Abstract
To investigate the expression of the endocannabinoid 1 and 2 receptors by human adipocyte cells of omental and subcutaneous fat tissue, as well as to determine whether these receptors are functional. The expression of CB1 and CB2 receptors on human adipocytes was analyzed by western blotting, immunohistology and immunocytology. We also investigated intracytoplasmic cyclic AMP level modulation following CB1 and CB2 receptor stimulation by an enzymatic immuno assay. All mature adipocytes, from visceral (epiploon) and subcutaneous fat tissue, express CB1 and CB2 on their plasma membranes. We also demonstrate in this study that adipocyte precursors (pre-adipocytes) express CB1 and CB2 on their plasma membranes and that both receptors are functional. Activation of CB1 increases intracytoplasmic cyclic AMP whilst CB2 activation leads to a cyclic AMP decrease. Here we demonstrate, for the first time, that adipocytes of human adipose tissue (mature adipocytes and pre-adipocytes) express functional plasma membrane CB1 and CB2 receptors. Their physiological role on the adipose tissue is not known. However, their major involvement in the physiology of other tissues leads us to suppose that they could play a significant role in the homeostasis of the energy balance and/or in the regulation of adipose tissue inflammation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The first recorded medicinal use of cannabis derivatives was found in Chinese and Egyptian texts dating back to several centuries before Jesus Christ. The beneficial effects of the active ingredients of marijuana (Cannabis sativa) have been known for millennia, with them being used to treat pain, spasms, nausea, insomnia and especially lack of appetite. The identification and characterization of the principal active ingredient of C. sativa, Δ9-tetrahydrocannabinol (Δ9-THC), is a recent discovery dating back to 1964 (Gaoni and Mechoulam 1964). Recent rapid progress, due in part to the power of molecular biology techniques, has made it possible to characterize and clone the Δ9-THC receptors, thus raising the crucial question as to the identity of the endogenous ligands. The endogenous cannabinoid ligands or endocannabinoids were identified a few years after the discovery of the first receptor and include the two principal ligands: arachidonylethanolamide (still called anandamide, fatty acid amide) (Devane et al. 1992) and 2-arachidonoylglycerol (2-AG, fatty acid ester) (Mechoulam et al. 1995). Two receptors isolated from rat brain were identified and named CB1 and CB2 (Matsuda et al. 1990). CB1a, a splicing variant truncated at the N-terminal region of the receptor, exhibiting 98% identity, was characterized and was shown to have the same distribution as CB1 (Shire et al. 1995). During this period, a second receptor called CB2 was isolated from myelocyte cells (Munro et al. 1993). The two receptors, CB1 and CB2 exhibit approximately 44% homology as well as some differences in the distribution of their expression. CB1 is mainly expressed, throughout the central nervous system, equally well by neurons as it is by glial cells (Matsuda et al. 1990; Herkenham et al. 1990). Nevertheless it is also expressed at a very much lower level in peripheral tissue, including the testicle, the uterus, the intestine, the bladder, retinal cells, endothelial cells and certain cells of the immune system (Bouaboula et al. 1993). Expression of CB1 has also been demonstrated in rat adipose tissue as well as in primary fat cell cultures (Bensaid et al. 2003). At present, the precise function of the CB1 receptor within peripheral tissue is not well understood (Bouaboula et al. 1993; Bensaid et al. 2003; Cota et al. 2003a; Galiegue et al. 1995; Liu et al. 2000). Studies on the nervous system have elucidated the mechanism of action of the CB1 receptor and made it possible to understand the action of endogenous or exogenous ligands on the physiological functions governed by the central nervous system, in particular the psychotropic effects of cannabis and the regulation of food intake (orexigenic effect of the endocannabinoids) (Cota et al. 2003b; Howlett et al. 1990; Berry and Mechoulam 2002; Martinez-Gonzalez et al. 2004). The expression of the CB2 receptor is primarily restricted to cells of the immune system, although certain studies have demonstrated its presence in the lung, the uterus and the pancreas (Bouaboula et al. 1993; Galiegue et al. 1995). Here we report, for the first time the existence of two new cellular locations of protein expression:
-
Expression of the functional CB1 receptor by human adipocytes.
-
New expression of the functional CB2 receptor by adipose cells (highlighted in our study on humans).
Materials and methods
Origin of adipose tissue samples
Human abdominal subcutaneous adipose tissue samples were obtained from men and women undergoing liposuction in the Department of Plastic Surgery, Centre Hospitalier Départemental Félix Guyon, Saint Denis, La Réunion. The mean age (years) and BMI (kg/m2) for women were 39±8.9 and 26±3, respectively, and for men were 45±5.4 and 27±3.5, respectively. Human omental (epiploon) adipose tissue samples were obtained from women and men undergoing intestinal surgery in the Department of Digestive Surgery, Centre Hospitalier Départemental Félix Guyon, Saint Denis, La Réunion. The mean age (years) and BMI (kg/m2) for women were 51±6.9 and 24±2.3, respectively, and for men were 57±6.4 and 26±4.5, respectively. The presence of an inflammatory syndrome was considered to be a non-inclusion criterion. All patients gave their consent to the gift and the study was approved by the regional CCPPRB (committee for the protection of persons undergoing biomedical research).
Isolation and purification of pre-adipocytes and mature adipocytes
Samples of human adipose tissue were rapidly processed after surgery. Twenty-five milliliters of adipose tissue were incubated with 25 ml Ringer-lactate buffer containing 1.33 or 1 mg/ml of collagenase NB4 (Coger, France), respectively, for pre-adipocyte and mature adipocyte purification, for 30 min at 37°C.
