Abstract
Purpose
To investigate and compare the clinical features of cytomegalovirus (CMV) retinitis after solid organ transplantation (SOT) and hematopoietic stem cell transplantation (HSCT) and to determine the poor prognostic factors.
Methods
Patients consulted to the ophthalmology department for CMV viremia after transplantation between March 2008 and February 2018 and followed for more than 6 months were analyzed. Medical records regarding demographic, serologic, and ocular characteristics were compared between the SOT and HSCT groups. Factors associated with poor visual outcomes were determined with logistic regression.
Results
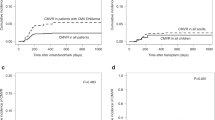
CMV retinitis developed in 11.3% of patients with CMV viremia following transplantation. In the SOT group (25 eyes/18 patients) and the HSCT group (33 eyes/21 patients), CMV retinitis occurred at 5.8 months and 3.7 months post-transplantation, respectively. Mortality was significantly higher in the HSCT group (52.4% vs. 5.6%, P < 0.001). During the mean 11.7 months of follow-up, visual acuity tended to be aggravated (P = 0.087) despite antiviral treatment, which was especially notable in the SOT group (P = 0.028). Six eyes (10.3%) underwent vitrectomy due to retinal detachment, most of which (5 eyes) were in the SOT group. Multivariate logistic regression analysis showed that the presence of concurrent CMV disease (OR = 14.11, P = 0.009) and foveal involvement (OR = 114.85, P = 0.001) were poor prognostic factors.
Conclusion
Clinical manifestations of CMV retinitis differed between the HSCT and SOT group. Concurrent CMV diseases and foveal involvement were associated with poor visual outcomes in CMV retinitis following transplantation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Cytomegalovirus (CMV) retinitis is a severe retinal disease usually observed in immunocompromised patients that may result in visual loss unless timely diagnosis and proper treatment are made [1, 2]. Although the retina is the most common site of CMV disease in patients with acquired immune deficiency syndrome (AIDS), the incidence of CMV retinitis in such patients has declined with the advancement of highly active antiretroviral therapy [3, 4]. On the other hand, the increasing number of transplant recipients is predisposed to a higher incidence of CMV retinitis and CMV diseases due to their prolonged survival [5,6,7].
Organ transplantation can be largely divided into solid organ transplantation (SOT) [8, 9] and hematopoietic stem cell transplantation (HSCT) [10, 11]. In general, patients with HSCT and established CMV diseases tend to present with poor systemic prognosis, which might be attributed to higher CMV viral load, lymphopenia, or CMV-specific T cell immunodeficiency [12]. Accordingly, patients who undergo HSCT have been shown to have a higher incidence of CMV pneumonia and related mortality rate than those who undergo SOT [13].
Numerous studies have described the clinical features of CMV retinitis in patients undergoing either HSCT or SOT; however, reports on side-by-side comparisons of the two groups in terms of CMV retinitis remain scarce [2, 14]. In our present study, we investigated the clinical features of CMV retinitis in transplant recipients and compared them according to the type of transplantation, i.e., SOT and HSCT. We also determined the factors associated with poor visual outcomes in these patients.
Materials and methods
Study subjects
In this retrospective, observational, single-center study, we reviewed the medical records of all consecutive patients diagnosed with CMV retinitis following SOT or HSCT between March 2008 and February 2018 at Asan Medical Center (Seoul, Korea). During this 10-year period, a total of 344 transplant recipients were diagnosed with CMV viremia serologically or by blood polymerase chain reaction (PCR) and were referred to ophthalmologists for the screening of CMV retinitis. Among these patients, only those who were confirmed to have CMV retinitis by retinal specialists and were followed for more than 6 months after the diagnosis were included in the present analysis.
Criteria for exclusion were as follows: patients with extremely poor systemic conditions that hinder proper ocular examination; patients with a follow-up period of less than 1 month after the diagnosis of CMV retinitis. All procedures of this study conformed to the principles of the Declaration of Helsinki, and the study was approved by the Institutional Review Board of Asan Medical Center (2018-0815).
