Abstract
Gene therapy trials for heart failure have demonstrated the key role of efficient gene transfer in achieving therapeutic efficacy. An attractive approach to improve adenoviral gene transfer is to use alternative virus serotypes with modified tropism. We performed a detailed analysis of cardiac expression of receptors for several adenovirus serotypes with a focus on differential expression of CAR and CD46, as adenoviruses targeting these receptors have been used in various applications. Explanted hearts from patients with DCM and healthy donors were analyzed using Q-RT-PCR, western blot and immunohistochemistry. Q-RT-PCR and Western analyses revealed robust expression of all receptors except CD80 in normal hearts with lower expression levels in DCM. Immunohistochemical analyses demonstrated that CD46 expression was somewhat higher than CAR both in normal and DCM hearts with highest levels of expression in intramyocardial coronary vessels. Total CAR expression was upregulated in DCM. Triple staining on these vessels demonstrated that both CAR and CD46 were confined to the subendothelial layer in normal hearts. The situation was clearly different in DCM, where both CAR and CD46 were expressed by endothelial cells. The induction of expression of CAR and CD46 by endothelial cells in DCM suggests that viruses targeting these receptors could more easily gain entry to heart cells after intravascular administration. This finding thus has potential implications for the development of targeted gene therapy for heart failure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite significant advances in prevention and treatment strategies, cardiovascular disease remains the leading cause of death in the Western world, underscoring the need to develop novel therapeutic modalities. This is especially true for end-stage heart failure, which is primarily caused by ischemic or dilated cardiomyopathy (DCM), as it carries a dismal prognosis and current therapeutic options are clearly limited. Various preclinical gene therapy strategies have been developed for heart failure and therapeutic approaches have included many viral vectors and non-viral gene transfer and various modes of administration (reviewed in Rissanen and Yla-Herttuala 2007). Most clinical gene therapy trials to date have focused on the promotion of therapeutic angiogenesis, and one of the lessons from these trials has been the key role of efficient gene delivery in achieving clinically meaningful therapeutic efficacy.
Despite the emergence of adeno-associated virus as a promising vector for cardiovascular gene therapy, adenovirus (Ad) has thus far been the vector of choice in most cardiovascular gene therapy trials. The advantages of Ad include easy production in high titers and the ability to rapidly induce high levels of transgene expression. Although considered rather immunogenic, optimal low doses induce little inflammation in skeletal muscle and myocardium (reviewed in Rissanen and Yla-Herttuala 2007). However, the ability of the standard serotype 5 Ad to transduce many important gene therapy targets is limited (Asaoka et al. 2000; Havenga et al. 2002; Zeimet et al. 2002). In many cases, this has been shown to be caused by low expression levels of the coxsackie and adenovirus receptor (CAR) on target cells (Hemmi et al. 1998; Li et al. 1999). Redirecting Ad vectors to other, preferentially target-specific cellular receptors has thus become a major goal in gene therapy.
Several strategies have been employed to target the adenovirus (Einfeld et al. 2001; Kasono et al. 1999; Nettelbeck et al. 2001; Wickham et al. 1996). The hybrid virus approach utilizes the fact that native Ads have different tissue tropisms and hybrid Ads have been constructed by swapping the fiber gene from one serotype to that of another. Fibers from serotypes 3 and 35 are among the most widely used for this purpose. Serotype 3 uses CD46, CD80 and CD86, and serotype 35 CD46 as their primary cellular receptors (Gaggar et al. 2003; Short et al. 2004). Extensive data demonstrate that both serotypes are able to efficiently transduce many cell types that are relatively resistant to Ad5 infection, including hematopoetic stem cells, tumor endothelial cells, and several cancer cell types (Amin 2003; Kanerva et al. 2002; Segerman et al. 2000; Shayakhmetov et al. 2002; Shinozaki et al. 2006; Sova et al. 2004; Suominen et al. 2006).
Despite growing interest in developing targeted gene therapy vectors for cardiovascular disease, there is only limited data on the expression of Ad receptors in the heart. Most studies have concentrated on CAR (Fechner et al. 2003; Noutsias et al. 2001), and to our knowledge detailed expression analysis of the other Ad receptors in the heart has not previously been reported. In this study we have analyzed the expression of Ad receptors in normal and DCM hearts with the purpose of providing data for rational design of targeted gene therapy for heart failure.
