Abstract
Purpose
To investigate the effect of methotrexate (MTX) or sulfasalazine (SSZ) on the course of HLA-B27-positive, remitting acute anterior uveitis (AAU).
Methods
Forty-six patients with HLA-B27-positive AAU with or without associated systemic rheumatic disease either receiving MTX (n = 20), SSZ (n = 13), or no systemic immunomodulating treatment (Ctrl; n = 13) were studied retrospectively. Best-corrected visual acuity (BCVA), AAU relapse rate, and occurrence of uveitis-related ocular complications were analyzed at baseline (BL) and at 12-month follow-up (FU).
Results
Groups did not differ regarding age, gender, and presence of associated systemic diseases. BCVA at baseline was significantly worse in patients receiving MTX (logMAR 0.39 ± 0.4) than in those treated with SSZ (0.17 ± 0.2; P = 0.05) or in controls (Ctrl; 0.14 ± 0.2; P = 0.009). At the 12-month endpoint, MTX treatment was associated with significantly improved BCVA (0.18 ± 0.4 logMAR; P = 0.004). In contrast, BCVA did not significantly change in patients treated with SSZ (0.17 ± 0.3 logMAR) or in the controls (0.11 ± 0.2 logMAR). The annual uveitis relapse rate significantly decreased with MTX (BL 3.6 ± 2.4 relapses to FU 0.7 ± 0.8; P = 0.0001) and SSZ (BL 3.6 ± 1.9 to FU 1.8 ± 2.4, P < 0.01), but not in the controls (BL 1.9 ± 1.4 vs 1.9 ± 1.7 FU). The complication rate was slightly reduced with MTX (BL 1.75 ± 1.2 complications present versus FU 1.3 ± 1.2, P = 0.09) but not with SSZ (BL 0.9 ± 0.8 to FU 1.3 ± 1.4; P = 0.4) or in the controls (BL and FU 1.0 ± 0.95; P = 0.7).
Conclusions
MTX and SSZ reduced the uveitis relapse rate in HLA-B27-positive AAU patients, with MTX showing a beneficial effect on AAU-related macular edema.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Uveitis represents a group of conditions defined by infectious or noninfectious inflammation of the uvea [1, 2]. Depending on which part of the uvea is affected, it is classified into anterior, intermediate, posterior, or panuveitis [3]. Acute anterior uveitis (AAU), defined as acute onset of inflammation of the iris and/or ciliary body [3], is the most frequently occurring form of uveitis in the general population, accounting for 75–90% of cases in Western countries [2, 4]. Human leukocyte antigen (HLA)-B27-associated AAU is a distinct type of uveitis observed in a proportion of approximately 30% of all uveitis patients and approximately 50% of all cases of anterior uveitis in Western Europe and the USA. Its annual incidence is about 12/100,000 up to 23/100,000 in the population in Finland, where a high frequency of HLA–B27 in the population has been found [5].
HLA-B27 AAU may occur as a solitary condition, but is commonly associated with HLA-B27-associated spondyloarthropathy (SpA) [6,7,8,9]. The estimated frequency of SpA in patients with AAU is approximately 50%, whereas AAU has been reported in 25–40% of patients with SpA, therefore being the most frequent extra-articular manifestation of SpA [6,7,8,9,10].
HLA-B27-associated AAU has characteristic clinical features, including a young age of onset (peak 36 years), male preponderance, mostly unilateral or unilaterally alternating uveitis flares, a nongranulomatous appearance, and frequent recurrences [10, 11]. AAU typically manifests by redness, periorbital pain, photophobia, and blurred or decreased vision. It is often self-limiting, but a severe and remitting disease course may result in sight-threatening complications such as posterior synechiae formation, cataract, band keratopathy, secondary ocular hypertension or glaucoma, papillitis, and cystoid macular edema (CME).
Early and effective treatment is essential to prevent sight-threatening complications [12,13,14]. Aims of therapy are thus (1) to reduce inflammation, (2) to relieve pain during active inflammation, and (3) to prevent occurrence of complications and loss of vision with minimal adverse effects [15]. Standard therapy during AAU flares consists of topical corticosteroids (CS) and mydriatic eye drops [16, 17]. In more severe cases, periocular CS injections or systemic CS are used [18, 19].