Screening for CMV viremia and protocols for systemic preemptive therapy and ocular screening tests
Patients undergoing transplantation at Asan Medical Center are routinely checked for the presence of CMV viremia in their peripheral venous blood for a certain period of time after the transplantation. Blood examinations were carried out either with CMV antigenemia assay (Light Diagnostics CMV pp65 antigenemia assay; Millipore Corp., Temecula, CA, USA) or with automated, real-time, quantitative polymerase chain reaction (PCR) with a detection threshold of 500 copies/ml. Generally, in the SOT group, the blood CMV check-up was performed every week in the first postoperative month, biweekly in the next month, and subsequently every 4 weeks until the 6th postoperative month. In the HSCT group, the blood CMV check-up was performed every week from the 3rd postoperative week to the 3rd postoperative month and subsequently every 4 weeks until the 6th postoperative month. A detailed screening protocol for the presence of CMV viremia was individualized on the basis of the transplanted organ, patient's immune status, and previous results of CMV viremia. However, the systemic treatment strategy was not significantly different between SOT and HSCT groups. Systemic antiviral treatments, such as intravenous ganciclovir (10 mg/kg/day) or oral valganciclovir (1800 mg/day), were started for patients with positive CMV results. The positive thresholds for the systemic treatment were CMV antigenemia (> 50/200,000 cells) or positive CMV PCR results in both SOT and HSCT groups. Systemic foscarnet (60 mg/kg IV every 8 h or 90 mg/kg every 12 h) was used in cases in which the systemic ganciclovir treatment could not be used because of severe neutropenia or a ganciclovir-resistant CMV infection. Simultaneously, as the systemic therapy began, the patients’ positive results in CMV antigen or CMV PCR tests were referred to ophthalmologists for fundus examination to search for retinal lesions resulting from CMV infection. Or, patients with negative results were also referred to the ophthalmology department when they had any ocular symptoms.
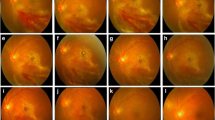
Ocular evaluation and treatments
All patients showing possible lesions of CMV manifestations at the primary screening were referred to retinal specialists and thoroughly examined. At the initial and following visits, all patients underwent detailed ophthalmologic examinations that included a review of ophthalmologic history, measurement of visual acuity, slit-lamp biomicroscopy, and funduscopic examinations through dilated pupils by retinal specialists. Steering fundus photograph was used from March 2008 to February 2012 and ultra-widefield fundus photography (Optos 200Tx system, Optos plc, Dunfermline, UK) was used from March 2012 to February 2018.
CMV retinitis was treated with systemic antiviral therapy as described above. Intravitreal ganciclovir injection (2 mg/0.1 ml) was added in the following circumstances: (1) CMV retinitis not improving after systemic ganciclovir/foscarnet treatment; (2) zone 1 involvement of the CMV retinitis; (3) systemic ganciclovir treatment could not be used because of severe side effects of the antiviral treatment (e.g., severe neutropenia). The number and interval of ganciclovir injection were determined depending on the treatment response as well as the size and location of the lesion. Ocular injection was not performed in patients who refused treatment because of short remaining life expectancy or those with general conditions too poor to expect adequate coordination for injection procedures.
Analysis
The following variables were analyzed in the cohort of patients with documented CMV viremia: (1) demographics and systemic disease-associated variables (i.e., age, sex, total follow-up duration, time from organ transplantation to diagnosis of CMV retinitis, prevalence of CMV retinitis among CMV viremia, concurrent CMV infection, such as CMV gastroinstestinal disease or CMV pneumonia, in which the presence of CMV is detectable in clinical specimens, presence of graft-versus-host disease, transplanted organ, underlying systemic disease, and mortality); (2) serologic variables (i.e., peak/preceding level [just before the diagnosis of CMV retinitis] of CMV DNA PCR, peak/preceding level of CMV antigenemia assay, time from initial viremia to the diagnosis of CMV retinitis, duration of positive results in CMV viremia tests, and absolute neutrophil count (ANC) at diagnosis); and (3) ocular characteristics and ocular treatment-related variables (i.e., visual acuity at baseline and each visit, presence of macular involvement, presence of other ocular complications, and the number and timing of intravitreal ganciclovir injections and/or vitrectomy). Involved zones of CMV retinitis were categorized into zones 1, 2, and 3 (from the posterior pole to the peripheral retina) as described in a previous study from our group[15].