Materials and methods
Samples
Failing left ventricles were harvested at the time of cardiac transplantation from seven patients with end-stage heart failure (New York Heart Association functional class IV) due to idiopathic DCM (n = 7) at the University Central Hospital, Helsinki, Finland. Normal heart samples (n = 7) were obtained from left ventricles of organ donors who had no history of cardiac disease and whose donated heart could not be used for transplantation. The cause of death in these subjects was either subarachnoid or intracerebral hemorrhage. The clinical characteristics of the patients in this study are shown in Table 1. After excision, the heart tissues were immediately frozen in liquid nitrogen and stored at −70°C. An institutional review board approved the use of normal and failing human heart samples, and the investigation conforms to the principles outlined in the Declaration of Helsinki.
Protein lysates were prepared from frozen tissue samples. Pieces of tissue were first homogenized by grinding in liquid nitrogen. The powdered tissue was suspended in 10 μl of RIPA lysis buffer (150 mM NaCl, 50 mM Tris–HCl, 1% Triton-X, 0.1% SDS, 0.5% Na-deoxycholate) per 1 mg tissue. The solution was pressed ten times through a 21-G needle and ten times through an 18-G needle. Homogenate was mixed in rotamix for 30 min at 4°C before centrifugation 4 min 5,000 rpm at 4°C. The pellet was discarded and supernatant was stored at −20°C for later use. Total RNA was extracted from cardiac tissue samples similarly. Nucleospin RNA II kit (Macherey–Nagel, Germany) was used for RNA purification. RNA concentrations were measured with NanoDrop spectrophotometer (Thermo Scientific, USA).
Quantitative reverse transcriptase PCR
The purified RNA was reverse transcribed to cDNA with Superscript II reverse transcriptase (Invitrogen, USA) according to the manufacturer’s instructions. For RT-PCR reactions 2× Taqman universal mastermix (Applied Biosystems, USA) was used. Receptor specific primers (CAR forward: ATGAAAAGGAAGTTCATCACGATA reverse: AATGATTACTGCCGATGTAGCTT CD46 forward: TGACAATTCAGTGTG GAGTCG CD46 reverse: TGGAAATCGACATTTGACCA CD80 forward: CATGTTACTCATGACTCC CD80 reverse: GTTGCGTCCACTTCTGGTCT CD86 forward: CAAGACGCGGCTTTTATCTT CD86 reverse: ATCCAAGGAATGTGGTCTGG, and αv integrin forward: TTATACAATTTTACTGGCGAGCAG αv integrin reverse: ACACATCTGCATAATCATCTCCA) and universal probe library probes (Roche, Switzerland) were added to this mixture. Reaction concentration was 3 μM for primers and 2 μM for probes. Eight microliters of this mastermix was applied to each well. Two microliters of cDNA solution was used as template. Standard curves were run on the same plate as the corresponding receptor reactions and all reactions were done in quadruplicates. RT-PCR runs were performed in the Turku Centre for Biotechnology core facility.
Western blot
Receptors CD80, CD86, and β-actin were run under denaturing conditions. In the denaturing assay, the samples were first boiled 5 min at 95°C and then loaded on 10% Bis–TRIS Criterion precast gels (Biorad, USA). Samples were run in MOPS buffer (Biorad, USA) for 50 min 200 V. Run samples were transferred onto PVDF membranes 1 h 400 mA. The membranes were blocked with 5% milk in PBST and incubated overnight at 4°C in 2 ml of antibody working dilution [CD80 0.5 μg/ml (clone 2D10, Abcam, UK) CD86 1:5,000 (concentration n/a) (clone 2F7, Abcam, UK) β-actin 0.85 μg/ml (clone AC-74, Sigma–Aldrich, USA)]. Horseradish peroxidase conjugated goat anti-mouse antibody (Dako, Denmark) (0.1 μg/ml working dilution) was added onto the membranes and incubated for 1 h at RT. Light reaction was initiated by adding 4 ml ECL mix onto the membranes and incubated 2 min at RT and X-ray film was exposed to the light reaction in the dark. Non-reducing conditions were used for CAR (5 μg/ml antibody dilution, clone RmcB, Upstate, USA), CD46 (1 μg/ml antibody dilution, clone MEM-258, Biolegend, USA) Hsc70 (1:5,000 antibody dilution (concentration N/A), and clone SPA-815, StressGen Biotechnologies, Canada). αv integrin (1:500 antibody dilution (concentration n/a), L230 conditioned medium collected from ATCC HB-8448 hybridoma cell line) was run in a native western assay. Non-reducing western blot was done as normal western described above, except the samples were diluted in non-reducing sample buffer and instead of boiling the samples, the samples were incubated at 37°C for 10 min before loading to gel. Native western blot was done the same way except that the 6% gel was cast without detergents [lower gel: 5 ml separating buffer (1.5 M Tris–HCl, pH8.8), 10.9 ml H2O, 4 ml 30% acrylamide, 100 μl APS (10% ammoniumpersulphate), 10 μl TEMED. Upper gel: 2.5 ml stacking buffer (0.5 M Tris–HCl, pH 6.8), 5.7 ml H2O, 1.7 ml 30% acrylamide, 90 μl APS, 10 μl TEMED]. The samples were not boiled prior to loading, but incubated at 37°C for 10 min and the gel was run under non-reducing conditions (running buffer: 25 mM Tris, 192 mM glycine, in H2O, pH 8.8). The intensities of specific bands on films were quantified using a CCD-camera. The signals were normalized to total loaded protein stained with Coomassie blue (Online resource 1).