The use of disease-modifying anti-rheumatic drugs (DMARD) such as methotrexate (MTX) or sulfasalazine (SSZ) as well as the more recently introduced anti-TNF agents are known to positively influence the course of disease. These agents are preferred in relapsing disease or prolonged inflammation despite CS therapy, when sight-threatening complications such as macular edema develop, in the presence of HLA-B27-associated systemic diseases, for steroid-sparing, especially in case of ocular side effects (e.g., steroid-induced glaucoma), or when generalized CS-related adverse events develop that require tapering or discontinuation of those drugs [3, 15].
While extensively studied and well established for the treatment of many other uveitis entities, the effect of nonbiological DMARDs on the AAU course is still not well defined. For both SSZ and MTX, a reduction in the AAU flare rate has been reported [20,21,22], while studies directly comparing the efficacy of both medications are missing. In this retrospective case-control study, we therefore compared the effect of MTX and SSZ on the AAU course in HLA-B27-positive patients.
Patients and methods
A retrospective cohort study was performed, including a total of 46 patients of Caucasian origin with HLA-B27-positive AAU. Patients who were treated between 2003 and 2016 were selected from the uveitis database at our tertiary referral center. Patients were included if they had been diagnosed with recurrent HLA-B27-positive anterior uveitis with acute onset of flares [23] and if they were exclusively treated with MTX (20 patients) or SSZ (13 patients), initiated because of uveitis, and if treatment was continued for at least 12 months. Patients started on SSZ or MTX, but later discontinuing the respective medication during the first year of treatment were excluded from the study. Patients received MTX once per week orally or subcutaneously (10–20 mg/week and occasionally up to 25 mg/week with dosage depending on body surface area), and with oral substitution of 5 mg folic acid 24 h later. SSZ was administered orally every day (doses 250–1000 mg/day). Additionally, 13 patients with HLA-B27-positive AAU and similar epidemiological and clinical characteristics but who had not received systemic anti-inflammatory treatment (AIT) served as control group (Ctrl). All patients including the controls received topical CS (prednisolone acetate 1%) and mydriatic eye drops during acute uveitis recurrence.
Epidemiological and ophthalmological parameters were assessed at baseline before instituting treatment with MTX or SSZ (baseline, BL) and also 1 year later (13.2 ± 4.9 months; follow-up, FU), including age, gender, presence, and type of HLA-B27-associated diseases, uni- or bilaterality of uveitis, number of all relapses during the previous 12 months, presence of ocular complications, and any ocular and systemic anti-inflammatory treatment. Follow-up ophthalmologic evaluations included best-corrected visual acuity (BCVA), intraocular pressure (IOP, applanation tonometry), and slit-lamp and fundus examinations. The presence of cystoid macular edema (CME) in fundoscopy (90 dpt. lens) was judged by typical macular abnormalities and was proven by optical coherence tomography (OCT), fluorescein angiography (images, 3 min), or both.
The treatment effect on the AAU course was judged by best-corrected visual acuity (BCVA, logMAR), uveitis relapse rate as defined by the number of AAU flares/patient/12 months, and the presence of sight-threatening complications, including band keratopathy, posterior synechiae, secondary cataract formation, glaucoma and ocular hypertension (≥ 22 mmHg, no glaucoma typical disk or visual field abnormalities), papillitis, and macular edema.
The study design conforms to the standards currently applied in Germany. No institutional review board approval or informed consent is required for chart review studies based on fully anonymized data as provided to the study directly by the treating physician.
For statistical analysis, GraphPad Prism version 7.0 (GraphPad Software, La Jolla California USA) was used. Chi-squared test, Fisher’s exact t test, Mann–Whitney test, one-way ANOVA (Kruskal-Wallis) test, and Wilcoxon rank test were used where appropriate. A probability (P) value equaling or lower than 5% (≤ 0.05) was regarded as significant.
Results
Clinical characteristics
The three patient groups did not differ significantly with regard to clinical and epidemiological characteristics (Table 1). At baseline (BL), there were no significant differences regarding age, gender, and affected eyes. Twenty patients (43.5%) presented with additional HLA-B27-associated conditions, such as ankylosing spondylitis (35%, n = 16), sacroiliitis (n = 1), ulcerative colitis (n = 1), or other SpA (n = 2). However, there was no significant difference between the groups regarding presence of HLA-B27-associated systemic diseases (P = 0.55). Twenty-six patients (56.5%) had HLA-B27-positive AAU without associated systemic disease (Table 1). At follow-up, 6 eyes (19%) of the MTX group, 4 eyes (24%) of the SSZ group, and 9 eyes (43%) of the control group received topical steroids.