Descriptive statistics were evaluated in order to analyze the baseline characteristics of subjects and expressed as number and percentage for categorical variables and median (1st quartile–3rd quartile) for continuous variables. For comparison between the SOT group and the HSCT group, Fisher’s exact test was used for categorical variables and the Mann-Whitney U test was used for continuous variables. Factors associated with poor final visual outcome (< 20/200) were analyzed as well. Odds ratios (ORs) for associations among potential risk factors were obtained using the binary logistic regression analysis. Univariate analyses were separately performed for each variable and the variables with probability values less than 0.1 in the univariate analysis were included in the multivariate regression analysis model. A forward elimination process was used to develop the final multivariate model, and ORs with 95% confidence intervals (CIs) were calculated. P values lower than 0.05 were considered to denote statistical significance. All statistical analyses were performed using SPSS version 21.0 software (IBM Corp., Armonk, NY, USA).
Results
A total of 58 eyes of 39 patients were included in the analysis (SOT, 25 eyes of 18 patients; HSCT, 33 eyes of 21 patients). The prevalence of CMV retinitis among the patients with serologically proven CMV viremia was 11.3% (39 out of 344), which was higher in the HSCT group than in the SOT group (15.4% vs. 8.7%, P = 0.052). The basic demographic information of both groups is presented in Table 1. The median age was 39.0 [IQR, 19.0–55.0] years and the HSCT group was younger than the SOT group (19.0 [9.0–41.5] vs. 52.5 [41.8–58.5] years, P < 0.001). After the diagnosis of CMV retinitis, the entire study cohort was followed for 11.7 [2.6–26.1] months, and the follow-up period was shorter in the HSCT group than in the SOT group (3.6 [1.6–14.6] vs. 20.4 [11.5–44.3] months, P = 0.026). The median time from transplantation to CMV retinitis diagnosis was 126.0 [76.0–239.0] days.
The earliest onset of CMV retinitis was observed at 36 days in the HSCT group and 113 days in the SOT group, and the median days from transplantation to CMV retinitis were 112.0 and 174.5, respectively (P = 0.283). Concurrent CMV diseases, such as gastrointestinal CMV diseases and CMV pneumonia, were observed in 2 and 3 patients in the HSCT group, respectively. GVHD was more frequently present in patients with HSCT (42.9% vs. 5.6%, P = 0.023) and treated with steroid and immunosuppressant therapy. The mortality rate during the follow-up period was 30.8% in the entire cohort and was significantly higher in the HSCT group (52.4% vs. 5.6%, P < 0.001). In order to rule out age-related effects, we compared the adult patients in the HSCT group (18 eyes of 12 patients) with the SOT group and found that the results were similar to those acquired in the HSCT group as a whole. The underlying diseases and transplanted organs are listed in Supplementary Table 1. Among the SOT group, kidney (38.9%) and liver (33.3%) were the most common organs for transplantation.
Serologic test results for CMV are shown in Supplementary Table 2. CMV DNA PCR examination presented the quantitative difference between the two groups; the peak level (P < 0.001) and the preceding level (P = 0.002) were higher in the HSCT group. In CMV antigenemia assay, the level of CMV antigen was not significantly different between the two groups, both for the peak level (P = 0.354) and the preceding level (P = 0.555). In 16 (41%) out of 39 patients, systemic antiviral treatment was started without preceding antigenemia, as their CMV PCR tests showed positive results. The median time lag between initial CMV viremia to the diagnosis of CMV retinitis was 59 days and was not significantly different between the two groups (P = 0.120). ANC at the diagnosis of CMV retinitis was 1550, which was slightly higher in the HSCT group (P = 0.086).