For pre-adipocyte purification, digested tissue was filtered through an 80 μm nylon mesh to eliminate undigested fragments, followed by centrifugation at 1,000g for 10 min. The cell pellet (SVF, Stromal Vascular Fraction) harvested after centrifugation was resuspended and incubated twice for 10 min in BLB (blood lysis buffer pH 7, NH4Cl 155 mM, KHCO3 10 mM, Na2EDTA 1 mM) to eliminate red blood cells. After centrifugation at 1,000g for 10 min, cells were resuspended in 199 medium (PAN Biotech, France). Cell number and viability were assessed by trypan blue dye exclusion.
For mature adipocyte purification, filtration was not carried out; mature adipocyte cells were carefully harvested by pipetting from the higher phase of the suspension after centrifugation at 200g for 20 s. Mature adipocyte were then rinsed with Ringer-lactate buffer.
Immunohistology of omental and subcutaneous adipose tissue
Formalin-fixed normal subcutaneous or omental fat tissue was sectioned on a microtome (7 μm), deparaffinized and unmasked by the use of heat treatment in sodium citrate buffer (10 mM) at 95°C for 15 min. Sections were pre-incubated with 5% bovine serum albumin (BSA) and exposed to a 1:50 dilution of polyclonal anti-human CB1 antibody (101500 CB1 Receptor Polyclonal Antibody, Cayman Chemical Company, USA) or polyclonal anti-human CB2 antibody (101550 CB2 Receptor Polyclonal Antibody, Cayman Chemical Company). Sections were then incubated with the secondary antibody (1/200 coupled to FITC or Alexa Fluor 594™), washed and mounted with Fluoprep (bioMerieux, France) mounting medium. Sections were examined on a fluorescent microscope (TE 2000-U, Nikon).
Immunocytotology of pre-adipocytes and mature adipocytes
Cells isolated from the SVF were plated on glass cover slips in culture flasks at 20,000 cells/cm2 in 199 medium supplemented with 10% FBS (PAN Biotech), 100 U/ml penicillin, 100 μg/ml streptomycin, 25 ng/ml amphotericin B and 100 ng/ml transferrin. Medium was changed every 2 days. Cells were cultured for 16 h (D0), 40 h (D1) and 88 h (D3) on glass cover slips, fixed with 0.4% paraformaldehyde (Sigma, France) and washed three times in PBS. Cells were pre-incubated with 5% BSA and then exposed to a 1:50 dilution of polyclonal anti-human CB1 antibody (101500 CB1 Receptor Polyclonal Antibody, Cayman Chemical Company) or polyclonal anti-human CB2 antibody (101550 CB2 Receptor Polyclonal Antibody, Cayman Chemical Company). After washing, cells were incubated with the secondary antibody (1/200 coupled to FITC or Alexa Fluor 594™), washed and mounted with Fluoprep (bioMerieux) mounting medium. Cells were examined on a fluorescent microscope (TE 2000-U, Nikon).
Mature adipocytes isolated from tissue were incubated with the same primary antibodies as described above and at the same concentrations. Cells were washed with PBS and centrifuged at 200g for 10 s. As above, the cells were then incubated with the same secondary antibody followed by washing. Cells were examined on a fluorescent microscope (TE 2000-U, Nikon).
Protein extraction
Proteins were extracted with 300 μl of lysis buffer [50 mM Tris–HCl pH 7.4, 150 mM NaCl, 1% triton, 1 mM EDTA, 1/20 (v/v) anti-protease cocktail (Sigma)] per culture plate. Protein extraction was quantified by the Bradford dosage assay using BSA as a standard.
Western blot analysis
Sodium dodecyl sulphate-polyacrylamide gel electrophoresis (SDS-PAGE) was performed according to the Laemmli protocol (1970). SDS-PAGE was carried out under reductive conditions with 12.5% running gels and 4% stacking gels. Gels were blotted onto a nitrocellulose membrane (Millipore, France). Membranes were soaked for 30 min in Tris buffered saline (TBS) buffer (138 mM NaCl, 15 mM Tris-base) containing 0.05% (v/v) Tween 20.
Human CB1 protein was visualized with the rabbit polyclonal anti-human CB1 antibody at a 1/500 dilution (101500 CB1 Receptor Polyclonal Antibody, Cayman Chemical Company). Human CB2 protein was visualized with the rabbit polyclonal anti-human CB2 antibody at a 1/500 dilution (101550 CB2 Receptor Polyclonal Antibody, Cayman Chemical Company). The membranes were incubated in TBS-Tween 20 containing 5% non-fat milk with the primary antibody for 2 h at room temperature. The membranes were washed three times for 10 min in TBS-Tween 20 buffer. This was followed by incubation with alkaline phosphatase-conjugated polyclonal anti-rabbit immunoglobulin (1/5,000) (Promega, France) in TBS-Tween 20/non-fat milk for 1 h at room temperature. After four washes of 5 min with TBS buffer, development was completed with an enzymatic assay consisting of a mixture of 5-bromo-4-chloro-3-indolyl phosphate and nitroblue tetrazolium salt in TBS buffer, pH 9.5 (100 mM Tris–HCl, 100 mM NaCl).
Detection of intracellular cyclic AMP level
Pre-adipocytes were cultivated in 60 mm culture plates until confluence (D7) following the same culture protocol as that used for the preparation of cells for the immunocytology assays. For CB1 stimulation, cells were treated for 7 min with 2-arachidonoylglycerol (2-AG) (Cayman Chemical Company) at 1, 2 and 5 nM concentrations as well as 5 nM 2-AG with 50 or 75 nM AM251 (Cayman Chemical Company). Cells treated with 0.1% ethanol were used as controls.