MTX or SSZ treatment positively influenced the course of visual acuity in patients with HLA-B27-positive AAU
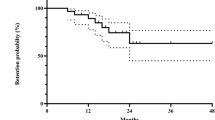
Best-corrected visual acuity (BCVA) in AAU-affected eyes differed among the cohorts before initiating MTX or SSZ treatment (Fig. 1). At baseline, vision was significantly worse in those patients then receiving MTX (0.39 ± 0.4 logMAR) than in those given SSZ (0.17 ± 0.2 logMAR, *P = 0.05) or in control patients (Ctrl 0.14 ± 0.2 logMAR, **P = 0.009).
Visual acuity in patients with acute anterior uveitis (AAU) treated with methotrexate (MTX) or sulfasalazine (SSZ). Best-corrected visual acuity (BCVA; logMAR) in AAU-affected eyes differed among the cohorts before systemic anti-inflammatory treatment with MTX or SSZ was initiated (baseline, BL). At baseline, BCVA was significantly worse in patients then receiving MTX than in those given SSZ (P = 0.05) or in control patients (P = 0.009). At the 12-month follow-up (FU), treatment with MTX (P = 0.004), but not with SSZ (P = 0.9), was associated with a significant improvement in BCVA. All data were assessed using Mann-Whitney U test; they are presented as mean ± standard deviation. A p value ≤ 0.05 was regarded as significant. Abbreviations: MTX AAU patients treated with MTX; SSZ AAU patients treated with SSZ; Ctrl AAU patients not receiving systemic immunomodulating therapy
At 12-month follow-up, MTX treatment was associated with a significant improvement in BCVA from logMAR 0.39 ± 0.4 to 0.18 ± 0.4 (P = 0.004), while this was not observed under SSZ (P = 0.9) or in the control group (P = 0.5). Nevertheless, there was no significant difference in BCVA between the three groups at the 12-month time point (P = 0.4).
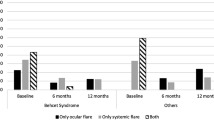
MTX or SSZ treatment reduced HLA-B27-positive AAU relapse rates
We then assessed AAU disease courses under the diverse treatment regimens. At baseline, the number of uveitis flares during the previous 12 months was significantly higher in those patients later receiving systemic anti-inflammatory treatment for their AAU than in control patients (Fig. 2). Before initiating systemic treatment, number of flares per 12 months was identical for patients of the MTX group and those of the SSZ group (3.6 ± 1.9). In contrast, control patients had significantly lower relapse rates (1.9 ± 1.4 flares per 12 months) at BL than did the MTX (P = 0.005) or SSZ group (P = 0.01).
Uveitis relapse rate in patients with acute anterior uveitis (AAU) treated with methotrexate (MTX) or sulfasalazine (SSZ). The annual uveitis relapse rate was calculated as number of uveitis flares per patient in 12 months. The uveitis flare rate decreased in both patients receiving either MTX (P = 0.0001) or SSZ (P < 0.01) compared to baseline (BL) and was significantly lower at the 12-month follow-up (FU) in MTX-treated than in control patients who had not received systemic anti-inflammatory medication (*P = 0.01). All data were assessed using Mann-Whitney U test; they are presented as mean ± standard deviation. A p value ≤ 0.05 was regarded as significant. Abbreviations: MTX AAU patients treated with MTX; SSZ AAU patients treated with SSZ; Ctrl AAU patients not receiving systemic immunomodulating therapy
At 12-month follow-up, the AAU relapse rates were significantly reduced in patients receiving either systemic MTX or SSZ medication. At follow-up, patients treated with MTX had developed 0.7 ± 0.8 AAU flares within the 12 months (P = 0.0001 compared to pre-treatment values). The relapse rate was significantly lower than in control patients not receiving systemic anti-inflammatory medication, who presented with a relapse rate of 1.9 ± 1.7 during follow-up (P = 0.01). Patients treated with SSZ also showed a significant reduction in AAU relapse rate from 3.6 ± 1.9 at BL to 1.8 ± 2.4 flares in 12 months at FU (P = 0.01). No AAU relapse occurred during the follow-up period in 45% of patients treated with MTX (P = < 0.0001 vs Ctrl), in 38% of patients treated with SSZ (P = 0.0004 vs Ctrl; P = 0.4 MTX vs SSZ), and in only 15% of the control patients.
