Abstract
Purpose
The vitelliform stage is the typical phenotypic manifestation of Best vitelliform macular dystrophy (BVMD). As yet, no study has focused specifically on the clinical changes occurring in the vitelliform stage over the follow-up.
Methods
The survey takes the form of a prospective observational study with a 5-year follow-up. Twenty-one eyes of 11 patients in the vitelliform stage were examined annually. The primary outcome was the identification of the changes in the vitelliform lesion over a 5-year follow-up. Secondary outcomes included changes in structural optical coherence tomography (OCT) parameters and the correlation with the BCVA variation over the follow-up.
Results
Spectral domain OCT at baseline showed one subform characterized by solid vitelliform deposition, in 81% of eyes, and another subform characterized by a combination of solid deposition and subretinal fluid, in 19% of eyes. Overall, 62% of eyes showed an increase in the area of vitelliform deposition. Once the maximal area was reached, a progressive flattening of the vitelliform deposition took place, with subsequent flattening of the vitelliform lesion and formation of subretinal fluid. Hyperreflective foci (HF) increased in number as long as the vitelliform area continued to expand, with no variation in HF when the vitelliform lesion flattened or the subretinal fluid formed.
Conclusions
The vitelliform stage reveals more subforms with clinical variations over the follow-up. Our data suggest that the substage before the flattening of the lesion, thus before the so-called subretinal fluid accumulates and when the visual acuity is still high, might offer the best opportunity for an optimal therapeutic approach.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Best vitelliform macular dystrophy (BVMD) is an autosomal dominantly inherited disorder distinguished by a multifaceted phenotypic pattern. According to the most commonly used clinical classification, five main stages can be identified: subclinical, vitelliform, pseudohypopyon, vitelliruptive, and atrophic/cicatricial [1,2,3]. A simplified classification breaks the disease down into subclinical, vitelliform, and atrophic stages [4, 5]. The typical manifestation of the vitelliform stage takes the clinical form of a round/oval central yellow lesion prompted by the accumulation of lipofuscin. Visual acuity at this stage is generally good, whereas fundus autofluorescence most often reveals a patchy pattern [6, 7]. To date, no study has focused specifically on the vitelliform stage of BVMD with the aim of describing the clinical changes over the follow-up. The object of the present study is to investigate the natural evolution of eyes affected by the vitelliform stage in BVMD over a five-year follow-up.
Methods
The survey takes the form of a prospective observational study with a 5-year follow-up. A consecutive series of patients affected by BVMD were prospectively recruited from November 2009 to March 2013. Inclusion criteria were phenotypic aspect typical of the vitelliform stage of BVMD, along with genetic characterization with mutations of the BEST1 gene. Exclusion criteria were cataract or other media opacities and/or any condition that could confuse the functional response, including any other ocular or systemic disorder.
All patients underwent a complete annual ophthalmic examination, including best-corrected visual acuity (BCVA) on standard Early Treatment Diabetic Retinopathy Study charts, biomicroscopic examination with applanation tonometry, color photography (TRC-50DX; Topcon Corporation, Tokyo, Japan), blue-light fundus autofluorescence (FAF), and spectral-domain optical coherence tomography (SD-OCT) (Spectralis HRA + OCT; Heidelberg Engineering, Heidelberg, Germany). Both FAF images and SD-OCT scans were independently analyzed by two masked examiners unaware of the purpose of the study (FR and AA). Both examiners classified FAF according to 6 patterns (normal, hyper-autofluorescent, hypo-autofluorescent, patchy, multifocal, and spoke-like) [6]. The ellipsoid zone (EZ) and the external limiting membrane (ELM) were classed as either “preserved” (layer intact), “disrupted” (layer disorganization), or “absent” (layer loss), by means of a single horizontal scan centered on the fovea [5]. The same examiners measured the size of the vitelliform lesion both on color photography using the instrument’s image analysis software. The mean of the area measured by the two examiners was taken as the lesion size. Changes in size were sorted into the arbitrary categories of “increased” (> 0.1 mm2 increase from baseline to last follow-up examination), “stable” (variation of less than 0.1 mm2), and “decreased” (> 0.1 mm2 reduction with respect to the last follow-up examination).