For CB2 stimulation, cells were pre-incubated for 10 min with 1 μM forskolin (Sigma) followed by treatment for 7 min with palmitoylethanolamide (PEA) (Cayman Chemical Company) at 20, 50, 100 μM concentrations as well as 100 μM PEA with 10 μM SR 144528 (Sanofi-Synthelabo company gift). Cells treated with 1 μM forskolin alone were used as controls. Following incubation, the medium was removed and 250 μl of 0.1 M HCl was added to each plate and incubated for 20 min at room temperature. Cells were removed with a cell scraper and a homogenous suspension obtained by repeated pipetting. This was centrifuged at 1,000g for 10 min. The cyclic AMP concentration in the supernatant was quantified by use of an Enzymatic Immuno Assay kit (Cayman Chemical Company) in accordance with the manufacturer’s instructions.
Mature adipocytes isolated from adipose tissue were cultured in 24 well plates (50,000 cells per well) without FBS for 18 h in the same culture medium as that used for the pre-adipocytes. The CB1 and CB2 stimulation protocol was carried out as described above.
Following stimulation, 200 μl of 0.1 M HCl was added to each well and incubated for 20 min at room temperature. The mixture was pipetted to obtain a homogeneous suspension and centrifuged at 1,000g for 10 min. The cyclic AMP concentration in the supernatant was quantified as above.
RNA preparation and reverse transcription
Cells from each 60 mm plate were extracted with 500 μl of TRIzol™ reagent (Invitrogen, France). Total RNA was isolated and precipitated according to the manufacturer’s instructions. Five micrograms of total RNA was reverse transcribed using random heptamer primers (Eurogentec, Belgium) with SuperscriptTM II (Invitrogen) according to the manufacturer’s instructions.
Real-time PCR
One microliter of reverse-transcribed RNA was amplified on an ABI PRISM 7000 thermal cycler (Applied Biosystems, France) using the Taqman™ Master Mix Kit (Eurogentec) in a 25 μl reaction volume. The primers used are indicated below. The 18S ribosomal RNA (rRNA) gene was used as an internal standard. Real-time amplifications were then analyzed using Sequence Detector software 1.1 (Applied Biosystems) and quantification of target mRNA was carried out by comparison of the number of cycles required in order to reach the reference point (ΔΔCT method).
CB1 (quantity used for one reaction volume: primers 10 pmol, probe 15 pmol) Primer (5′) 5′-CAC AGC CAT CGA CAG GTA CAT ATC-3′ Primer (3′) 5′-ACG GCG ATC ACA ATG GCT AT-3′ Probe 5′- FAM-ATT GTC ACC AGG CCC AAG GCC G -TAMRA-3′ |
CB2 (quantity used for one reaction volume: primers 10 pmol, probe 10 pmol) Primer (5′) 5′-ATCCTGAGTGGTCCCCAGAAG-3′ Primer (3′) 5′-GTGGGAGGACAGGATCAGATAGAG-3′ Probe 5′-FAM-TGC TAA GTG CCC TGG AGA ACG TGG C -TAMRA-3′ |
18 S (quantity used for one reaction volume: primers 5 pmol, probe 5 pmol) Primer (5′) 5′-CAT TCT TGG CAA ATG CTT TC-3′ Primer (3′) 5′-CGC CGC TAG AGG TGA AAT TCT-3′ Probe 5′-JOE-ACC GGC GCA AGA CGG ACC AGA-TAMRA-3′ |
Results
Expression of CB1 and CB2 receptors genes in pre-adipocytes and mature adipocytes
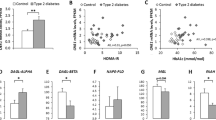
We have used real-time PCR to demonstrate expression of CB1 and CB2 on pre-adipocytes and mature adipocytes at mRNA level. These two cellular types, proceeding whether from omental or subcutaneous tissue, or from male or female subjects, express both messages (representative results shown in Fig. 1, panel A).
CB1 and CB2 gene expression in pre-adipocyte and mature adipocyte. Panel A Analyze of RT-PCR products was performed on 4% agarose gel. Only results obtained from subcutaneous tissue were shown. Same results were obtained with pre-adipocyte and mature adipocyte isolated from omental fat tissue. Lane 1 amplification obtained using specific CB1 primers with pre-adipocyte. Lane 2 amplification obtained using specific CB1 primers with mature adipocyte. Lane 3 amplification obtained using specific CB2 primers with pre-adipocyte. Lane 4 amplification obtained using specific CB2 primers with mature adipocyte. Lane 5 molecular weight. Panel B CB1 and CB2 gene relative expression in cells isolated from subcutaneous fat tissue. Same legends were attributed that above. Results were expressed comparatively to CB1 gene expression arbitrary fixed to 1. Values are expressed in arbitrary units as means with SD in vertical bars (n=9). Filled diamond and filled circle denotes P<0.01 compared with CB1 gene expression by Student’s t test
We have determined, by real-time RT-PCR, CB1 and CB2 mRNA level in adipose cells isolated from fat subcutaneous tissue. CB1 and CB2 mRNA levels were, respectively, 130- and 61-fold higher in mature adipocytes than in pre-adipocytes (Fig. 1, panel B). We have also determined that CB2 expression was higher than those of CB1. Expression level was, respectively, approximately 8- and 4-fold higher in pre-adipocyte and in mature adipocyte.