MTX or SSZ treatment reduced sight-threatening, HLA-B27-positive, AAU-associated complications
HLA-B27-positive AAU may potentially cause sight-threatening complications. Preventing such complications is a major goal of treatment. Before initiation of treatment, patients from the MTX-group had developed 1.75 ± 1.2 uveitis-associated complications per affected eye. At follow-up, this complication rate per AAU-affected eye had slightly decreased to 1.3 ± 1.2 in MTX-treated patients (P = 0.09). In contrast, patients taking SSZ had developed 1.3 ± 1.4 ocular complications per AAU-affected eye at FU, as compared to a complication rate of 0.9 ± 0.9 before treatment (P = 0.4). In control patients, the complication rate remained unchanged from 0.95 ± 0.95 at BL compared to 1.0 ± 0.95 at FU (P = 0.7) (Table 2). When analyzing the frequency of individual complications, the only complication for which a significant difference was observed was the frequency of CME in MTX-treated patients (n = 13 eyes at baseline vs n = 0 eyes at follow-up; p < 0.0001). All other complications did not display relevant differences between pre- and post-treatment timepoints.
None of the patients developed band-keratopathy before treatment or during the subsequent follow-up period. Secondary glaucoma was only found in two patients treated with MTX and in another two control patients at baseline as well as during the 12-month follow-up. Incident glaucoma was not observed during the observation period. Ocular hypertension was found in seven patients before and in six patients after 1 year of MTX treatment. Ocular hypertension was found in two patients before and during treatment with SSZ. Only one patient in the control group presented with incident ocular hypertension after follow-up, increasing their numbers from two patients at baseline to three patients at 12-month follow-up.
The most frequent complication of AAU detected in all patients with HLA-B27-positive AAU was cystoid macular edema (CME). At baseline, 15 AAU-affected eyes presented with clinically significant CME, 13 in patients who then started on MTX and in 1 each of both the SSZ and control group. Notably, CME resolved in all patients during the MTX treatment period, and in none of the MTX-treated patients did CME develop anew under treatment. In contrast, two patients treated with SSZ newly developed CME during follow-up, and another one had persistent CME despite SSZ therapy (Table 2). The only eye with CME at baseline among the control patients did not show any more significant macular pathology at FU.
A relevant proportion of patients treated with MTX or SSZ experiences side effects
In the patient population discussed in this study, side effects of treatment were not frequent. A total of four patients in the MTX group and one patient in the SSZ group experienced side effects of treatment (MTX: two patients with nausea, two patients with transient elevation of liver enzymes; SSZ: gastrointestinal side effects and malaise).
However, we identified an additional 16 patients seen in our clinic during the same period of time and meeting all inclusion criteria besides time of treatment (7 started on MTX and 9 on SSZ), who were not able to complete the full 12 months of treatment (and were, therefore, not included in the current analysis). This was due to side effects (concerning four patients in the MTX group and five patients in the SSZ group) or lack of effectiveness of treatment (three in the MTX group and four in the SSZ group).
We can therefore conclude that treatment needed to be terminated during the first year of therapy in 26% of MTX-treated (7 out of 27) and 41% of SSZ-treated (9 out of 22) patients due to side effects or ineffectiveness of treatment and therapy can therefore be considered primarily unsuitable/unsuccessful in those patients.
Discussion
Early and effective treatment of HLA-B27-positive AAU—beyond CS—is crucial to prevent severe sight-threatening complications. Relapse rates are high, and ocular complications and subsequent visual impairment may develop more frequently than in HLA-B27-negative anterior uveitis patients [24]. Our study suggests that MTX or SSZ positively influences the course of HLA-B27-positive AAU by reducing the relapse rate and sight-threatening complications. Furthermore, MTX seems to be a potent drug promoting visual recovery in patients with CME.
First-line treatment of AAU primarily consists of corticosteroids. The efficacy of topical CS is high [17], whereas topically applied NSAID are not as effective [25]. To reach a higher level of drug efficacy, subconjunctival or peribulbar injections can be performed [26]. Long-term intake of systemic CS may not be of benefit and may cause undesired side effects.
Systemic DMARDs, including MTX, sulfasalazine, or cyclosporin A, are indicated mostly in cases of persisting active ocular inflammation, recurrent flares despite CS therapy, or sight-threatening complications—especially macular edema. In case of systemic HLA-B27-associated diseases, systemic DMARD treatment may be indicated to improve general health and quality of life, as well as for steroid-sparing [3, 15].
