Abstract
Purpose
To detail the methodology for a novel ocular trauma registry and utilize the registry to determine the demographics, nature of injury, and associations of severe visual loss for open globe injuries (OGI).
Methods
Thirteen hospitals in 7 countries used International Globe and Adnexal Trauma Epidemiology Study (IGATES) platform. Patients presenting between April 2009 and 2020 with OGI (with or without) adnexal involvement or intraocular foreign body (IOFB) were included.
Results
Analyses of presenting and final VA, using “severe vision loss” (VA ≤ 6/60) and “no severe loss” (VA > 6/60), were performed. Four hundred fifty-four (64%) patients had VA < 6/60 at presentation and 327 (44.8%) at final follow-up, with a highly significant association between presenting and final VA (p < 0.0001). From the cohort of 746 patients, 37 were missing VA at presentation and 16 at follow-up and complete clinical data was available for 354 patients. The male to female ratio is 6:1, and mean age 36.0 ± 20.0 years old. Relative afferent pupillary defect (RAPD), zone III injury, IOFB, and eyelid injury at presentation were recorded in 50 (6.7%), 55 (7.8%), 97 (13%), and 87 (11.7%) patients, respectively, and were significantly associated with VA < 6/60 at follow-up. Older age, ≥ 61 years, was associated with 3.39 times (95% CI: 1.95–5.89) higher risk than ≤20-year-old patients (p < 0.0001) and males 0.424 times (95% CI: 0.27–0.70) lower risk than female (p = 0.0001) of severe vision loss (SVL).
Conclusion
In OGIs from 13 hospitals, female gender, older age, zone III injury, eyelid injury, and IOFB were associated with higher risk of visual outcome of SVL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Ocular trauma is the leading cause of monocular vision loss internationally [1]; there are significant social and economic costs associated with its treatment and management [2, 3]. The lifetime prevalence of ocular injuries has been estimated at between 13.5 [4] and 22.5 in 1000 people [5]. Risk factors for ocular trauma include younger age [6, 7], male gender [8, 9], and lower socioeconomic status [10]. Improved knowledge of the circumstances of an injury and factors associated with poor clinical outcomes may aid the development of evidence-based prevention programs. Clinical prognostication for patients presenting with ocular trauma is needed for appropriate counseling and management. The Ocular Trauma Score (OTS) is currently accepted as the gold standard for prognostication [11] but has a number of limitations [12]. Limitations include the lack of information about the mechanism of injury and adnexal injuries, limited application in children due to difficulties in VA assessment in these patients, and limited clinical relevance of the zone demarcations [12] [13].
In order to address these uncertainties, robust data are required. Randomized control trials (RCTs) in the context of OGIs are difficult because of the variety of injuries, making multicenter cohort studies essential. The lack of data on ocular trauma is compounded by the absence of standardized method for data collection. The United States Eye Injury Registry (USEIR) was the most successful registry for classification, analysis, and reporting of ocular trauma [14], including in Cuba [15] and Hungary [9], but no internationally accepted format exists.
Registries have been effectively used in ophthalmology [16] [17]. Injury registries with clearly defined data points, determined by expert consensus, may be a useful tool to gather robust data from a geographically dispersed patient base [14]. To our knowledge, the International Globe and Adnexal Trauma Epidemiology Study (IGATES) is the first multinational collaboration to establish a digital registry for ocular trauma. IGATES was created to collect robust data to refine a methodology for prognostication and management of ocular trauma.
The objective of this study was to report on the demographics and nature of the injury and associations of SVL for OGI’s utilizing data from IGATES.
Materials and methods
Development of software platform
A data entry platform was developed to address the broad ranging epidemiology and treatment of ophthalmic (ocular and adnexal) trauma. A steering committee, which was composed of A.H, R.A, F.W, and A.R, performed a review of the literature to identify data collection points and a process for data. The steering committee, through consensus, then determined the target population and methods for data collection, quality review, and management of data.
The secure encrypted platform was programmed in Amazon Cognito® by D.V.G and R.A and maintained and stored on servers at the Tan Tock Seng Hospital, Singapore. The full data set was only available to the core research team, through a unique individual password. Only de-identified data was able to be downloaded or stored outside the server. This web-based form provided users with explanations and prompts to facilitate accurate data collection [18].