Visual acuity tended to decrease at follow-up despite antiviral therapy (Table 2), which was especially notable in the SOT group (P = 0.028). In the HSCT and SOT groups, bilateral involvement was noted in 57.1% and 38.8% (P = 0.341), and foveal involvement was noted in 12.1% and 4.0% (P = 0.275). As for zonal involvement, central involvement was commonly observed in HSCT. The number of eyes that received intravitreal ganciclovir injection was not significantly different between the two groups (45.5% vs. 54.2%, P = 0.621). The number of intravitreal ganciclovir injections was significantly lower in the HSCT group (2.1 ± 2.9 vs. 10.4 ± 14.5, P = 0.002). Five patients in the HSCT group and one patient in the SOT group could not receive ganciclovir injection due to poor general condition. Six eyes (10.3%) underwent vitrectomy due to retinal detachment, most of which (5 eyes) were in the SOT group.
Logistic regression analyses were performed to determine the factors associated with poor visual prognosis (< 20/200) (Table 3). In univariate analyses, age (P = 0.027), concurrent systemic CMV disease (P = 0.020), mortality during follow-up (P = 0.015), zone 1 involvement (P = 0.049), and foveal involvement (P = 0.006) were identified as possible prognostic factors for poor visual outcomes. In multivariate analysis, the presence of concurrent CMV disease (OR = 14.11, P = 0.009) and foveal involvement (OR = 114.85, P = 0.001) were shown to be significantly associated with poor final visual outcomes.
Discussion
In this study, we performed a comprehensive analysis of CMV retinitis in transplant recipients. CMV retinitis developed in 11.3% of patients with CMV viremia at a median of four months after transplantation; specifically, CMV retinitis tended to develop more frequently in the HSCT group than in the SOT group. The HSCT group had more severe presentations and a significantly higher mortality rate than did the SOT group. During follow-up, patients with CMV retinitis tended to show visual loss despite antiviral treatments, which was more notable in the SOT group. The presence of concurrent CMV disease and foveal involvement were poor prognostic factors for CMV retinitis following transplantation. To the best of our knowledge, this is the first study to compare the clinical findings of CMV retinitis according to the type of organ transplantation.
The prevalence of CMV retinitis among patients with CMV viremia was higher in the HSCT group than in the SOT group with a marginal statistical significance. And the HSCT group had more patients in whom CMV retinitis occurred early during follow-up. These results are in line with those of a previous study that compared CMV diseases after kidney transplantation and HSCT [14]. The higher prevalence of CMV retinitis in the HSCT group may be explained by the higher viral load; even with a lower cut-off value of CMV antigenemia, the HSCT group had a higher viral load than did the SOT group as shown with antigenemia test and DNA PCR. In a previous study, patients undergoing HSCT achieved more intense immunosuppression than those undergoing SOT, which resulted in greater intensity and frequency of neutropenia [16]. In another study, the HSCT group was shown to be more susceptible to opportunistic infections than the SOT group in the process of re-establishing the immune system after transplantation [17]. Likewise, in our study population, only those in the HSCT group had concurrent CMV diseases. Considering the higher prevalence of CMV retinitis following HSCT despite the use of systemic ganciclovir in preemptive therapy, more frequent and close observations to detect retinal lesions for possible CMV retinitis are required for patients who undergo HSCT.
The HSCT group tended to have a more severe form of CMV retinitis, as a higher proportion of patients had bilateral or foveal involvement; as such, baseline visual acuity was poorer in the HSCT group. However, due to the poorer general condition and higher mortality rate, the HSCT group had a significantly shorter follow-up duration. As a result, the SOT group, whose a life expectancy was expected to be longer than in the HSCT group, showed significant deterioration of visual acuity and a higher incidence of retinal complications requiring vitrectomy during follow-up. In addition, the SOT group received more ocular treatments such as intravitreal ganciclovir injection, which is plausible because the HSCT group had less opportunity for receiving ophthalmic treatments. In our study population, ocular treatment was discontinued in a considerable portion of the HSCT patients whose macular were intruded with CMV lesions due to poor general condition.