Sulfasalazine (Azulfidine, SSZ) is a classical DMARD that has been extensively studied and is often used for first-line medical treatment of rheumatoid arthritis (RA) and inflammatory bowel disease since its use was approved in the USA in 1950. SSZ has previously been suggested as potential treatment for AAU [21] and a reduction in flare rate and severity of AAU by this treatment has been described [20, 21]. Sieper et al. suggested a similar efficacy for SSZ and the TNF inhibitor etanercept in preventing uveitis relapses [27]. However, the therapeutic capacity as compared to other treatment modes routinely chosen in clinical practice, particularly MTX, has not yet been defined [28].
SSZ is broken down into sulfapyridine and 5-aminosalicylic acid; in case of allergies to aspirin or sulfonamides, it is therefore obsolete. It is taken orally at initial dosages of 1 g/day and then increased by 500 mg/day up to a final intake of 2 g/day. Typical adverse effects of SSZ include loss of appetite, nausea, headache, fatigue, and rash, and significant side effects develop in as many as 11–40% of treated patients [29]. Severe and usually irreversible side effects such as bone marrow suppression or liver and kidney damage are rare when the treatment is properly and frequently monitored.
The folic acid antagonist MTX is another well-studied DMARD, to date with more trials and long-term clinical experience than any other immunomodulating therapeutic agent. Owing to its effectiveness and safety, low-dose MTX, administered weekly at doses of 7.5–25 mg/week, has commonly been being used as first-line therapy in the treatment of RA and other autoimmune conditions since the 1980s [30,31,32,33]. Although MTX has been widely used in the treatment of uveitis for decades, there are only few data describing experience with MTX in a uveitis entity as common as AAU. Samson and colleagues (24) reported a visual improvement in 90% of 160 patients with chronic noninfectious uveitis as well as decreased inflammatory activity in 76%, and a steroid-sparing effect in 56% of the patients treated with MTX, while adverse effects could be detected in only 18%, and severe adverse effects were observed in 8% of the patients [34]. A retrospective multi-center study confirmed these observations [35]. Rathinam et al. found that uveitis inactivity was achieved in 69% of patients with non-infectious intermediate, posterior, or panuveitis receiving MTX for 6 months, but only in 47% of patients treated with mycophenolate mofetil [36]. Another RCT found that MTX was inferior to IFN beta regarding resolution of CME in patients with intermediate uveitis [37]. However, no comprehensive data exist on the efficacy of MTX treatment in HLA-B27-associated AAU.
Compared to other immunosuppressant drugs, low-dose MTX is relatively safe and well tolerated, when given under strict monitoring. One advantage of MTX over many other conventional DMARDs is its weekly administration. However, discontinuation rates are as high as 16% due to adverse effects, which may occur even at low dosages [35, 38]. Typical adverse effects of MTX include nausea, headaches, and fatigue, especially on the day of administration. In addition, hepatotoxicity and liver function abnormalities, gastrointestinal toxicity, and bone marrow suppression are typical adverse effects of MTX, but they can be diminished by subsequent folic acid supplementation [39, 40]. Multiple studies have confirmed the superior and beneficial effects of the “anchor drug” MTX (alone or in combination with other drugs) in comparison to other DMARDs on rheumatoid arthritis [30, 38, 41,42,43]. Regarding the systemic HLA-B27-associated conditions, MTX has been traditionally used to treat psoriatic SpA and ankylosing SpA and SSZ primarily for inflammatory bowel disease, but an inhibitory effect on the course of these conditions and especially on the progression of arthritis could not be demonstrated either for MTX or for SSZ [44,45,46,47].
The aim of our study was to add evidence for two medication strategies routinely employed in clinical practice as an attempt to facilitate therapeutic decisions in managing patients with HLA-B27-associated AAU. The decision to initiate systemic treatment with either SSZ or MTX in this clinical entity is currently based upon a variety of factors, including the clinician’s experience with one or the other medication, the rheumatologist’s recommendation, and, of course, patients’ preferences, but reliable data comparing the efficiency of the two drugs in this clinical setting or even indicating a promising role for MTX treatment in this entity are lacking.