Immunohistochemistry
Frozen sections from diseased and normal cardiac tissue samples were stained with Vectastain HRP-kit (Vector laboratories, USA). Five-micrometer tissue sections were cut from the frozen human heart samples. The sections were fixed onto Superfrost plus slides (O. Kindler GmbH, Germany) with cold acetone. The endogenous peroxidase was inactivated with 0.3% H2O2. Primary antibody working dilution [anti-CAR 5 μg/ml (clone RmcB, Upstate, USA), anti-CD46 0.5 μg/ml (clone MEM-258, Biolegend, USA), anti-CD80 0.5 μg/ml (clone 2D10, Abcam, USA), anti-CD86 1:250 (concentration n/a, clone EP1158Y, Abcam, USA), or anti-αv integrin 1:2,000 (L230 conditioned medium collected from ATCC HB-8448 hybridoma cell line)] was applied on the sections encircled with PapPen (Daido Sangyo, Japan). Vectastain ABC-reagent was applied on the sections (Vector Laboratories, USA) and receptors were stained with diaminobenzidine (DAB, Sigma–Aldrich, USA) and counterstained with Mayer’s hematoxylin (Sigma–Aldrich, USA). Frozen sections prepared from cardiac tissue samples were also triple stained with fluorescent labels. Five-micrometer sections were fixed onto Superfrost plus microscopic slides with cold acetone. The first primary antibody, anti-CD31 (1:200 dilution in 1% BSA-PBST, concentration n/a) was applied onto the sections and incubated for 1 h at RT in humid chamber. Cy3-labeled goat anti-mouse secondary antibody (1 μg/ml) was used to label first primary antibody binding. The second primary antibody anti-αv integrin (1:2,000 dilution) was applied onto the sections and incubated overnight at +4°C in humid chamber in the dark. Cy5-labeled goat anti-mouse secondary antibody (1 μg/ml) was used to label second primary antibody binding. The third primary antibody (anti-CAR 5 μg/ml or anti-CD46 0.5 μg/ml), applied onto the sections and incubated overnight at +4°C in humid chamber in the dark Cy2-labeled goat anti-mouse secondary antibody (1 μg/ml) was used to label third primary antibody binding. The sections were counterstained with Hoechst for 5 min RT in the dark.
IHC stained sections were photographed using a microscope and quantified using a CCD camera. Color intensity per area was measured from intact areas of each sample including as much of the sample as possible. Background signal was measured from each slide from an area with no sample and subtracted from the section signal before calculation of mean values for normal and DCM groups. IF stained sections were photographed using a confocal microscope. The receptor-specific areas were evaluated using ImageJ software (National Institutes of Health, Maryland, USA). To eliminate the variation in vein size a region of interest (ROI) was set to each picture. The ROI covered 25 × 50 pixels for endothelium and was aligned to include part of lumen. For subendothelial layer ROI covered 70 × 50 pixels and was aligned to include the subendothelial layer of the vein. CD31-expressing areas in DCM samples was only 14.6% smaller than in non-DCM samples (p = 0.179, data not shown) indicating constant amount of endothelium included in ROI. For three out of seven samples in both groups the image quality was not sufficient to allow for reliable quantification.
Statistical analysis
To determine statistical significance, we used Microsoft Excel software and Student’s t test analysis. p Values < 0.05 were considered statistically significant.