Despite the seemingly poor outcomes noted in the HSCT group, we found that HSCT itself was not an independent risk factor associated with poor visual outcomes of CMV retinitis after transplantation. Rather, the presence of concurrent CMV disease and foveal involvement were found as significant risk factors. Despite receiving antiviral treatment, these patients still had poor visual prognosis. However, our results on the worsening of visual acuity despite treatment in CMV retinitis should not be interpreted as diminishing the importance of proper treatment in CMV retinitis. CMV retinitis is an opportunistic infection due to its intrinsic nature, and retinal lesions often improve as the general condition recovers. Therefore, we need to consider prompt and more aggressive systemic and local treatment including intraocular ganciclovir injection for such patients to prevent retinal complications and improve visual outcomes.[18]
The current study has several limitations including its retrospective design and the short follow-up period of the HSCT group. We recognize that it is hard to draw many robust conclusions from this study because of the considerable heterogeneity in age or disease state between the two groups. However, the clinical outcomes maintained the same trend when analyzing the results for adult patients. Moreover, possible confounders in the comparison of both groups were difficult to control because of the relatively small number of subjects. Nevertheless, as far as we are aware, no other studies have been conducted to compare the clinical features of CMV retinitis between SOT and HSCT. In this context, we believe that our data provide meaningful clinical outlooks in this grey area of limited experience.
In summary, the ophthalmic results and general prognosis in CMV retinitis were significantly different between SOT and HSCT. Whereas CMV retinitis in the HSCT group showed poorer initial presentation, the SOT group showed a prolonged deteriorating clinical course. Overall, concurrent CMV diseases and foveal involvement were significantly associated with poor final visual outcomes. Therefore, when examining patients with CMV retinitis after transplantation, these clinical features may be considered in order to choose the appropriate treatment strategy and predict the prognosis.
Data availability
Not applicable (pateints’ information is confidential).
References
Martin DF, Sierra-Madero J, Walmsley S, Wolitz RA, Macey K, Georgiou P, Robinson CA, Stempien MJ (2002) A controlled trial of valganciclovir as induction therapy for cytomegalovirus retinitis. N Engl J Med 346:1119–1126
Eid AJ, Bakri SJ, Kijpittayarit S, Razonable RR (2008) Clinical features and outcomes of cytomegalovirus retinitis after transplantation. Transpl Infect Dis 10:13–18. https://doi.org/10.1111/j.1399-3062.2007.00241.x
Jabs DA, Van Natta ML, Holbrook JT, Kempen JH, Meinert CL, Davis MD, Group SotOCoAR (2007) Longitudinal study of the ocular complications of AIDS: 1. Ocular diagnoses at enrollment. Ophthalmology 114:780–786.e783
Ausayakhun S, Watananikorn S, Ittipunkul N, Chaidaroon W, Patikulsila P, Patikulsila D (2003) Epidemiology of the ocular complications of HIV infection in Chiang Mai. J Med Assoc Thail 86:399–406
Ramanan P, Razonable RR (2013) Cytomegalovirus infections in solid organ transplantation: a review. Infect Chemother 45:260–271
Xhaard A, Robin M, Scieux C, de Latour RP, Deplus S, Mazeron M-C, Devergie A, Espérou H, Rocha V, Gluckman E (2007) Increased incidence of cytomegalovirus retinitis after allogeneic hematopoietic stem cell transplantation. Transplantation 83:80–83
Kuo IC, Kempen JH, Dunn JP, Vogelsang G, Jabs DA (2004) Clinical characteristics and outcomes of cytomegalovirus retinitis in persons without human immunodeficiency virus infection. Am J Ophthalmol 138:338–346