Expression of CB1 and CB2 receptors protein on mature adipose cells
In this study, an immunohistological assay was used to demonstrate protein expression of CB1 and CB2 receptors on native adipocyte plasma membranes. Figure 2 shows a positive staining profile throughout the plasma membrane of mature adipocytes. Immunocytological labeling of isolated mature adipocytes from adipose tissue was carried out in order to verify the existence of CB1 and CB2 on these cells. Figure 3 shows, as for the immunohistological assay, a positive staining profile throughout the plasma membrane of isolated mature adipocytes. In both labeling assays, the binding specificity of the secondary antibody was assured by the absence of a positive signal following incubation with the secondary antibody alone.
Plasma membrane expression of CB1 and CB2 receptors by mature adipocytes in omental and subcutaneous fat tissue. Immunohistology was performed on 7 μm thick tissue sections with polyclonal anti-human CB1 or polyclonal anti-human CB2 antibodies. Panel A omental adipocyte staining with 1/50 anti-CB1 + 1/200 FITC conjugated secondary antibody; Panel B tissue with 1/200 FITC conjugated secondary antibody only; Panel C subcutaneous adipocyte staining with 1/50 anti-CB1 + 1/200 FITC conjugated secondary antibody; Panel D omental adipocyte staining with 1/50 anti-CB2 + 1/200; Panel E tissue with 1/200 Alexa Fluor 594™ conjugated secondary antibody only; Panel F subcutaneous adipocyte staining with 1/50 anti-CB2 + 1/200 Alexa Fluor 594™ conjugated secondary antibody. Magnification 250×
Plasma membrane expression of CB1 and CB2 receptors by mature adipocytes isolated from omental and subcutaneous fat tissue. Immunocytology was performed on mature adipocytes isolated from omental and subcutaneous fat tissue. Panel A Omental mature adipocyte staining with 1/50 anti-CB1 + 1/200 FITC conjugated secondary antibody; Panel B omental mature adipocyte with 1/200 FITC conjugated secondary antibody only; Panel C omental mature adipocyte staining with 1/50 anti-CB2 + 1/200 Alexa Fluor 594™ conjugated secondary antibody; Panel D omental mature adipocyte with 1/200 Alexa Fluor 594™ conjugated secondary antibody only. Same staining was obtained with mature adipocyte isolated from subcutaneous fat tissue. Magnification 100×
Staining was carried out on two types of fat tissue (omental and abdominal subcutaneous fat) derived from male and female subjects. Three omental and four subcutaneous samples were analyzed from the two sexes (14 samples). In all cases, CB1 and CB2 receptors were shown to be present on the plasma membrane of mature adipocytes (representative staining of one sample from each origin was shown, Figs. 2, 3). In order to verify that the antibodies used for the recognition of CB1 and CB2 were specific for the ligands, western blotting was carried out on isolated mature adipocyte proteins isolated from tissue by collagenase treatment. A single band of the expected size (45 kDa for CB1, 55 kDa for CB2) was revealed following incubation with the polyclonal anti-human CB1 and CB2 antibodies used for the immunohistology and immunocytology assays (Fig. 4). We have also carried out immunostaining on cells which expressed both receptors CB1 and CB2 (leucocytes, Fig. 6a). We have verified that positive staining obtained was CB1 and CB2 presence specific by realizing the same staining on cells which do not express cannabinoid receptors (blood red cells, Fig. 6b).
Western blot analysis of CB1 and CB2 receptors expressed by human omental and subcutaneous mature adipocytes and pre-adipocytes. In each lane 50 μg total protein was separated by SDS-PAGE. Staining was performed with anti-CB1 (lane A–E) and anti-CB2 (lane F–J) antibodies. Lane A pre-adipocyte protein from omental tissue; Lane B mature adipocyte protein from omental tissue; Lane C pre-adipocyte protein from subcutaneous tissue; Lane D mature adipocyte protein from subcutaneous tissue; Lane E extracted brain cell protein (positive control). Lane F pre-adipocyte protein from omental tissue; Lane G mature adipocyte protein from omental tissue; Lane H pre-adipocyte protein from subcutaneous tissue; Lane I mature adipocyte protein from subcutaneous tissue; Lane J Jurkat cell protein (positive control). No staining was obtained with secondary antibodies alone (data not shown)
We are thus able to confirm that mature human adipocytes, whether from omental or subcutaneous tissue, or from male or female subjects, express, on their surface, CB1 and CB2 cannabinoid receptors.
Expression of CB1 and CB2 receptors protein on pre-adipocytes
Immunocytology on pre-adipocytes was also carried out in order to investigate the presence of cannabinoid receptors in these cells isolated from fat tissue (staining was not visible by immunohistology as the size and quantity of pre-adipocytes compared to the total number of cells investigated is too small). Labeling was carried out 16 h (D0) and 88 h (D3) after seeding cells on glass cover slips so as to allow the cells to adhere. Flow cytometric analysis of the cell population (SVF) was carried out at 16 and 88 h in order to ascertain the proportion of the various cell types present (Festy et al. 2005). Cells of the SVF possessing the CD34+ and CD31- phenotype have been characterized as being the only cells able to differentiate into adipocytes and thus are considered to be the cellular precursors of adipocytes (Sengenes et al. 2005). After 88 h of incubation (D3) almost all of the cells display this phenotype as well as positive labeling for the presence of CB1 and CB2 (Fig. 5, 6). At D0, 7–15% of the cells expressed the leukocyte specific surface antigen CD45, with approximately half being identified as lymphocytes (CD3+) and the rest as macrophages (CD14+ and/or CD15+). In addition 20% of the cells presented the endothelial cell specific surface antigen CD31, with around 65% of the remaining cells possessing the CD34+ and CD31− phenotype. At D0, a very large proportion of the cells exhibit positive labeling for the CB1 and CB2 receptors (more than 70%, data not shown). Thus, the majority of the cells labeled by immunofluorescence are pre-adipocytes. This can be assumed with certainty as the contaminant population represents no more than 35% of the total cells extracted from the SVF and thus cannot be the origin of the uniform labeling observed.