Data collection
The sites contributing data were invited to participate through the ocular trauma societies in India (Indian Society of Ocular Trauma) and the Asia Pacific (Asia Pacific Ophthalmic Trauma Society). These societies contacted sites from their respective memberships, including India, Nepal, Singapore, Australia, Argentina, Malaysia, China, Indonesia, and the United States of America (USA). Participation was voluntary. Data was collected from a total of 13 hospitals in India, Singapore, Australia, Pakistan, Malaysia and the USA (see IGATES 1 Study Group). The collaborating principal investigator (PI) from each center provided copies of Institutional Review Board (IRB)/Ethics committee approval. Patient identifiers were omitted to ensure patient anonymity and privacy.
Measures to maintain data quality included clear inclusion and exclusion criteria, as noted in the definitions below. Any patients with missing data were identified during initial quality assessment, and collaborators were prompted to cross-check data with clinical notes.
The retrospective cohort study of patients with ocular trauma was conducted using IGATES registry. The study was conducted in accordance with the tenets of the Declaration of Helsinki. Data included from Australia were approved for inclusion by the South Eastern Sydney Local District Human Research Ethics Committee (HREC reference number 15/018).
The details of the participating centers and parameters collected are provided in Appendices 1 and 2, respectively.
Definitions
The diagnostic criteria for ocular trauma used in IGATES were patients with an OGI with or without adnexal involvement. Patients who satisfied the diagnostic criteria and received treatment as an inpatient or outpatient with the following inclusion criteria between April 2009 and April 2020 were included in the study: (1) availability of patient’s medical records with details of their ophthalmic examination and (2) completion of a minimum of 2 weeks’ follow-up. Patients who presented for a pre-existing injury were excluded.
Follow-up data were recorded when the patient re-attended, with periods for follow-up recorded at 1–2 weeks, 1 month, 3 months, and 6 months, 12 months, 18 months, and 24 months, when available. The final outcome was determined at the last visit, and the reason for conclusion of treatment or non-attendance noted if known OGIs were classified according to Birmingham Eye Trauma Terminology System (BETTS) [19]. Zone III injuries were defined as those injuries extending into the sclera more than 5 mm posterior to the corneoscleral limbus. For bilateral eye injuries, data were collected for the more severely injured eye, defined as the eye with the worse visual acuity (VA) at presentation, and if both eyes had a similar vision, the right eye was chosen.
VA was recorded at each visit and last follow-up appointment. Time to presentation was defined as the time from injury occurring to first presentation. Visual impairment was classified using the World Health Organization criteria, [20] as mild visual loss (< 6/12), moderate (< 6/18), severe (< 6/60), or blindness (<3/60). Delay in presentation was defined as presentation >24 h following injury.
The steering committee reviewed and agreed on the categories for the location, object, and mechanism of injury, which were grouped further for analysis. Locations of injury were classified as “industrial” for all work-related injuries; “home” for when an injury occurred at their place of residence; “outdoors/public area” which included schools, sporting venues, and shops; and “other” for remaining locations. Objects associated with the trauma were classified as sharp metal, blunt (which included metal, rubber, stone, and wood), other sharps (which included wood and tiles or ceramics), and other (which included consumer products such as pens and knives, falls onto surfaces, body parts, thermal including fireworks, animal related, glass, chemicals, and sports equipment). The mechanism of injury was classified as blunt, road traffic accident, projectile, unknown, or other (which included fall, burn thermal, burn chemical, assault, animal/insect bight or sting).
Statistical analysis
Descriptive statistics, frequencies and percentage, mean, and standard deviation were reported for “all included patients.” For the cohort with complete data, “complete data patients”, the effect of demographic and clinical variables, mechanism of injury, and object causing injury were assessed on the dichotomous visual status at presentation as well as following treatment, using univariate analysis. Patient visual outcomes were further stratified into a binomial outcome variable of either “SVL” (VA ≤ 6/60) or “no SVL” (VA > 6/60) [20]. Variables with p < 0.20 were considered for multiple logistic regression (MLR) analysis and removed in stepwise backwards elimination. Statistically significant variables from univariate analysis were incorporated into the MLR model. The outcome variables used were vision at presentation and final VA. Model fit was evaluated with Hosmer-Lemeshow test and area under curve (AUC) for MLR to ascertain the predictive value of the model. All analyses were performed using SPSS version 20.0 (IBM Corp, USA), and the statistical significance was 5%.