Results
Q-RT-PCR
The clinical characteristics of the patients used in this study are summarized in Table 1. Adenoviral receptor mRNA expression was evaluated with quantitative real-time PCR (Fig. 1). High mRNA levels were detected for CAR, CD46, and CD86. αv integrin mRNA expression was somewhat lower despite high protein expression suggesting slower protein turnover. CD80 expression was 14 to 15 orders of magnitude lower than the expression of other receptors and barely detectable. Expression of CAR was observed to be upregulated in cardiomyopathy 2.5 fold when compared to normal cardiac tissue. In contrast, CD46, CD86, and αv integrin mRNA levels were 1.9, 1.7, and 4.2 fold lower in DCM, respectively. CAR mRNA was 1.8 and 8.5 times more abundant than CD46 mRNA in normal and DCM samples, respectively, indicating that CAR is more prevalent in cardiac tissue than CD46, and this difference increases significantly after alterations in cardiac morphology.
Q-RT-PCR analysis of adenoviral receptors on heart tissue samples. A piece of heart tissue was excised and weighted and total RNA was extracted and purified. Gene copy numbers were normalized to the weight of tissue at the start of RNA purification. For both normal and DCM groups n = 7. Student’s t test was performed to evaluate the significance of group differences, and p value < 0.05 was considered statistically significant. No statistical significance was seen between non-DCM and DCM groups. Error bars show the standard error of the mean
Western analysis
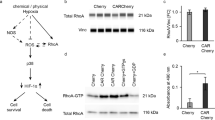
Western analysis was used to analyze the total protein levels of adenoviral receptors in normal and DCM samples (Fig. 2). Due to variation in the expression levels of housekeeping genes β-actin and Hsc70, total loaded protein was used as a loading control. Due to differences in primary antibody affinities for their respective antigens, we cannot make direct comparisons of the expression levels between different receptors. Robust receptor expression was detected for all adenoviral receptors except CD80 in both normal and DCM samples. Quantification of band intensities showed that CD46 and αv integrin were expressed at slightly lower levels in DCM samples, but the differences were not statistically significant. CAR, CD80, and CD86 expressions were upregulated in DCM 2.6, 1.9, and 1.8 fold, respectively. The difference in CAR expression was found to be statistically significant (p = 0.013). It must also be noted that total expression levels for CD80 were very low.
Western blot analysis of receptor expression. Protein preparations purified from tissue samples were run on PAGE gels and labeled with monoclonal receptor specific antibodies (a). Band intensities were measured with CCD-camera and normalized to total protein stained with Coomassie blue and the average signal intensities were compared between non-DCM and DCM groups (b). Students t test was performed to evaluate the significance of group differences (*p < 0.05, **p < 0.01). Error bars show the standard error of the mean
Immunohistochemistry and immunofluorescence
All human cardiac samples were also stained with standard IHC methods with receptor specific antibodies (Fig. 3). CAR was expressed throughout the myocardium in both normal and DCM hearts. CD46 was also ubiquitously expressed in the myocardium in both groups with highest levels of expression in intramyocardial coronary vessel walls. CD86 was expressed in a similar pattern as CD46, but at clearly lower levels. αv integrin was expressed strongly in both normal and DCM groups with highest levels of expression in intramyocardial coronary vessels. CD80 expression was close to background in both groups.
We further characterized the IHC expressions by quantifying stained sections with CCD-camera and measuring color intensity per area (Fig. 4). CD80 and CD86 stainings gave low intensities and were excluded from this analysis. No statistically significant changes in expression levels between normal and DCM samples were observed for CAR, CD46, and αv integrin. Although direct comparisons cannot be made between different antibodies, CD46 was expressed more widely than CAR.
Quantification of immunohistochemistry stainings. Cryosections stained with receptor-specific monoclonal antibodies were photographed and color formation was quantified using a CCD camera measuring color intensity per area. Student’s t test was performed to evaluate the significance of group differences and p value < 0.05 was considered statistically significant. No statistical significance was seen between non-DCM and DCM groups. Error bars show the standard error of the mean (n = 7 DCM, n = 7 non-DCM)
In order to characterize in detail the expression patterns of the receptors in intramyocardial coronary vessels, triple staining immunofluorescence approach was used to evaluate the colocalization of adenoviral receptors with the endothelial marker CD31 (Fig. 5). Interestingly, we saw the primary receptors CAR and CD46 to be localized to the media of intramyocardial coronary vessels in normal samples while αv integrin was co-localized with the CD31-expressing endothelial cells in the luminal surface of intramyocardial coronary vessels. In contrast, in DCM samples CAR and CD46 were co-localized with αv integrin and CD31, showing differential expression patterns between normal and diseased heart tissue. This phenomenon was observed in all 14 samples. Quantification of the data revealed that CAR expression was 7.0 (p = 0.0004) and CD46 expression 7.1 (p = 0.0037) times higher in endothelium in DCM when compared with normal samples (Fig. 6), whereas in the subendothelial layer CAR expression was 16.7 (p = 0.002) and CD46 expression 24.4 (p = 0.001) times higher in normal heart samples when compared with DCM samples, indicating clearly different receptor patterns between the DCM and non-DCM groups (Fig. 6).