Plasma membrane expression of CB1 and CB2 receptors by pre-adipocytes. Immunocytology was performed with polyclonal anti-human CB1 or polyclonal anti-human CB2 antibodies. Panel A omental pre-adipocyte staining with 1/50 anti-CB1 + 1/200 FITC conjugated secondary antibody; Panel B omental pre-adipocyte staining with 1/200 FITC conjugated secondary antibody only; Panel C omental pre-adipocyte staining with 1/50 anti-CB2 + 1/200 Alexa Fluor 594™ conjugated secondary antibody; Panel D omental pre-adipocyte staining with 1/200 Alexa Fluor 594™ conjugated secondary antibody only. The same staining experiment was performed with pre-adipocytes isolated from subcutaneous fat tissue, with identical results obtained (positive staining for CB1 and CB2, data not shown). Magnification 250×
a CB1 and CB2 staining positive control. Immunocytology was performed on blood-isolated leucocytes with polyclonal anti-human CB1 or anti-human CB2 antibodies used for adipocyte staining. Panel A leucocyte staining with 1/50 anti-CB1 + 1/200 FITC conjugated secondary antibody; Panel B leucocyte staining with 1/200 FITC conjugated secondary antibody only; Panel C leucocyte staining with 1/50 anti-CB2 + 1/200 Alexa Fluor 594™ conjugated secondary antibody; Panel D leucocyte staining with 1/200 Alexa Fluor 594™ conjugated secondary antibody only. Magnification 400×. b CB1 and CB2 staining negative control. Immunocytology was performed on blood-isolated red cells with polyclonal anti-human CB1 or anti-human CB2 antibodies used for adipocyte staining. Panel A red cells staining with 1/50 anti-CB1 + 1/200 FITC conjugated secondary antibody; Panel B red cells staining with 1/50 anti CD36 + 1/200 FITC conjugated secondary antibody; Panel C red cells staining with 1/50 anti-CB2 + 1/200 Alexa Fluor 594™ conjugated secondary antibody; Panel D red cells staining with anti CD36 + 1/200 Alexa Fluor 594™ conjugated secondary antibody only. Magnification 400×
The presence of CB1 and CB2 receptors is therefore not due to an expression artifact resulting from cell culture. As for the mature adipocytes, proteins of cells derived from the SVF were extracted and analyzed by western blotting. A single band of the expected size was revealed following incubation with the polyclonal anti-human CB1 and CB2 antibodies (Fig. 4). Labeling was carried out on the 14 fat tissue samples already described and showed in all cases that pre-adipocytes were positively labeled for CB1 and CB2. Thus, we can conclude that irrespective of sex or tissue origin, all pre-adipocytes express on their surface the CB1 and CB2 receptors.
Functionality of CB1 and CB2 receptors expressed on adipose cells
In order to demonstrate that the two receptors, CB1 and CB2, are functional, we tested the action of two agonists upon the production of the cyclic AMP second messenger. The experiment was carried out with both types of cellular adipocytes (mature adipocytes and pre-adipocytes). In both cases, the results obtained are similar and lead us to the same conclusions. As such, in order to reduce the number of similar results presented, only data relating to the pre-adipocytes will be discussed.
2-AG increases the production of intracytoplasmic cyclic AMP (Fig. 7). The production of cyclic AMP was 1.5, 1.8 and 2.2-fold higher than the control with, respectively, 1, 2 and 5 nM of 2-AG. This effect is dose dependent even though the difference between 1 and 2 nM, as well as between 2 and 5 nM is not significant with P≤0.05. The difference between the results obtained with doses of 1 and 5 nM is significant with P<0.01. It was demonstrated in vitro that 2-AG could act as a ligand for the CB1 and CB2 receptors, with three times greater affinity for CB1 than for CB2 (K i 58 and 1,400 nM, respectively, for CB1 and CB2; Ben-Shabat et al. 1998). In order to verify that the CB1 receptor is in effect responsible for the augmentation of cyclic AMP by 2-AG, we wanted to inhibit this effect with a receptor specific antagonist. AM 251 is an antagonist with an affinity for CB1 1,000 times greater than for CB2 (K i 12 and 13,200 nM, respectively, for CB1 and CB2) (Felder and Glass 1998; Rinaldi-Carmona et al. 1994). AM 251 functions by blocking, in a dose dependent manner, the increase in the production of cyclic AMP by 2-AG. In effect, AM 251 at doses of 50 and 75 nM results in a reduction in 2-AG induced production of cyclic AMP of 14 and 42%, respectively. Thus, 2-AG increases in a significant dose dependent way the level of intracytoplasmic cyclic AMP and is characterized by the activation of CB1 receptors.