Results
Demographic characteristics
Seven hundred forty-six patients (746 eyes) with OGIs from 7 countries were included (Fig. 1). The median age of included patients was 35.9 ± 20.0 years with most patients in the 21- to 40-year-old age group (47.9%), and 640 (85.8%) males. The majority of injuries were unilateral; with 414 (52.7%) left eye, 345 (44.0%) right eye, and 13 (1.7%) bilateral injuries.
Patient follow-up data was recorded at 1–2 weeks (287), 1 month (89), 3 months (93), and 6 months (146), 12 months (74), 18 months (18), and 24 months (29) with average follow-up period 4.67 months and a total of 89 patients (11.9%) lost to follow-up. Complete data were available for 354 patients, and this group had a median age of 35.7 ± 20.1 years. Males 21- to 40 years old accounted for 56.1% (183/326) and females younger than 40 years old 32.1% (9/28, 32.1% each); this was significantly more than in the other age groups (p = 0.0381).
Patients <20 years old were highly represented in India (41.1%, n = 97/236) and Pakistan (49.1%, n = 27/55) and 21- to 40-year-olds in Australia (37.4%, n = 77/206), Malaysia (80.0%, 24/30), and Singapore (74.4%, n = 152/207). Patient demographics stratified by country are detailed in Tables 1 and 2.
One hundred seventy-three (23.2%) patients had delayed presentation with patients from Pakistan (50.9%) and India (36.9%) representing the highest proportion.
Mechanism, location, and object of injury
A wide range of objects were associated with an OGI with sharp metal (n = 235); blunt metal (n = 76); sharp glass (n = 35); body part, e.g., finger (n = 35); sharp wood (n = 32); and blunt wood (n = 27) the largest contributors. Other items responsible included stationeries—pens and pencils (n = 11), scissors (n = 2), book (n = 2), and eraser (n = 1)—and animals: cow/bullock horns (n = 6), insects (n = 10), birds (n = 4), dog (n = 1), and cat (n = 1). Sports-related activities were responsible for 38 OGIs with soccer, badminton, and cricket the most common sports.
Overall, the main mechanism of injury was via a projectile, in 292 (39.14%), followed by blunt trauma (19.2%), road traffic related (3.0%), and others (13.9%) (see Table 1).
The leading location where the injuries occurred was an industrial setting in 41.4%, at home in 26.3%, or outdoor setting in 19.7%, n = 147/746. When examining object responsible by location, the largest contributors to industrial injuries were sharp objects (51.7%) including those composed of metal, plastic, tiles, and/or wood. While in the home, blunt and sharp metal objects represented the largest contributors (19% and 18%, respectively). Injuries in the home associated with OGIs included falls, fireworks, body parts, glass, and wood objects. Outdoor contributors to OGI were blunt (13%) and sharp (14%) objects including wood, glass, and stone, with cow horns and tails and fishing hooks and sinkers also identified.
By geography, industrial injuries were responsible for the largest proportion of injuries in Singapore (74.9%, n = 155/207) and home-related injuries the largest proportion in India (41.1%, 97/236). Sharp metal objects were responsible for the highest proportion of injuries in Australia (31.1%, n = 64/206), Malaysia (66.7%, n = 20/30), Pakistan (56.4%, n = 31/55), and Singapore (42.5%, n = 88/207) (see Table 2).
Clinical features
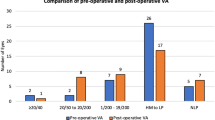
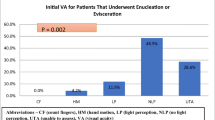
VA at presentation was recorded in 709 patients, with the majority of patients (64.0%) (n = 454/709) being blind with normal VA in 17.2% (n = 122/709), mild (2.7%, n = 19/709), moderate (11.7%, n = 83/709), or severe visual loss (4.4%, n = 31/709).