Immunofluorescence staining of heart sections. Frozen sections were triple stained using receptor specific monoclonal antibodies for CAR + αv integrin + CD31 (a) or CD46 + αv integrin + CD31 (b) and photographed using a confocal microscope. Representative results are shown (n = 7 DCM, n = 7 non-DCM). L lumen, E endothelium
Quantification of immunofluorescence stainings. CAR (a) and CD46 (b) expression profiles were quantified separately for the endothelial (EC) and subendothelial (SEC) layers. Positive areas (px2) were evaluated using ImageJ software. Region of interest was chosen from each section and positioned to include either the endothelium or the subendothelial layer. Students t test was performed to evaluate the significance of group differences (*p < 0.05, **p < 0.01). Error bars show the standard error of the mean (n = 4 DCM, n = 4 non-DCM)
Discussion
In this paper, we set out to investigate the expression patterns of known adenoviral receptors in normal and DCM human hearts. Our analysis focused on two distinct issues related to the development of novel adenovirus-based gene therapy approaches. First, what are the differences in expression patterns between different Ad receptors? Second, what effect does heart failure have on the expression of these receptors? We especially wanted to focus on comparing the expression patterns of CAR and CD46 as viruses attaching to these receptors have been extensively compared in many non-cardiovascular applications. It has been shown previously that one of the most critical issues for efficient adenovirus-based gene therapy is the adequate expression of virus receptor on the target tissue. For example, Douglas et al. (2001) have demonstrated that the level of CAR receptor expression crucially affects the anti-tumor efficacy of adenoviral therapy in a mouse glioma model. Our previous studies show significant decrease in infection efficiencies of head and neck cancer cells with lower CAR expression levels (Suominen et al. 2006). For the heart such studies have not thus far been carried out, but Cirielli et al. (2004) have demonstrated that adenoviral vectors binding to αV integrin exhibit superior transgene delivery capacity than vectors binding to heparin sulfate after intramuscular injection.
Our results demonstrate robust CAR mRNA and protein expression both in normal and DCM hearts. Previously published data have demonstrated CAR receptor expression to be upregulated in DCM 12 to 34-fold in comparison with normal cardiac tissue, although expression levels were highly variable between samples (Noutsias et al. 2001; Sasse et al. 2003). We saw small differences in CAR expression levels between normal and DCM hearts with minor in-group variation. Adenovirus genomes have been detected in DCM samples and enhanced CAR expression in DCM has been suggested to play a role in the pathogenesis of this disease, but no direct causal link has thus far been established (Kuhl et al. 2005). It has previously been reported that in DCM, CAR is localized to the cardiomyocyte sarcolemma and intercalated disks (Noutsias et al. 2001). Our results demonstrate a clear difference between normal and DCM hearts, as in the normal heart CAR expression is confined to the subendothelial layer of intramyocardial coronary vessels, whereas in DCM, CAR expression is concentrated in CD31 + endothelial cell layer and colocalized with αv integrin expression (Fig. 5). Quantification of this data demonstrated that it is clearly statistically significant (Fig. 6). Similar induction of CAR expression by endothelial cells has previously been demonstrated in the infarct zone of experimental rat myocardial infarction (Fechner et al. 2003). In addition, as CAR exhibits properties of a cell adhesion molecule (CAM), it is interesting to note that several CAMs have also shown to be expressed by endothelial cells in DCM (Noutsias et al. 1999). Various cancer studies report decreased CAR expression in advanced stages of the disease, but have not demonstrated any correlation with age or sex of the patient (Giaginis et al. 2008; Matsumoto et al. 2005; Rauen et al. 2002). Similarly, we did not find any statistical correlation between adenovirus receptor expression and age or sex of the patient or the drug therapy used.