Increase in intracytoplasmic cyclic AMP production by 2-AG. Pre-adipocyte cells were cultivated until confluence (D7). Then, cells were treated for 7 min with 2-arachidonoylglycerol (2-AG) at 1, 2 and 5 nM concentrations. In order to be sure that the 2-AG was effectively acting upon the CB1 receptor, the cells were treated with 5 nM 2-AG with 50 or 75 nM of the specific CB1 receptor antagonist, AM 251. Cells treated with 0.1% ethanol were used as controls. CAMP concentration values are expressed as means (pmol cAMP/104 cell) with SD in vertical bars (n=9). Double asterisks denote P<0.01 compared with control by Student’s t test; filled circle denotes P<0.05 compared with 2-AG 5 nM by Student’s t test; and Double filled circle denotes P<0.01 compared with 2-AG 5 nM by Student’s t test
The action of PEA alone does not modify the levels of intracytoplasmic cyclic AMP (same level as the control, data not shown). In order to demonstrate its effect, we investigated the inhibitory action of PEA compared to the stimulation of cyclic AMP production by forskolin, a strong activator of adenylyl cyclase. Incubation with 1 μM forskolin gives rise to an intracytoplasmic cyclic AMP level 3-fold higher than the control assay (Figs. 7, 8). PEA inhibits the production of cyclic AMP induced by forskolin, with 14% inhibition observed with 50 μM of PEA and 25% inhibition with 100 μM. There is a large consensus of opinion that PEA does not interact with CB1 and that a part of their effects are mediated by CB2 (Devane et al. 1992; Felder et al. 1993; Facci et al. 1995). In this study, we have used PEA concentrations between 20 and 100 μM in order to demonstrate that the effect PEA has upon the inhibition of the production of cyclic AMP is effectively mediated by the CB2 receptor. The specific CB2 receptor antagonist, SR 144528 was chosen to investigate this effect (Rinaldi-Carmona et al. 1998). SR 144528 at a concentration of 100 μM reverses the PEA-induced inhibition of cyclic AMP production by 72% (25% of inhibition without SR 144528 vs. 6.5% with SR 144528, Fig. 8). Thus, CB2 is a functional receptor in human adipocytes with activation inducing an inhibition of the production of cyclic AMP.
Decrease in intracytoplasmic cyclic AMP production by PEA. Fat tissue isolated mature adipocytes were treated for 7 min with 1 μM forskolin either alone (control), or with palmitoylethanolamide (PEA) at 20, 50 and 100 μM or 100 μM PEA plus 10 μM SR 144528. CAMP concentration values are expressed as means (pmol cAMP/104 cell) with SD in vertical bars (n=9). Double asterisks denote P<0.01 compared with control by Student’s t test; single asterisk denotes P<0.05 compared with control by Student’s t test; filled star denotes P<0.05 compared with control by Student’s t test
Discussion
The work of a number of research groups on the expression of murine CB1 adipocyte receptors has lead to some controversy. Certain studies have reported the expression of CB1 on mature murine adipocytes (Bensaid et al. 2003; Cota et al. 2003a). However, in recent work, Nieri et al. have suggested that cannabinoid receptors are not present in the epididymal rat adipocyte while fat cells respond to cannabinoid agonists (Nieri et al. 2003). In this study, we demonstrate without ambiguity and for the first time that human mature adipocytes, as well as their cell precursors (pre-adipocytes) of visceral and subcutaneous adipose tissue of male and female subjects, express type 1 cannabinoid receptors (CB1). We also show that this receptor is functional and that its activation brings about an increase in the intracytoplasmic cyclic AMP level. The relationship between CB1 receptor stimulation and the modification of cAMP levels is not new. In a number of studies it has been shown that CB1 activation could, respectively, stimulate or inhibit adenylate cyclase via the proteins Gs or Gi/o (Glass and Felder 1997; Rhee et al. 1998). The function of the CB1 receptor within adipose tissue is not known. In recent years, the physiological role of the endogenous cannabinoid system has been implicated in appetite control, highlighting CB1 as a novel and promising drug target (Cota et al. 2003a, b; Martinez-Gonzalez et al. 2004). Some studies would suggest that the endocannabinoids have a direct effect upon adipocyte metabolism (Gomez et al. 2002). The presence of CB1 receptors on adipocytes could be an explanation for the understanding of the peripheral effect of physiological adipocyte modification by direct endocannabinoid action on fat tissue. It is possible to imagine that the activation of cannabinoid receptors may modulate fat storage by regulating the adipogenesis/adipolysis balance. However, as is also the case in the murine model, this hypothesis remains to be confirmed.
Secondly, we demonstrate for the first time that human mature adipocytes, as well as their cell precursors (pre-adipocytes) of visceral and subcutaneous adipose tissue of male and female subjects, also express the CB2 cannabinoid receptor. This is certainly the most original discovery of this study, as we have uniquely demonstrated the expression of CB2, something that has not been reported by any other group, irrespective of the species studied. The expression of this receptor has previously been associated with cells of the immune system (Bouaboula et al. 1993). The CB2 receptor on adipocytes is functional, with its activation bringing about the inhibition of cyclic AMP production. Several studies have already demonstrated a link between CB2 and the inhibition of adenylate cyclase via a Gi/o protein (Vogel et al. 1993; Felder et al. 1992). It has also been reported that the endocannabinoid system has an immunomodulatory role, in particular in leukocytes, both at the whole organism as well as at the cellular level (Klein et al. 2004; Cabral and Fischer-Stenger 1994; McCoy et al. 1999; Massa et al. 2004). The function of CB2 receptors in adipose tissue is at the present time unknown, but could be related to adipose tissue inflammation. Excessive weight gain can lead to functional disturbances in the adipose tissue, which result in dysfunction of other peripheral organs (regrouped as metabolic syndromes) (Hubert et al. 1983; Yanovski and Yanovski 2002). During the expansion of the adipose tissue, secretion of leptin, resistin and pro-inflammatory molecules such as TNFα and IL6 are increased (Wellen and Hotamisligil 2003; Xu et al. 2003). Recently, it has been shown that this inflammatory state was largely maintained by macrophage infiltration in the adipose tissue (Weisberg et al. 2003). The limitation or even control of this deleterious inflammatory state could lead to a limitation in weight related morbidity. As in leukocytes, the presence of CB2 in adipose cells, whilst their exact function remains to be determined, provides extremely promising therapeutic targets for the downregulation of adipose tissue inflammation (Piomelli et al. 2000).