Patient follow-up data was recorded at 1–2 weeks (n = 287), 1 month (n = 89), 3 months (n = 93), and 6 months (n = 146), 12 months (n = 74), 18 months (n = 18), and 24 months (n = 29). The average follow-up period was 4.7 months, and in total 89 patients (11.9%) were lost to follow-up. VA at final follow-up was recorded in 730 patients. The majority of the patients, 44.8% (n = 327/730), were blind, with normal VA in 26.8% (n = 196/730), and mild (10.8%, n = 79/730), moderate (13.2%, n = 96/730), and severe visual loss (4.4%, n = 32/730).
The presence of RAPD, zone III injury, IOFB, and eyelid injury were observed in 50 (6.7%), 55 (7.4%), 97 (13.0%), and 87 (11.7%) of patients at presentation, respectively (Table 1). The highest proportion of patients with zone III injury, IOFB, and eyelid injury was found in India (13.3%, 33.3%. 33.33%, respectively), and RAPD the highest in the USA (66.7%). Using Pearson’s chi-square test, females were significantly more likely to present with an RAPD than males (32.1%, 14.7%, p = 0.0161).
Severe vision loss
Across the complete cohort, “all included patients,” the proportion of patients with SVL at presentation was 64.0% (454/709) and 46.1% (327/709) at final follow-up. For the cohort with VA data at presentation and final follow-up, “complete data cohort,” a statistically significant improvement in vision was observed (p value <0.0001). Comparing presenting vision to final visual outcomes for the complete data cohort, 127/354 (35.9%) patients had SVL at final follow-up (Table 3). However, at final follow-up, 3 patients who had moderate vision loss at presentation were blind and 2 patients with SVL at presentation were blind. A delay in presentation was associated with a 1.60 times [95% CI: 1.09–2.34; p = 0.02] higher risk of SVL than those presenting within 24 h (Table 4).
The risk of SVL at final follow-up was estimated for each parameter through univariate analysis for the complete data cohort (Table 5). The risk of SVL at final follow-up was found to be significantly associated with age, gender, location of injury and object of injury. Patients aged over 60 years were at 3.39 times higher risk of blindness [95% CI: 1.953–5.887; p < 0.0001] compared to the teenage group. The risk associated with males was significantly lower at 0.42 [95% CI: 0.27–0.66; p = 0.0001] compared to females.
Industrial-related ocular trauma had a lower rate of SVL than that of home related at final follow-up, OR 0.48 [95% CI: 0.328–0.687; p = 0.0007]. The observation was similar for sharp metallic objects. The presence of a RAPD had significantly higher odds of SVL with OR of 7.49 [95% CI: 4.55–12.33; p < 0.0001] as compared to the absence of RAPD. Similarly, for zone III injury, the odds were 4.13 times [95% CI: 2.29–7.46; p < 0.0001] higher, while those with IOFB had 1.63 times [95% CI: 0.06–2.50; p = 0.026] higher risk of SVL even after treatment. Patients with eyelid injury had 3.92 [95% CI: 2.43–6.34; p < 0.0001] times higher risk of SVL.
The variables with significant relevance to SVL in univariate analysis were entered in a MLR model to obtain adjusted risk estimates using the 354 patients with complete data (Table 6). Model fitness was evaluated using Hosmer-Lemeshow test, which resulted in a p value of 0.49 indicating good fitness. Receiver operating characteristic (ROC) analysis was performed on model scores (predicted probabilities) to determine model strength (Fig. 2a and b). AUC was 0.71 [95% CI: 0.66–0.76; p < 0.0001], which was acceptable and supported the model fitness.
For SVL at presentation, age categories 21–40 and 41–60 years showed significant reduction in adjusted risk with ORs of 0.39 [95% CI: 0.20–0.73; p = 0.0036] and 0.31 [95% CI: 0.14–0.68; p = 0.004], respectively, compared to the teenage group. Delayed presentation following an injury had significantly increased adjusted risk of SVL with OR 1.82 [95% CI: 1.06–3.15; p = 0.031]. Presence of RAPD had increased adjusted risk of SVL with OR of 9.20 [95% CI: 3.10–27.25; p = 0.0001].