CD46 is a complement regulatory protein with multiple isoforms which is expressed by many cell types in humans (Seya et al. 1999). In addition to being a receptor for group B adenoviruses, CD46 has previously been described also as a cellular receptor for both measles virus and human herpes virus 6 (Dorig et al. 1993; Santoro et al. 1999). The hybrid Ad5/35 virus targeting CD46 has been widely used in many non-cardiovascular gene therapy applications where it has been shown to be superior to standard Ad5 in transducing many cell types. In mature skeletal muscle, CD46 has been detected at extremely low levels with highest levels of expression on blood vessels (Larochelle et al. 2008). However, there is scarce previous data on CD46 expression in healthy or diseased heart. We show here robust CD46 expression at levels comparable to CAR with highest levels of expression in intramyocardial coronary vessels. Similar to CAR, normal and DCM hearts express CD46 at roughly the same levels. Interestingly, we also observed the same phenomenon of induction of endothelial CD46 expression in DCM (Fig. 5).
CD80 and CD86 (also known as B7-1 and B7-2) are B-cell receptors, which are present also in other antigen presenting cells. These receptors act as costimulatory molecules that bind T-cell receptors CD28 and CTLA-4 (van der Merwe et al. 1997). CD80 and CD86 have been shown to mediate Ad3 cellular attachment (Short et al. 2004). We found barely detectable CD80 mRNA or protein expression levels in normal and DCM hearts. Previously, similar results have been obtained using Q-RT-PCR (Akdere et al. 2005). In contrast, CD86 was expressed at robust levels in both normal and DCM hearts as demonstrated by western blotting and Q-RT-PCR. However, immunohistochemistry demonstrated only low level of staining with no concentration of expression in intramyocardial coronary vessels as with CAR and CD46 (Fig. 3). We could not exclude technical or antibody-related problems as a reason for this observation.
αvβ3 and αvβ5 integrins interact with the penton base structure in the adenovirus capsid and are responsible for adenovirus internalization (Wickham et al. 1993). They are widely expressed by many cell types, including endothelial and smooth muscle cells (Cheresh1987; Janat et al. 1992) and are upregulated in hypoxia and angiogenesis (Brooks et al. 1994; Kalinowski et al. 2008). Our data demonstrate high αv integrin protein expression with strong immunohistochemistry signal in intramyocardial coronary vessels. Triple stainings revealed that αv integrin was expressed by endothelial cells both in normal and DCM hearts. There was no upregulation of total αv integrin expression in DCM, and in fact, we observed a slight, but statistically non-significant downregulation in DCM.
In conclusion, the present results offer insight into the development of targeted vectors for heart failure gene therapy. The shift in expression of CD46 and CAR from subendothelial to endothelial layer of intramyocardial coronary vessels suggests that therapeutic genes could be efficiently delivered to DCM hearts with either of these vectors after intravascular administration. Presently it is not known if this phenomenon applies to other forms of heart failure as well. In many non-cardiovascular gene therapy applications, CD46 is expressed at higher levels than CAR and vectors targeting CD46 have demonstrated superior transduction efficiency when compared with the standard CAR-targeting vectors. The present results demonstrate that in the heart this may not be the case as the expression profiles of CAR and CD46 were similar. As adenoviruses require human CD46 as their attachment receptor, the in vivo comparison of these vectors in the heart must be done, e.g., in transgenic mice expressing the human CD46 gene. Such studies are underway in our laboratory.
References
Akdere F, Bock O, Lehmann U et al (2005) Quantitative mRNA expression analysis of co-stimulatory molecules in sequential biopsies from heart allografts. Transpl Int 18:1197–1202. doi:10.1111/j.1432-2277.2005.00199.x
Amin KM (2003) Ad5 and Ad3 chimeric fiber travels into the cell without the CAR. Cancer Biol Ther 2:516–517
Asaoka K, Tada M, Sawamura Y, Ikeda J, Abe H (2000) Dependence of efficient adenoviral gene delivery in malignant glioma cells on the expression levels of the Coxsackievirus and adenovirus receptor. J Neurosurg 92:1002–1008