In order to characterize the vitelliform lesion better, the SD-OCT acquisition protocol also included 19 horizontal linear B-scans (9 averaged OCT B-scans at 240-μm intervals, covering an area of 20 × 15°). Hyperreflective foci (HF) were identified as small hyperreflective focal areas within the retinal layers, invisible at the clinical examination and on fundus photography. The number of HF was determined considering the total number in all 19 horizontal linear B-scans acquired during the SD examination. HF were divided into the arbitrary categories of foveal HF (between 1 and 199 μm from the center) and junctional HF (in correspondence with the border between vitelliform deposition and healthy retina).
SD-OCT scan measurements were independently analyzed by two examiners (CDN and AB) unaware of the purpose of the study. The examiners counted the number of HF on a high-magnification section, measuring their greatest length manually and determining their location. The mean of the measurements of the same HF performed independently by the two masked readers was used in the analysis.
The primary outcome was the identification of the changes in the vitelliform lesion over a 5-year follow-up. Secondary outcomes included the changes in SD-OCT parameters and the correlation with the BCVA variation over the follow-up.
Results
Overall, eleven patients (21 eyes) were enrolled in the study. The mean age of the patients was 19 ± 12 years (range 6–50), with seven males and four females. Past and present general medical history was negative for all patients.
All 21 eyes showed a central, round/oval, yellowish lesion, typical of the vitelliform stage, on biomicroscopic examination. One patient revealed an asymmetric involvement: with one eye in the subclinical stage and the fellow eye in the vitelliform stage. BCVA changed from 0.18 ± 0.13 at baseline to 0.29 ± 0.16 LogMAR at the end of the 5-year follow-up.
Overall, considering any of the time-points during the follow-up, the vitelliform lesion increased in 14 eyes (66%), remained stable in 2 eyes (10%), and reduced in 5 eyes (24%). Eight eyes (38%) were found to be evolving toward the vitelliruptive stage at the end of the follow-up.
SD-OCT examination at baseline showed two different subforms of the vitelliform stage appearing biomicroscopically: a subform characterized by solid vitelliform deposition with OCT hyperreflective signal, in 17 eyes (81%), and another subform distinguished by a combination of solid deposition and subretinal fluid, in 4 eyes (19%). BCVA was similar in the 2 phenotypic subforms, both at baseline and at the end of the 5-year follow-up (Table 1).
Among the seventeen eyes characterized by a solid vitelliform lesion, the following evolution was observed at various time-points over the follow-up: 13 eyes (62% of all eyes) showed an increase and 4 eyes (19%) a decrease of the area of the lesion. On the other hand, out of the 4 eyes showing the combination of solid and fluid accumulation, no variations were noticed in 3 eyes (14% of all eyes) and a reduced area was observed in 1 eye (5%).
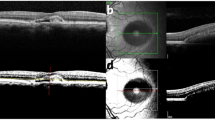
The 13 eyes that showed an enlargement of the lesion increased their area over a mean period of 2.3 ± 1.1 years, reaching a maximal area. Obviously, in all these eyes, no further enlargement occurred once the maximal area extension was reached, but a progressive flattening of the vitelliform deposition did take place. The flattening of the vitelliform lesion was subsequently followed by the formation of subretinal fluid, which was registered 3.15 ± 1.4 years from the beginning of the follow-up. Subretinal fluid tended to expand over the follow-up as the vitelliform material was gradually reabsorbed. A specimen case is shown in Fig. 1.
Natural course of vitelliform stage in BVMD over 5 years of follow-up. The typical vitelliform aspect is recognizable on fundus image at baseline (a), confirmed by structural OCT showing the presence of subretinal accumulation. This alteration increases in size both on fundus image and on structural OCT (b). At one point of the follow-up, the fundus examination continues to detect the vitelliform alteration, although structural OCT reveals a considerable decrease in subretinal accumulation (c). Finally, the fundus image and structural OCT in particular are able to show how the subretinal accumulation is replaced by clear fluid (d)
At baseline, the mean HF number in all 21 eyes was 5.4 ± 5.3 and 3.5 ± 3.9 in the foveal and junctional areas, respectively. The mean number of HF increased, echoing the area’s enlargement in the cohort of 13 eyes with baseline solid vitelliform deposition, whose area increased. In more detail, the number of HF in this latter cohort changed from 4.7 ± 4.2 and 2.2 ± 3.1 at baseline to 8.3 ± 4.4 and 6.9 ± 3.1 at the time-point of the maximal area increase in the foveal and junctional zones, respectively. The mean number of HF in the foveal and junctional zones turned out to be substantially stable when the vitelliform flattening occurred (8.7 ± 5.7 and 7.2 ± 4.3), as well as when the subretinal fluid formed (8.9 ± 4.5 and 7.5 ± 4.1), but revealed a tendency to increase when the subretinal fluid expanded (11.0 ± 7.5 and 8.7 ± 6.5).