Our study is in line with previously published data on the effect of SSZ in AAU regarding reduction of severity and number of flares (20, 21, 27). We can now demonstrate a similar efficacy of MTX in reducing flare rate and, moreover, observe a beneficial effect in patients presenting with CME, a severe vision-threatening complication of AAU. Our results are in line with a recent prospective study by Bachta and colleagues, who showed that MTX dosed at 25 mg/week is highly effective in the treatment of recurrent idiopathic AAU, regardless of HLA-B27 positivity (15). The authors report long-term results of MTX therapy in 19 patients with recurrent idiopathic AAU, the mean follow-up period being 3.3 years. Of all patients, 84% remained flare-free on MTX therapy, and the number of AAU flares in the whole cohort decreased from 2.12 to 0.11/patient-year. Interestingly, all flares observed on MTX therapy observed by the Bachta group occurred in HLA-B27-positive patients. Our study, however, exclusively included HLA-B27-positive patients with AAU, and we also report beneficial effects of MTX on relapse rates.
To our knowledge, no data exist on the effect of MTX on CME in HLA-B27-associated AAU. Mackensen et al. reported worsening of CME in MTX-treated patients as compared to a beneficial effect of IFN beta; however, these patients had been diagnosed with intermediate uveitis, a clinically and probably pathomechanistically different entity [37]. Another retrospective study comparing the effect of TNF blockade and conventional DMARDs (including patients receiving MTX) on CME in uveitis of different entities found that both treatments achieved a similar reduction in foveal thickness [48]; however, as the cohort was not stratified according to subgroups of conventional DMARDs, the effect of MTX monotherapy can hardly be deduced from these data.
Our study suggests that MTX and SSZ positively influence the course of HLA-B27-positive AAU, by reducing the relapse rate and sight-threatening complications. Our findings also suggest that MTX is a potent drug when it comes to promoting visual recovery, as CME resolved in all patients treated with MTX, and none of the MTX-group newly developed CME under treatment. As most of our patients presenting with CME and, therefore, with reduced BCVA, were started on MTX treatment, a meaningful statistical comparison of SSZ versus MTX regarding the potency in resolving CME is not possible. Our data suggest that, depending on the clinical situation as defined by disease activity, presence, and severity of uveitis complications, initiation of MTX treatment might represent a valuable alternative to the already well-documented use of SSZ.
This study has some limitations, not only due to its retrospective design, but also as only patients were included who were treated with MTX or SSZ for at least 12 months because of their HLA-B27-positive AAU. Patients in whom the respective DMARD had been withdrawn early due to insufficient immunosuppression or due to incompliance, and in whom adverse effects had developed, were not taken into account, although retrospective analysis of our patient population suggests that this might be a rather frequent problem, especially in those patients receiving SSZ.
When regarding clinical characteristics at baseline, patients later receiving MTX probably were those with a worse course of disease, as in this group, relapses and occurrence of CME were more frequent, and BCVA was worse, accordingly. It might, therefore, be that any effect of the different systemic medications observed could have been even more pronounced, had patients been randomly assigned to one of the treatment regimes. Selection of patients with a worse course of disease for MTX treatment might lead to underestimation of the beneficial effect of this medication.
In conclusion, systemic anti-inflammatory therapy with MTX as well as with SSZ positively influences relapse rates in patients with HLA-B27-positive AAU with MTX demonstrating a beneficial effect on AAU-related macular edema.
References