The MLR was also carried out for “final” SVL (Table 6). The Hosmer-Lemeshow test suggested a good model fit (p = 0.609). Moreover, the AUC was 0.76 [95% CI: 0.70–0.81; p < 0.0001], which was acceptable and supported the model fitness. The adjusted risk associated with males was significantly lower at 0.33 [95% CI: 0.140–0.83; p = 0.018] as compared to females. The adjusted risk for the presence of an RAPD was significantly higher at 6.96 [95% CI: 3.33–14.540; p < 0.0001] compared to absence of RAPD. Eyelid injury had 3.61 [95% CI: 1.68–7.75; p = 0.001] increased adjusted risk of SVL.
Discussion
IGATES is a secure online registry available internationally for the collection of ocular trauma data. OGI occurred more frequently in males in industrial settings and females at home. Three hundred twenty-seven (48.8%) patients had SVL after an OGI across 13 sites from 7 countries. Adjusted risk of post-treatment SVL was significantly higher for females, and presence of an RAPD or eyelid injury was associated with increased risk of SVL.
Patients 41–60 years (47.1%) and over 61 years (69.6%) had the highest rate of final SVL. Eye injuries in elderly patients have recently been identified as increasing and frequently associated with falls [21, 22] and a history of intraocular surgery [23]. In our study, female gender and older age were significantly associated with increased risk of SVL following OGI.
Delay in presentation has been associated with poorer visual outcomes following treatment for ocular trauma. In our study, a 24-h delay leads to increased risk of SVL at presentation but there was no significant association with SVL at final follow-up. This finding may be related to the fact that the severe injuries were more likely to present without delay enabling treatment to be instituted.
A male predominance was found consistent with previous studies [21, 22, 24, 25], with working-age males most affected. Working with metal has been frequently reported as a leading contributor to OGIs [23], and almost 1/3 of injuries in our study were due to sharp metal. Ocular trauma occurred more commonly in the home in India (41.1%) and Pakistan (38.3%) and in industrial locations in Australia (32.0%), Malaysia (60.0%), and Singapore (74.9%). In Singapore children suffer eye injuries commonly at home [26], whereas working-age adults in Australia are commonly injured at work [23].
Females were more likely to be injured at home, be subject to a blunt injury, and present with an RAPD. These findings, to our knowledge, have not been reported by prior studies [21, 27, 28]. Due to the retrospective nature of our data collection, the reasons for this finding are not clear. Females injured in the home may be less likely to seek treatment unless the injuries are severe; to investigate this and institute preventative measures, prospective data is needed.
The participating centers varied in terms of social factors and demographic. Gross domestic product (GDP), while only one measure relating to standard of living, varied significantly, from 1284 ($USD per capita) in Pakistan, $2099 India, $11,414 in Malaysia to $55,060 in Australia, $65,233 in Singapore, and $65,297 in the USA [29] Median age across the included countries varied significantly with Pakistan (22 years old), India (28.7 years old), and Malaysia (29.2 years old) younger overall than the higher GDP countries of Australia, Singapore, and the USA (37.5, 35.6, and 38.5 years old, respectively). Factors such as GDP and population distribution by age and gender influence the distribution of OGIs and should be considered in the development of prevention strategies. For example, the countries with lower GDP may have less structured regulations and standards relating to the use of eye protection in industrial environments. The high rate of OGIs in industrial environments in Singapore (74.9%) conflicts with this hypothesis, highlighting the influence of other factors, e.g., potential lack of reinforcement of regulations.
A variety of objects were associated with OGIs with the geography and location of the injury influencing the type of object. Sharp metal was a significant contributor in industrial locations, while stationery, animals, and sporting equipment were reported with injuries at home and outdoors. Future studies with more rigorous methodology and including a larger number of institutions internationally will enable trends associated with OGIs to be identified to inform strategies for their prevention.
Retrospective data collection limitations included incompleteness of data and variable time points for follow-up, making it difficult to draw conclusions regarding risk factors. In particular, 73 patients had no VA data reported and no active follow-up was undertaken. Assault-related ocular trauma contributed to almost 25% eye injuries in the USA in the period 2001 to 2014 [21]. In our study, assault was only reported in a small number of patients (3.3%). Reporting of assault may have been limited by the retrospective nature of our data collection.