Conclusion
Here, we demonstrate for the first time that mature human adipocytes, as well as their cell precursors, the pre-adipocytes, express the CB1 and CB2 cannabinoid receptors. Expression of these receptors occurs both on adipocytes from visceral (epiploon) tissue as well as adipocytes from subcutaneous tissue from male and female subjects. These two cannabinoid receptors are functional with the activation of CB1 and CB2 bringing about, respectively, an increase and decrease in the levels of intracytoplasmic cyclic AMP.
References
Bensaid M, Gary-Bobo M, Esclangon A, Maffrand JP, Le Fur G, Oury-Donat F, Soubrie P (2003) The cannabinoid CB1 receptor antagonist SR141716 increases Acrp30 mRNA expression in adipose tissue of obese fa/fa rats and in cultured adipocyte cells. Mol Pharmacol 63(4):908–914
Ben-Shabat S, Fride E, Sheskin T, Tamiri T, Rhee MH, Vogel Z, Bisogno T, De Petrocellis L, Di Marzo V, Mechoulam R (1998) An entourage effect: inactive endogenous fatty acid glycerol esters enhance 2-arachidonoyl-glycerol cannabinoid activity. Eur J Pharmacol 353:23–31
Berry EM, Mechoulam R (2002) Tetrahydrocannabinol and endocannabinoids in feeding and appetite. Pharmacol Ther 95:185–190
Bouaboula M, Rinaldi M, Carayon P, Carillon C, Delpech B, Shire D, Le Fur G, Casellas P (1993) Cannabinoid-receptor expression in human leukocytes. Eur J Biochem 214:173–180
Cabral GA, Fischer-Stenger K (1994) Inhibition of macrophage inducible protein expression by delta-9-tetrahydrocannabinol. Life Sci 54:1831–1844
Cota D, Marsicano G, Tschop M, Grubler Y, Flachskamm C, Schubert M, Auer D, Yassouridis A, Thone-Reineke C, Ortmann S et al (2003a) The endogenous cannabinoid system affects energy balance via central orexigenic drive and peripheral lipogenesis. J Clin Invest 112:423–431
Cota D, Marsicano G, Lutz B, Vicennati V, Stalla GK, Pasquali R, Pagotto U (2003b) Endogenous cannabinoid system as a modulator of food intake. Int J Obes Relat Metab Disord 27:289–301
Devane WA, Hanus L, Breuer A, Pertwee RG, Stevenson LA, Griffin G, Gibson D, Mandelbaum A, Etinger A, Mechoulam R (1992) Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science 258:1946–1949
Facci L, Dal Toso R, Romanello S, Buriani A, Skaper SD, Leon A (1995) Mast cells express a peripheral cannabinoid receptor with differential sensitivity to anandamide and palmitoylethanolamide. Proc Natl Acad Sci USA 92:3376–3380
Felder CC, Glass M (1998) Cannabinoid receptors and their endogenous agonists. Annu Rev Pharmacol Toxicol 38:179–200
Felder CC, Veluz JS, Williams HL, Briley EM, Matsuda LA (1992) Cannabinoid agonists stimulate both receptor- and non-receptor-mediated signal transduction pathways in cells transfected with and expressing cannabinoid receptor clones. Mol Pharmacol 42:838–845
Felder CC, Briley EM, Axelrod J, Simpson JT, Mackie K, Devane WA (1993) Anandamide, an endogenous cannabimimetic eicosanoid, binds to the cloned human cannabinoid receptor and stimulates receptor-mediated signal transduction. Proc Natl Acad Sci USA 90:7656–7660
Festy F, Hoareau L, Bes-Houtmann S, Péquin AM, Gonthier MP, Munstun A, Hoarau JJ, Césari M, Roche R (2005) Surface proteins expression between human adipose tissue-derived stromal cells and mature adipocytes. Histochem Cell Biol 20:1–9
Galiegue S, Mary S, Marchand J, Dussossoy D, Carriere D, Carayon P, Bouaboula M, Shire D, Le Fur G, Casellas P (1995) Expression of central and peripheral cannabinoid receptors in human immune tissues and leukocyte subpopulations. Eur J Biochem 232:54–61
Gaoni Y, Mechoulam R (1964) Isolation, structure and partial synthesis of an active constituent of hashish. J Am Chem Soc 86:1646–1647
Glass M, Felder CC (1997) Concurrent stimulation of cannabinoid CB1 and dopamine D2 receptors augments cAMP accumulation in striatal neurons: evidence for a Gs linkage to the CB1 receptor. J Neurosci 17:5327–5333
Gomez R, Navarro M, Ferrer B, Trigo JM, Bilbao A, Del Arco I, Cippitelli A, Nava F, Piomelli D, Rodriguez de Fonseca F (2002) A peripheral mechanism for CB1 cannabinoid receptor-dependent modulation of feeding. J Neurosci 22:9612–9617
Herkenham M, Lynn AB, Little MD, Johnson MR, Melvin LS, de Costa BR, Rice KC (1990) Cannabinoid receptor localization in brain. Proc Natl Acad Sci USA 87:1932–1936
Howlett AC, Bidaut-Russell M, Devane WA, Melvin LS, Johnson MR, Herkenham M (1990) The cannabinoid receptor: biochemical, anatomical and behavioral characterization. Trends Neurosci 13:420–423
Hubert HB, Feinleib M, McNamara PM, Castelli WP (1983) Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation 67:968–977
Klein TW, Newton C, Larsen K, Chou J, Perkins I, Lu L, Nong L, Friedman H (2004) Cannabinoid receptors and T helper cells. J Neuroimmunol 147:91–94