Brooks PC, Clark RA, Cheresh DA (1994) Requirement of vascular integrin alpha v beta 3 for angiogenesis. Science 264:569–571
Cheresh DA (1987) Human endothelial cells synthesize and express an Arg-Gly-Asp-directed adhesion receptor involved in attachment to fibrinogen and von Willebrand factor. Proc Natl Acad Sci USA 84:6471–6475
Cirielli C, Serino F, Straino S et al (2004) Adenovirus vectors targeting alphaV integrin or heparan sulfate receptors display different distribution of transgene activity after intramuscular injection. J Gene Med 6:309–316. doi:10.1002/jgm.521
Dorig RE, Marcil A, Chopra A, Richardson CD (1993) The human CD46 molecule is a receptor for measles virus (Edmonston strain). Cell 75:295–305
Douglas JT, Kim M, Sumerel LA, Carey DE, Curiel DT (2001) Efficient oncolysis by a replicating adenovirus (ad) in vivo is critically dependent on tumor expression of primary ad receptors. Cancer Res 61:813–817
Einfeld DA, Schroeder R, Roelvink PW et al (2001) Reducing the native tropism of adenovirus vectors requires removal of both CAR and integrin interactions. J Virol 75:11284–11291. doi:10.1128/JVI.75.23.11284-11291.2001
Fechner H, Noutsias M, Tschoepe C et al (2003) Induction of coxsackievirus-adenovirus-receptor expression during myocardial tissue formation and remodeling: identification of a cell-to-cell contact-dependent regulatory mechanism. Circulation 107:876–882
Gaggar A, Shayakhmetov DM, Lieber A (2003) CD46 is a cellular receptor for group B adenoviruses. Nat Med 9:1408–1412. doi:10.1038/nm952
Giaginis CT, Zarros AC, Papaefthymiou MA, Papadopouli AE, Sfiniadakis IK, Theocharis SE (2008) Coxsackievirus and adenovirus receptor expression in human endometrial adenocarcinoma: possible clinical implications. World J Surg Oncol 6:59. doi:10.1186/1477-7819-6-59
Havenga MJ, Lemckert AA, Ophorst OJ et al (2002) Exploiting the natural diversity in adenovirus tropism for therapy and prevention of disease. J Virol 76:4612–4620
Hemmi S, Geertsen R, Mezzacasa A, Peter I, Dummer R (1998) The presence of human coxsackievirus and adenovirus receptor is associated with efficient adenovirus-mediated transgene expression in human melanoma cell cultures. Hum Gene Ther 9:2363–2373
Janat MF, Argraves WS, Liau G (1992) Regulation of vascular smooth muscle cell integrin expression by transforming growth factor beta1 and by platelet-derived growth factor-BB. J Cell Physiol 151:588–595. doi:10.1002/jcp.1041510319
Kalinowski L, Dobrucki LW, Meoli DF et al (2008) Targeted imaging of hypoxia-induced integrin activation in myocardium early after infarction. J Appl Physiol 104:1504–1512. doi:10.1152/japplphysiol.00861.2007
Kanerva A, Mikheeva GV, Krasnykh V et al (2002) Targeting adenovirus to the serotype 3 receptor increases gene transfer efficiency to ovarian cancer cells. Clin Cancer Res 8:275–280
Kasono K, Blackwell JL, Douglas JT et al (1999) Selective gene delivery to head and neck cancer cells via an integrin targeted adenoviral vector. Clin Cancer Res 5:2571–2579
Kuhl U, Pauschinger M, Seeberg B et al (2005) Viral persistence in the myocardium is associated with progressive cardiac dysfunction. Circulation 112:1965–1970. doi:10.1161/CIRCULATIONAHA.105.548156
Larochelle N, Deol JR, Srivastava V et al (2008) Downregulation of CD46 during muscle differentiation: implications for gene transfer to human skeletal muscle using group B adenoviruses. Hum Gene Ther 19:133–142. doi:10.1089/hum.2007.040
Li D, Duan L, Freimuth P, O’Malley BW Jr (1999) Variability of adenovirus receptor density influences gene transfer efficiency and therapeutic response in head and neck cancer. Clin Cancer Res 5:4175–4181
Matsumoto K, Shariat SF, Ayala GE, Rauen KA, Lerner SP (2005) Loss of coxsackie and adenovirus receptor expression is associated with features of aggressive bladder cancer. Urology 66:441–446. doi:10.1016/j.urology.2005.02.033
Nettelbeck DM, Miller DW, Jerome V et al (2001) Targeting of adenovirus to endothelial cells by a bispecific single-chain diabody directed against the adenovirus fiber knob domain and human endoglin (CD105). Mol Ther 3:882–891. doi:10.1006/mthe.2001.0342
Noutsias M, Seeberg B, Schultheiss HP, Kuhl U (1999) Expression of cell adhesion molecules in dilated cardiomyopathy: evidence for endothelial activation in inflammatory cardiomyopathy. Circulation 99:2124–2131