Limited information relating to eye injury prevention measures, such as eye protection, was reported. Only 39 patients were recorded as wearing eye protection, with 9 determined as “non-safety” glasses, e.g., sunglasses or regular spectacles, indicating a lack of understanding of the need for and what is safety eyewear. Education about what constitutes eye protection, both for patients and practitioners, may be needed. Countries in this study had a diverse range of occupational health and safety laws and their enforcement in regard to the use of eye protection in the workplace and standards for eye protection. For example, employers have a duty of care to provide eye protection complying with standards in Australia [30] and the USA [31]. Future studies could identify the impact of regulations relating to eye protection to guide and support evidence-based prevention strategy for ocular trauma.
Participant bias may also have been introduced as it is difficult to know if all patients with trauma were entered at each center. Furthermore, as we rely on patient’s self-reported information relating to the circumstances of the injury, this may have introduced reporting bias.
Utilizing IGATES registry, current trends in OGIs and the associated SVL have been highlighted. This data could be used to develop preventative strategies. Prospective and uniform data collection in future studies could further inform such strategies.
Data availability
The full data set was only available to the core research team, through a unique individual password.
Change history
08 September 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00417-021-05408-5
References
Thylefors B (1992) Epidemiological patterns of ocular trauma. Aust N Z J Ophthalmol 20(2):95–98
Negrel AD, Thylefors B (1998) The global impact of eye injuries. Ophthalmic Epidemiol 5(3):143–169
Munoz E (1984) Economic costs of trauma, United States, 1982. J Trauma 24(3):237–244
Luo H, Beckles GL, Fang X, Crews JE, Saaddine JB, Zhang X (2012) Socioeconomic status and lifetime risk for workplace eye injury reported by a us population aged 50 years and over. Ophthalmic Epidemiol 19(2):103–110
Katz J, Tielsch JM (1993) Lifetime prevalence of ocular injuries from the Baltimore eye survey. Arch Ophthalmol 111(11):1564–1568
Long J, Mitchell R (2009) Hospitalised eye injuries in New South Wales, Australia. Open Epidemiol J 2:1–7
Leonard JC (2019) National trends in ocular injury: differing studies, common call to action. JAMA Ophthalmol 137(1):56–57
Yardley AE, Hoskin AK, Hanman K, Sanfilippo PG, Lam GC, Mackey DA (2017) Paediatric ocular and adnexal injuries requiring hospitalisation in Western Australia. Clin Exp Optom 100(3):227–233
Kuhn F, Mester V, Berta A, Morris R (1998) Epidemiology of severe eye injuries. United States eye injury registry (USEIR) and Hungarian eye injury registry (HEIR). Ophthalmologe. 95(5):332–343
Low L, Hodson J, Morris D, Desai P, MacEwen C (2017) Socioeconomic deprivation and serious ocular trauma in Scotland: a national prospective study. Br J Ophthalmol 101(10):1395–1398
Kuhn F, Maisiak R, Mann L, Mester V, Morris R, Witherspoon CD (2002) The ocular trauma score (OTS). Ophthalmol Clin N Am 15(2):163–165 vi
Agrawal R, Shah M, Mireskandari K, Yong GK (2013) Controversies in ocular trauma classification and management: review. Int Ophthalmol 33(4):435–445
Shah MA, Agrawal R, Teoh R, Shah SM, Patel K, Gupta S et al (2017) Pediatric ocular trauma score as a prognostic tool in the management of pediatric traumatic cataracts. Graefes Arch Clin Exp Ophthalmol 255(5):1027–1036
Hoskin AK, Watson SL, Mackey DA, Agrawal R, Keay L (2019) Eye injury registries - A systematic review. Injury 50(11):1839–1846. https://doi.org/10.1016/j.injury.2019.07.019
