcinoma (RCC): implications for an individualized angiogenesis-related targeted drug delivery. Histochem Cell Biol 137, 195–204 (2012). https://doi.org/10.1007/s00418-011-0886-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00418-011-0886-z