Darrell RW, Wagener HP, Kurland LT (1962) Epidemiology of uveitis. Incidence and prevalence in a small urban community. Arch Ophthalmol 68:502–514
Chang JH, Wakefield D (2002) Uveitis: a global perspective. Ocul Immunol Inflamm 10:263–279
Jabs DA, Rosenbaum JT, Foster CS, Holland GN, Jaffe GJ, Louie JS, Nussenblatt RB, Stiehm ER, Tessler H, Van Gelder RN, Whitcup SM, Yocum D (2000) Guidelines for the use of immunosuppressive drugs in patients with ocular inflammatory disorders: recommendations of an expert panel. Am J Ophthalmol 130:492–513
Brewerton DA, Caffrey M, Nicholls A, Walters D, James DC (1973) Acute anterior uveitis and HL-A 27. Lancet 302:994–996
Chang JH, McCluskey PJ, Wakefield D (2005) Acute anterior uveitis and HLA-B27. Surv Ophthalmol 50:364–388
Brewerton DA, Caffrey M, Nicholls A, Walters D, Oates JK, James DC (1973) Reiter's disease and HL-A 27. Lancet 302:996–998
Brewerton DA, Hart FD, Nicholls A, Caffrey M, James DC, Sturrock RD (1973) Ankylosing spondylitis and HL-A 27. Lancet 1:904–907
Linder R, Hoffmann A, Brunner R (2004) Prevalence of the spondyloarthritides in patients with uveitis. J Rheumatol 31:2226–2229
Monnet D, Breban M, Hudry C, Dougados M, Brezin AP (2004) Ophthalmic findings and frequency of extraocular manifestations in patients with HLA-B27 uveitis: a study of 175 cases. Ophthalmology 111:802–809
Zeboulon N, Dougados M, Gossec L (2008) Prevalence and characteristics of uveitis in the spondyloarthropathies: a systematic literature review. Ann Rheum Dis 67:955–959
Braakenburg AM, de Valk HW, de Boer J, Rothova A (2008) Human leukocyte antigen-B27-associated uveitis: long-term follow-up and gender differences. Am J Ophthalmol 145:472–479
Selmi C (2014) Diagnosis and classification of autoimmune uveitis. Autoimmun Rev 13:591–594
Larson T, Nussenblatt RB, Sen HN (2011) Emerging drugs for uveitis. Expert Opin Emerg Drugs 16:309–322
D’Ambrosio EM, Cava M, Tortorella P, Gharbyia M, Campanella M, Iannetti L (2016) Clinical features and complications of the HLA-B27-associated acute anterior uveitis: a Metanalysis. Semin Ophthalmol 32(6):689–701
Islam N, Pavesio C (2010) Uveitis (acute anterior). BMJ Clin Evid 2010:0705
Dunn JP (2004) Review of immunosuppressive drug therapy in uveitis. Curr Opin Ophthalmol 15:293–298
Dunne JA, Jacobs N, Morrison A, Gilbert DJ (1985) Efficacy in anterior uveitis of two known steroids and topical tolmetin. Br J Ophthalmol 69:120–125
Gaudio PA (2004) A review of evidence guiding the use of corticosteroids in the treatment of intraocular inflammation. Ocul Immunol Inflamm 12:169–192
Wakefield D (1985) Methylprednisolone pulse therapy in severe anterior uveitis. Aust N Z J Ophthalmol 13:411–415
Benitez-Del-Castillo JM, Garcia-Sanchez J, Iradier T, Banares A (2000) Sulfasalazine in the prevention of anterior uveitis associated with ankylosing spondylitis. Eye (Lond) 14(Pt 3A):340–343
Munoz-Fernandez S, Hidalgo V, Fernandez-Melon J, Schlincker A, Bonilla G, Ruiz-Sancho D, Fonseca A, Gijon-Banos J, Martin-Mola E (2003) Sulfasalazine reduces the number of flares of acute anterior uveitis over a one-year period. J Rheumatol 30:1277–1279
Munoz-Fernandez S, Garcia-Aparicio AM, Hidalgo MV, Platero M, Schlincker A, Bascones ML, Pombo M, Morente P, Sanpedro J, Martin-Mola E (2009) Methotrexate: an option for preventing the recurrence of acute anterior uveitis. Eye (Lond) 23:1130–1133
Jabs DA, Nussenblatt RB, Rosenbaum JT (2005) Standardization of uveitis nomenclature for reporting clinical data. Results of the first international workshop. Am J Ophthalmol 140:509–516
Power WJ, Rodriguez A, Pedroza-Seres M, Foster CS (1998) Outcomes in anterior uveitis associated with the HLA-B27 haplotype. Ophthalmology 105:1646–1651
Sand BB, Krogh E (1991) Topical indometacin, a prostaglandin inhibitor, in acute anterior uveitis. A controlled clinical trial of non-steroid versus steroid anti-inflammatory treatment. Acta Ophthalmol 69:145–148
Weijtens O, Feron EJ, Schoemaker RC, Cohen AF, Lentjes EG, Romijn FP, van Meurs JC (1999) High concentration of dexamethasone in aqueous and vitreous after subconjunctival injection. Am J Ophthalmol 128:192–197