Guerra García RA, García DP, Martínez FE, Columbié Garbey YE, Martínez RR (2013) The Cuban Ocular Trauma Registry. J Clin Exp Ophthalmol 4:276. https://doi.org/10.4172/2155-9570.1000276
Agrawal R, Gunasekeran DV, Grant R, Agarwal A, Kon OM, Nguyen QD et al (2017) Clinical features and outcomes of patients with tubercular uveitis treated with antitubercular therapy in the collaborative ocular tuberculosis study (COTS)-1. JAMA Ophthalmol 135(12):1318–1327
Tan JCK, Ferdi AC, Gillies MC, Watson SL (2019) Clinical registries in ophthalmology. Ophthalmology. 126(5):655–662
Gunasekeran DV, Agrawal R, Testi I, Agarwal A, Mahajan S, Nguyen QD et al (2020) Lessons in digital epidemiology from COTS-1: coordinating multicentre research across 10 countries using operational and technology innovation to overcome funding deficiencies. Ocul Immunol Inflamm:1–7
Kuhn F, Morris R, Witherspoon CD, Mester V (2004) The Birmingham eye trauma terminology system (BETT). J Fr Ophtalmol 27(2):206–210
World Health Organisation. Blindness and vision impairment. Key Facts [Website]. [updated 8th October 2019; cited 2019. WHO Definition of Blindness]. Available from: https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment#:~:text=Mild%20%E2%80%93visual%20acuity%20worse%20than,acuity%20worse%20than%203%2F60. Acessed 20th May 2021
Iftikhar M, Latif A, Farid UZ, Usmani B, Canner JK, Shah SMA (2019) Changes in the incidence of eye trauma hospitalizations in the United States from 2001 through 2014. JAMA Ophthalmol 137(1):48–56
Gunasekeran DV, Tan P, Goh ES (2014) Evaluation and management outcomes of orbital wall fractures presenting to a tertiary hospital in SIngapore. Invest Ophthalmol Vis Sci 55(13):2785
Beshay N, Keay L, Dunn H, Kamalden TA, Hoskin AK, Watson SL (2017) The epidemiology of open globe injuries presenting to a tertiary referral eye hospital in Australia. Injury. 48(7):1348–1354
Court JH, Lu LM, Wang N, McGhee CNJ (2019) Visual and ocular morbidity in severe open-globe injuries presenting to a regional eye Centre in New Zealand. Clin Exp Ophthalmol 47(4):469–477
Tovell A, McKenna K (2018) Eye injuries in Australia, 2010–11 to 2014–15. Injury research and statistics series no. 194. . Canberra: AIHW. Contract No.: Cat. no. INJCAT 114
Abbott J, Shah P (2013) The epidemiology and etiology of pediatric ocular trauma. Surv Ophthalmol 58(5):476–485
Chang YS, Teng YT, Huang YH, Liu ML, Hung JH, Hsu SM et al (2018) Major ocular trauma in Taiwan: 2002-2004 versus 2012-2014. Sci Rep 8(1):7081
Northey LC, Bhardwaj G, Curran S, McGirr J (2014) Eye trauma epidemiology in regional Australia. Ophthalmic Epidemiol 21(4):237–246
OECD.org. Organisation for Economic Co-operation and Development 2021 [cited 2021 28th May 2021]. Available from: https://data.oecd.org/gdp/gross-domestic-product-gdp.htm. Acessed 20th May 2021
AS/NZS 1337.1 Personal eye protection Part 1: Eye and face protectors for occupational applications. Sydney: Standards Australia/ Standards New Zealand, 2010
ANSI Z87.1 American National Standard for Occupational and Educational Personal Eye and Face Protection Devices. American National Standards Institute, Inc. 2010
Acknowledgments
We thank Dr. Dhananjay Raje and Ms. Moumita Chakraborty, Data Analysis Group, MDS Bio-Analytics, Nagpur, India, for their assistance in clinical information analysis.
Code availability
Secure encrypted platform was programmed in Amazon Cognito® by D.V.G and R.A and maintained and stored on servers at the Tan Tock Seng Hospital, Singapore.
Funding
Annette Hoskin is the recipient of an NHMRC PhD Scholarship.
Stephanie Watson is a Sydney Medical School Foundation Fellow.
Lisa Keay has an NHMRC Career Development Fellowship.
Dinesh Visva Gunasekeran is a Commonwealth Fellow (Innovation).