Kotton CN, Kumar D, Caliendo AM, Åsberg A, Chou S, Danziger-Isakov L, Humar A, Group TSICC (2013) Updated international consensus guidelines on the management of cytomegalovirus in solid-organ transplantation. Transplantation 96:333–360
Snydman D (1999) Infection in solid organ transplantation. Transpl Infect Dis 1:21–28
Coskuncan NM, Jabs DA, Dunn J, Haller JA, Green WR, Vogelsang GB, Santos GW (1994) The eye in bone marrow transplantation: VI. Retinal complications. Arch Ophthalmol 112:372–379
Ganly P, Arthur C, Goldman J, Schulenburg W (1988) Foscarnet as treatment for cytomegalovirus retinitis following bone marrow transplantation. Postgrad Med J 64:389–391
Boeckh M, Leisenring W, Riddell SR, Bowden RA, Huang ML, Myerson D, Stevens-Ayers T, Flowers ME, Cunningham T, Corey L (2003) Late cytomegalovirus disease and mortality in recipients of allogeneic hematopoietic stem cell transplants: importance of viral load and T-cell immunity. Blood 101:407–414. https://doi.org/10.1182/blood-2002-03-0993
Moon SM, Sung H, Kim MN, Lee SO, Choi SH, Kim YS, Woo JH, Kim SH (2012) Diagnostic yield of the cytomegalovirus (CMV) antigenemia assay and clinical features in solid organ transplant recipients and hematopoietic stem cell transplant recipients with CMV pneumonia. Transpl Infect Dis 14:192–197. https://doi.org/10.1111/j.1399-3062.2011.00703.x
Kim T, Lee Y-M, Lee S-O, Choi S-H, Kim YS, Woo JH, Sung H, Jung JH, Shin S, Kim YH (2016) Differences of cytomegalovirus diseases between kidney and hematopoietic stem cell transplant recipients during preemptive therapy. Korean J Intern Med 31:961
Kim DY, Jo J, Joe SG, Kim J-G, Yoon YH, Lee JY (2017) Comparison of visual prognosis and clinical features of cytomegalovirus retinitis in HIV and non-HIV patients. Retina 37:376–381
Burns L, Miller W, Kandaswamy C, DeFor T, MacMillan M, Van Burik J, Weisdorf D (2002) Randomized clinical trial of ganciclovir vs acyclovir for prevention of cytomegalovirus antigenemia after allogeneic transplantation. Bone Marrow Transplant 30:945
Schetelig J, Oswald O, Steuer N, Radonic A, Thulke S, Held T, Oertel J, Nitsche A, Siegert W (2003) Cytomegalovirus infections in allogeneic stem cell recipients after reduced-intensity or myeloablative conditioning assessed by quantitative PCR and pp65-antigenemia. Bone Marrow Transplant 32:695
Agarwal A, Kumari N, Trehan A, Khadwal A, Dogra MR, Gupta V, Sharma A, Gupta A, Singh R (2014) Outcome of cytomegalovirus retinitis in immunocompromised patients without Human Immunodeficiency Virus treated with intravitreal ganciclovir injection. Graefes Arch Clin Exp Ophthalmol 252:1393–1401
Funding
This study was supported by a grant from the Ministry of Science and ICT (Information and Communication Technology) (NRF-2019R1F1A1063124) and Asan Institute for Life Sciences (2011-0660), Asan Medical Center, Seoul, South Korea (NRF-2019R1F1A1063124).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the (place name of the institution and/or national research committee) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
The informed consent was waived under the approval of the Institutional Review Board of Asan Medical Center (2018-0815).
Consent for publication
Not applicable (retrospective review of anonymized medical records).
Code availabililty
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Son, G., Lee, J.Y., Kim, JG. et al. Clinical features of cytomegalovirus retinitis after solid organ transplantation versus hematopoietic stem cell transplantation. Graefes Arch Clin Exp Ophthalmol 259, 585–591 (2021). https://doi.org/10.1007/s00417-020-04871-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04871-w