Concerning the 4 eyes with mixed composition at baseline, the amount of subretinal fluid tended to enlarge over a mean of 1.25 ± 0.5 years, reaching a maximal extension. The mean number of HF in the foveal and junctional area was 6.1 ± 3.5 and 4.5 ± 4.7 at baseline, and 8.7 ± 7.6 and 5.1 ± 4.1 at the end of the 5-year follow-up.
Vitelliruptive evolution was documented in 8 eyes (38%) (6 of which originally in the subform characterized by solid vitelliform material, and another 2 eyes in the subform with mixed composition), over a mean of 2.75 ± 0.4 years. At the point of conversion to the vitelliruptive stage, BCVA changed from a baseline value of 0.2 ± 0.16 to 0.28 ± 0.21, whereas the mean number of HF in the foveal and junctional area changed from 6.3 ± 6.5 and 4.9 ± 4.7 to 12.8 ± 7.2 and 9.9 ± 5.6, respectively.
Baseline FAF showed hyper-autofluorescent and patchy patterns in 11 eyes (52%), and 10 eyes (48%), respectively. FAF showed a patchy pattern in all the eyes at the end of the follow-up. SD-OCT examination revealed a disrupted EZ and ELM in all the eyes at baseline, whereas at the end of the 5-year follow-up, both EZ and ELM turned out to be disrupted in 19 eyes (90%) and absent in 2 eyes (10%).
The thickness of the vitelliform lesion, measured on SD-OCT, significantly decreased in the eyes turning into vitelliruptive stage (P = 0.05), with figures of 270 ± 173 μm at baseline and 160 ± 63 μm at end of the follow-up. On the contrary, eyes still remaining in the same vitelliform stage did not show any appreciable difference in height (P = 0.634). Consequently, a reduction in height was found to be strongly associated with the vitelliruptive evolution (chi = 8.889; P = 0.003).
Overall, a progressive reduction of the vitelliform accumulation was evident in all eyes at the end of the 5-year follow-up.
Discussion
BVMD is an inherited autosomal dominant disease, in most cases related to mutations in the BEST1 gene, and is characterized by wide genetic and phenotypic heterogeneity. The complex metabolic alterations, primarily related to calcium-activated chloride channels, eventually result in a progressive accumulation of lipofuscin, clinically appearing as a yellow subretinal lesion, which represents the hallmark of the vitelliform stage of BVMD. In the literature, the vitelliform stage is described as normally evolving through a gradual reabsorption of the vitelliform material, with possible pseudohypopyon aspect, into the vitelliruptive stage [1,2,3]. However, there is no study explicitly focusing on the variations within the vitelliform stage over the follow-up.
Our study analyzes the 5-year evolution in eyes clinically displaying only the vitelliform stage on biomicroscopic examination. It indicates that in spite of the uniformly dense, yellowish aspect of the vitelliform stage, as visualized on biomicroscopic examination, structural OCT reveals two phenotypical subforms: one characterized by solid deposition in about 80% of eyes and another one with subretinal fluid in about 20% of eyes.
Furthermore, the more frequent subform, displaying solid vitelliform deposition, enlarges in about 75% of eyes in the vitelliform stage, whereas the mixed solid/subretinal fluid subform remains substantially stable. Once the vitelliform deposition has reached its maximal extension, the lesion gradually tends to flatten and in time further reabsorption of vitelliform material leads to the detection of what we usually define as “subretinal fluid”, possibly representing a mere empty space under the retina.
We hypothesize that the vitelliform subform with subretinal fluid represents an evolution of any previous solid subform. It is likely that a progressive enlargement may occur in all eyes in the vitelliform stage, but it can be recorded in only a fraction of them, since only a proportion of affected patients requires and undergoes regular examinations because of the good visual function.
Visual acuity remains substantially good in all eyes in the vitelliform stage, even though the formation of fluid marks a worsening. The outcomes of FAF, EZ, and ELM confirm the results of previous studies, showing the variable degree of involvement in the vitelliform stage [5,6,7].