Noutsias M, Fechner H, de Jonge H et al (2001) Human coxsackie-adenovirus receptor is colocalized with integrins alpha(v)beta(3) and alpha(v)beta(5) on the cardiomyocyte sarcolemma and upregulated in dilated cardiomyopathy: implications for cardiotropic viral infections. Circulation 104:275–280
Rauen KA, Sudilovsky D, Le JL et al (2002) Expression of the coxsackie adenovirus receptor in normal prostate and in primary and metastatic prostate carcinoma: potential relevance to gene therapy. Cancer Res 62:3812–3818
Rissanen TT, Yla-Herttuala S (2007) Current status of cardiovascular gene therapy. Mol Ther 15:1233–1247. doi:10.1038/sj.mt.6300175
Santoro F, Kennedy PE, Locatelli G, Malnati MS, Berger EA, Lusso P (1999) CD46 is a cellular receptor for human herpesvirus 6. Cell 99:817–827
Sasse A, Wallich M, Ding Z, Goedecke A, Schrader J (2003) Coxsackie-and-adenovirus receptor mRNA expression in human heart failure. J Gene Med 5:876–882. doi:10.1002/jgm.411
Segerman A, Mei YF, Wadell G (2000) Adenovirus types 11p and 35p show high binding efficiencies for committed hematopoietic cell lines and are infective to these cell lines. J Virol 74:1457–1467
Seya T, Hirano A, Matsumoto M, Nomura M, Ueda S (1999) Human membrane cofactor protein (MCP, CD46): multiple isoforms and functions. Int J Biochem Cell Biol 31:1255–1260
Shayakhmetov DM, Li ZY, Ni S, Lieber A (2002) Targeting of adenovirus vectors to tumor cells does not enable efficient transduction of breast cancer metastases. Cancer Res 62:1063–1068
Shinozaki K, Suominen E, Carrick F et al (2006) Efficient infection of tumor endothelial cells by a capsid-modified adenovirus. Gene Ther 13:52–59. doi:10.1038/sj.gt.3302598
Short JJ, Pereboev AV, Kawakami Y, Vasu C, Holterman MJ, Curiel DT (2004) Adenovirus serotype 3 utilizes CD80 (B7.1) and CD86 (B7.2) as cellular attachment receptors. Virology 322:349–359. doi:10.1016/j.virol.2004.02.016
Sova P, Ren XW, Ni S et al (2004) A tumor-targeted and conditionally replicating oncolytic adenovirus vector expressing TRAIL for treatment of liver metastases. Mol Ther 9:496–509. doi:10.1016/j.ymthe.2003.12.008
Suominen E, Toivonen R, Grenman R, Savontaus M (2006) Head and neck cancer cells are efficiently infected by Ad5/35 hybrid virus. J Gene Med 8(10):1223–1231. doi:10.1002/jgm.957
van der Merwe PA, Bodian DL, Daenke S, Linsley P, Davis SJ (1997) CD80 (B7–1) binds both CD28 and CTLA-4 with a low affinity and very fast kinetics. J Exp Med 185:393–403
Wickham TJ, Mathias P, Cheresh DA, Nemerow GR (1993) Integrins alpha v beta 3 and alpha v beta 5 promote adenovirus internalization but not virus attachment. Cell 73:309–319
Wickham TJ, Segal DM, Roelvink PW et al (1996) Targeted adenovirus gene transfer to endothelial and smooth muscle cells by using bispecific antibodies. J Virol 70:6831–6838
Zeimet AG, Muller-Holzner E, Schuler A et al (2002) Determination of molecules regulating gene delivery using adenoviral vectors in ovarian carcinomas. Gene Ther 9:1093–1100. doi:10.1038/sj.gt.3301775
Acknowledgments
The authors have no conflicts of interest. We thank Sari Pitkänen for her advice and contribution to the histological stainings, Marjo Hakkarainen and Susanna Pyökäri (Turku Centre for Biotechnology) for their expertise on cell culture and viral vectors and Seija Lindqvist (University of Turku Central Animal Laboratory) for animal care. Mikko Simolin, Suvi Syväranta, the heart transplantation coordinators and the cardiac transplantation team of the Helsinki University Hospital are thanked for help in collection of the cardiac specimens. This work was supported by the Academy of Finland, Finnish Medical Foundation, Turku University Central Hospital, Turku University Foundation, Cancer Foundation of South-Western Finland, Turku Graduate School of Biomedical Sciences and the Finnish Foundation for Cardiovascular Research. Wihuri Research Institute is maintained by the Jenny and Antti Wihuri Foundation.
Conflict of interest statement
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Toivonen, R., Mäyränpää, M.I., Kovanen, P.T. et al. Dilated cardiomyopathy alters the expression patterns of CAR and other adenoviral receptors in human heart. Histochem Cell Biol 133, 349–357 (2010). https://doi.org/10.1007/s00418-009-0666-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00418-009-0666-1