These funding organizations had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Consortia
Contributions
All authors made substantial contributions to the study conception or design. Material preparation and data analysis were performed by Rupesh Agrawal, Annette Hoskin, Lisa Keay, and Stephanie Watson. The first draft of the manuscript was written by Annette Hoskin, and all authors commented on previous versions of the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethics Committee approval was obtained by each center. Data included from Australia were approved for inclusion by the South Eastern Sydney Local District Human Research Ethics Committee (HREC reference number 15/018).
Consent for publication
Not applicable, all information is anonymized, and the submission does not include images that may identify the person.
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised. Collaborators are now corrected.
Supplementary Information
ESM 1
(DOCX 15 kb)
Appendix
Appendix
IGATES 1 Study Group
Members of IGATES Study Group | Participating centers | Country |
|---|---|---|
Dr. Sundaram Natarajan | Aditya Jyot Eye Hospital, India | India |
Dr. Satish Gooty, Dr. Arjun, Dr. Pravallika, Dr. Tarannum | Anand Eye Institute, Hyderabad, India | India |
Dr. R Kim, Dr. Chitaranjan Mishra | Aravind Eye Hospital, Madurai, India | India |
Dr. Meenu Chaudhary | B.P. Koirala Lions Center for Ophthalmic Studies, Nepal | Nepal |
Dr Andres Rousselot | Consultorios Oftalmológicos Benisek Ascarza, Capital Federal, Buenos Aires, Argentina | Argentina |
Dr. Shreya Mehul Shah, Dr. Mehul Shah | Drashti Nethralaya Eye Hospital, Dahod, India | India |
Dr. Marian Pauly, Dr. Giridhar | Giridhar Eye Institute, Kochi, Kerala, India | India |
Dr. Hussain Khaqan | Lahore General Hospital, Lahore, Pakistan | Pakistan |
Dr. Anadi Khatri | Lumbini hospital, Kedia Eye Hospital, Birat Eye Hospital, Kakarvitta Eye Centre, Nepal | Nepal |
Dr. Chaitra Jayadev, Dr. Kushagra Jain | Narayana Nethralaya, India | India |
Dr. Rupesh Agrawal, John Kan, Rebecca Low, Dinesh VG | National Healthcare Group Eye Institute, Tan Tock Seng Hospital, Singapore | Singapore |
A/Prof Gangadhara Sundar, Prof Caroline Chee, Dr. Victor Koh | National University Healthcare System, Department of Ophthalmology, Singapore | Singapore |
Dr. Rekha Khandelwal | NKP Save Institute of Medical Sciences, Nagpur, India | India |
Dr. Alok Sen | Sadguru Netra Chikitsalaya, India | India |
Dr. Parveen Sen | Sankara Nethralaya, Chennai, India | India |
Dr. Shakeen Singh | Shakeen Singh Eye Hospital, India | India |
Dr. Amer Awan | Shifa International Hospital, Rawalpindi and Islamabad, Pakistan | Pakistan |
Dr. Ashok Grover, Dr. Anurag Mittal | Sir Ganga Ram Hospital, India | India |
Ms. Annette Hoskin, Prof Stephanie Watson | The University of Sydney, Save Sight Institute, Discipline of Ophthalmology, Sydney Medical School, Sydney, New South Wales, Australia. | Australia |
Dr. Eli Pradhan | Tilganga Institute of Ophthalmology, Nepal | Nepal |
Dr. Tengku Ain Kamalden, Dr. Maftuhim Addenan, Dr. Hannie Ch’ng, Dr. Fatin Nadia Zamawi | University of Malaya Medical Centre, Kuala Lumpur, Malaysia | Malaysia |
Assistant Professor Dr. Fasika Woreta | Wilmer Eye Institute, Johns Hopkins University School of Medicine, Maryland, USA | USA |
Rights and permissions
About this article
Cite this article
Hoskin, A.K., Low, R., Sen, P. et al. Epidemiology and outcomes of open globe injuries: the international globe and adnexal trauma epidemiology study (IGATES). Graefes Arch Clin Exp Ophthalmol 259, 3485–3499 (2021). https://doi.org/10.1007/s00417-021-05266-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05266-1