HF are likely to represent a biomarker of the vitelliform deposition [8], their number increasing as the area enlarges. Nevertheless, there is no variation in the number of HF associated with the flattening of the vitelliform material and the accumulation of subretinal fluid. Moreover, HF increase slightly in number when the subretinal fluid expands. A similar HF trend was found comparing foveal and junctional areas.
Our observations may have a practical therapeutic implication. The vitelliform stage can be considered the most crucial stage of BVMD, as it is generally characterized by good visual acuity and more intact retinal layers. Thus, theoretically, the vitelliform stage is the most favorable moment for any therapeutic intervention in clinically evident BVMD designed to prolong the stage and preserve the visual function. Nevertheless, our investigation suggests that the substage before the flattening of the lesion, thus before the so-called subretinal fluid accumulates and when the visual acuity is still high, might offer the best opportunity for an optimal therapeutic approach.
We acknowledge that the present study has many limitations, especially bearing in mind the limited sample and the problems related to the HF calculations. BVMD is a rather infrequent disorder and it is therefore very difficult to recruit a sufficient number of patients in the vitelliform stage. In addition, the current technical limitations during SD-OCT examination militate against precise imaging, especially with regard to HF identification and quantification. In addition, the young age of some patients hampered high-quality OCT acquisition. It should also be said that our study’s scheduled yearly follow-up might have been too long to capture all the initial SD-OCT features. Lastly, the statistical analysis included both eyes of the same patient in all but one case (owing to asymmetric involvement), and this kind of approach could result in potential bias [9]. As mentioned above, BVMD is a rare disease and it is therefore hard to collect a sufficiently large sample. Consequently, we are aware that the present study ought to be regarded as merely an exploratory survey examining the natural course of the vitelliform stage in BVMD.
In essence, the present study reveals that eyes in the vitelliform stage of BVMD can present two SD-OCT phenotypic subforms, with a solid aspect in 80% of cases and a mixed form in 20% of eyes. The natural course of the solid subform leads to a flattening and the subsequent formation of subretinal fluid. Further studies are warranted to confirm our preliminary results and to extend our understanding of the natural course of BVMD.
References
Gass JDM (1997) Best’s disease. In: Gass J (ed) Stereoscopic atlas of macular diseases. Diagnosis and treatment. Vol 1, 4th edn. Mosby, St Louis, pp 304–311
Boon CJF, Klevering B, Leroy BP et al (2009) The spectrum of ocular phenotypes caused by mutations in the BEST1 gene. Progr Ret Eye Res 28:187–205
Booij JC, Boon CJF, van Schooneveld MJ et al (2010) Course of visual decline in relation to the Best1 genotype in vitelliform macular dystrophy. Ophthalmology 117:1415–1422
Battaglia Parodi M, Castellino N, Iacono P et al (2018) Microperimetry in Best vitelliform macular dystrophy. Retina 38:841–848
Battaglia Parodi M, Iacono P, Romano F, Bandello F (2018) Spectral domain optical coherence tomography features in different stages of Best vitelliform macular dystrophy. Retina 38:1041–1046
Battaglia Parodi MB, Iacono P, Campa C et al (2014) Fundus autofluorescence patterns in Best vitelliform macular dystrophy. Am J Ophthalmol 158:1086–1092
Battaglia Parodi M, Iacono P, Del Turco C et al (2015) Functional assessment of the fundus autofluorescence pattern in Best vitelliform macular dystrophy. Graefes Arch Clin Exp Ophthalmol 254:1297–1302
Battaglia Parodi M, Romano F, Sacconi R et al (2018) Intraretinal hyperreflective foci in Best vitelliform macular dystrophy. Retina 38:2379–2386
Murdoch IE, Morris SS, Cousens SN (1998) People and eyes: statistical approaches in ophthalmology. Br J Ophthalmol 82:971–973
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Francesco Bandello consultant for Allergan Inc. (Irvine, California, USA), Bayer Shering-Pharma (Berlin, Germany), Hoffmann-La-Roche (Basel, Switzerland), NTC Pharma, Novartis (Basel, Switzerland), SIFI, SOOFT, Thrombogenics (Heverlee, Belgium), and Zeiss (Dublin, USA). All other authors have no disclosures to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Battaglia Parodi, M., Romano, F., Arrigo, A. et al. Natural course of the vitelliform stage in best vitelliform macular dystrophy: a five-year follow-up study. Graefes Arch Clin Exp Ophthalmol 258, 297–301 (2020). https://doi.org/10.1007/s00417-019-04454-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04454-4