Liu J, Gao B, Mirshahi F, Sanyal AJ, Khanolkar AD, Makriyannis A, Kunos G (2000) Functional CB1 cannabinoid receptors in human vascular endothelial cells. Biochem J 346(Pt 3):835–840
Martinez-Gonzalez D, Bonilla-Jaime H, Morales-Otal A, Henriksen SJ, Velazquez-Moctezuma J, Prospero-Garcia O (2004) Oleamide and anandamide effects on food intake and sexual behavior of rats. Neurosci Lett 364:1–6
Massa F, Marsicano G, Hermann H, Cannich A, Monory K, Cravatt BF, Ferri GL, Sibaev A, Storr M, Lutz B (2004) The endogenous cannabinoid system protects against colonic inflammation. J Clin Invest 113:1202–1209
Matsuda LA, Lolait SJ, Brownstein MJ, Young AC, Bonner TI (1990) Structure of a cannabinoid receptor and functional expression of the cloned cDNA. Nature 346:561–564
McCoy KL, Matveyeva M, Carlisle SJ, Cabral GA (1999) Cannabinoid inhibition of the processing of intact lysozyme by macrophages: evidence for CB2 receptor participation. J Pharmacol Exp Ther 289:1620–1625
Mechoulam R, Ben-Shabat S, Hanus L, Ligumsky M, Kaminski NE, Schatz AR, Gopher A, Almog S, Martin BR, Compton DR et al (1995) Identification of an endogenous 2-monoglyceride, present in canine gut, that binds to cannabinoid receptors. Biochem Pharmacol 50:83–90
Munro S, Thomas KL, Abu-Shaar M (1993) Molecular characterization of a peripheral receptor for cannabinoids. Nature 365:61–65
Nieri P, Greco R, Adinolfi B, Breschi MC, Martinotti E, Nannetti C, Podesta A (2003) CB1- and CB2-cannabinoid receptor-independent lipolysis induced by WIN 55,212-2 in male rat adipocytes. Naunyn Schmiedebergs Arch Pharmacol 368:352–359
Piomelli D, Giuffrida A, Calignano A, Rodriguez de Fonseca F (2000) The endocannabinoid system as a target for therapeutic drugs. Trends Pharmacol Sci 21:218–224
Rhee MH, Bayewitch M, Avidor-Reiss T, Levy R, Vogel Z (1998) Cannabinoid receptor activation differentially regulates the various adenylyl cyclase isozymes. J Neurochem 71:1525–1534
Rinaldi-Carmona M, Barth F, Heaulme M, Shire D, Calandra B, Congy C, Martinez S, Maruani J, Neliat G, Caput D et al (1994) SR141716A, a potent and selective antagonist of the brain cannabinoid receptor. FEBS Lett 350:240–244
Rinaldi-Carmona M, Barth F, Millan J, Derocq JM, Casellas P, Congy C, Oustric D, Sarran M, Bouaboula M, Calandra B, Portier M, Shire D, Breliere JC, Le Fur GL (1998) SR 144528, the first potent and selective antagonist of the CB2 cannabinoid receptor. J Pharmacol Exp Ther 284:644–650
Sengenes C, Lolmede K, Zakaroff-Girard A, Busse R, Bouloumie A (2005) Preadipocytes in the human subcutaneous adipose tissue display distinct features from the adult mesenchymal and hematopoietic stem cells. J Cell Physiol 205(1):114–122
Shire D, Carillon C, Kaghad M, Calandra B, Rinaldi-Carmona M, Le Fur G, Caput D, Ferrara P (1995) An amino-terminal variant of the central cannabinoid receptor resulting from alternative splicing. J Biol Chem 270:3726–3731
Vogel Z, Barg J, Levy R, Saya D, Heldman E, Mechoulam R (1993) Anandamide, a brain endogenous compound, interacts specifically with cannabinoid receptors and inhibits adenylate cyclase. J Neurochem 61:352–355
Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW Jr (2003) Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest 112:1796–1808
Wellen KE, Hotamisligil GS (2003) Obesity-induced inflammatory changes in adipose tissue. J Clin Invest 112:1785–1788
Xu H, Barnes GT, Yang Q, Tan G, Yang D, Chou CJ, Sole J, Nichols A, Ross JS, Tartaglia LA et al (2003) Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest 112:1821–1830
Yanovski SZ, Yanovski JA (2002) Obesity. N Engl J Med 346:591–602
Acknowledgements
We would like to thank the plastic surgeons J.F. Baron, P. Delarue and J. Gonçalves who took part in this study and allowed the collection of subcutaneous adipose tissue samples; the gastrointestinal surgeons Y. Haffaf, A. Munstun and T. Aziz who took part in this study and allowed the collection of visceral adipose tissue samples; the CHD Félix Guyon Hospital, Reunion Island, for welcoming our research team, as well as for all of the technical services placed at our disposal; The Ministry of National Education and of Research, as well as the Overseas Ministry of the French State for their financial support; The Regional Council, also for their financial support. Finally all patients who consented to the collection of peri-operative tissue samples and thus made this study possible.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roche, R., Hoareau, L., Bes-Houtmann, S. et al. Presence of the cannabinoid receptors, CB1 and CB2, in human omental and subcutaneous adipocytes. Histochem Cell Biol 126, 177–187 (2006). https://doi.org/10.1007/s00418-005-0127-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00418-005-0127-4