Sieper J, Koenig A, Baumgartner S, Wishneski C, Foehl J, Vlahos B, Freundlich B (2010) Analysis of uveitis rates across all etanercept ankylosing spondylitis clinical trials. Ann Rheum Dis 69:226–229
Wakefield D, Chang JH, Amjadi S, Maconochie Z, Abu El-Asrar A, McCluskey P (2011) What is new HLA-B27 acute anterior uveitis? Ocul Immunol Inflamm 19:139–144
Rogler G (2010) Gastrointestinal and liver adverse effects of drugs used for treating IBD. Best Pract Res Clin Gastroenterol 24:157–165
Cronstein BN (2005) Low-dose methotrexate: a mainstay in the treatment of rheumatoid arthritis. Pharmacol Rev 57:163–172
Gubner R, August S, Ginsberg V (1951) Therapeutic suppression of tissue reactivity. II Effect of aminopterin in rheumatoid arthritis and psoriasis. Am J Med Sci 221:176–182
Guidelines ACoRSoRA (2002) Guidelines for the management of rheumatoid arthritis: 2002 update. Arthritis Rheum 46:328–346
Rantalaiho V, Korpela M, Hannonen P, Kautiainen H, Jarvenpaa S, Leirisalo-Repo M, Hakala M, Puolakka K, Julkunen H, Luosujarvi R, Mottonen T (2009) The good initial response to therapy with a combination of traditional disease-modifying antirheumatic drugs is sustained over time: the eleven-year results of the Finnish rheumatoid arthritis combination therapy trial. Arthritis Rheum 60:1222–1231
Samson CM, Waheed N, Baltatzis S, Foster CS (2001) Methotrexate therapy for chronic noninfectious uveitis: analysis of a case series of 160 patients. Ophthalmology 108:1134–1139
Gangaputra S, Newcomb CW, Liesegang TL, Kacmaz RO, Jabs DA, Levy-Clarke GA, Nussenblatt RB, Rosenbaum JT, Suhler EB, Thorne JE, Foster CS, Kempen JH (2009) Methotrexate for ocular inflammatory diseases. Ophthalmology 116:2188–2198 e2181
Rathinam SR, Babu M, Thundikandy R, Kanakath A, Nardone N, Esterberg E, Lee SM, Enanoria WT, Porco TC, Browne EN, Weinrib R, Acharya NR (2015) A randomized clinical trial comparing methotrexate and mycophenolate mofetil for noninfectious uveitis. Ophthalmology 121:1863–1870
Mackensen F, Jakob E, Springer C, Dobner BC, Wiehler U, Weimer P, Rohrschneider K, Fiehn C, Max R, Storch-Hagenlocher B, Becker MD (2013) Interferon versus methotrexate in intermediate uveitis with macular edema: results of a randomized controlled clinical trial. Am J Ophthalmol 156:478–486 e471. https://doi.org/10.1016/j.ajo.2013.05.002
Lopez-Olivo MA, Siddhanamatha HR, Shea B, Tugwell P, Wells GA, Suarez-Almazor ME (2014) Methotrexate for treating rheumatoid arthritis. Cochrane Database Syst Rev (6):CD000957. https://doi.org/10.1002/14651858.CD000957.pub2
van Ede AE, Laan RF, Rood MJ, Huizinga TW, van de Laar MA, van Denderen CJ, Westgeest TA, Romme TC, de Rooij DJ, Jacobs MJ, de Boo TM, van der Wilt GJ, Severens JL, Hartman M, Krabbe PF, Dijkmans BA, Breedveld FC, van de Putte LB (2001) Effect of folic or folinic acid supplementation on the toxicity and efficacy of methotrexate in rheumatoid arthritis: a forty-eight week, multicenter, randomized, double-blind, placebo-controlled study. Arthritis Rheum 44:1515–1524
Salliot C, van der Heijde D (2009) Long-term safety of methotrexate monotherapy in patients with rheumatoid arthritis: a systematic literature research. Ann Rheum Dis 68:1100–1104
Hazlewood GS, Barnabe C, Tomlinson G, Marshall D, Devoe DJ, Bombardier C (2016) Methotrexate monotherapy and methotrexate combination therapy with traditional and biologic disease modifying antirheumatic drugs for rheumatoid arthritis: a network meta-analysis. Cochrane Database Syst Rev (8):CD010227. https://doi.org/10.1002/14651858.CD010227.pub2
Gaujoux-Viala C, Smolen JS, Landewe R, Dougados M, Kvien TK, Mola EM, Scholte-Voshaar M, van Riel P, Gossec L (2010) Current evidence for the management of rheumatoid arthritis with synthetic disease-modifying antirheumatic drugs: a systematic literature review informing the EULAR recommendations for the management of rheumatoid arthritis. Ann Rheum Dis 69:1004–1009
Nam JL, Ramiro S, Gaujoux-Viala C, Takase K, Leon-Garcia M, Emery P, Gossec L, Landewe R, Smolen JS, Buch MH (2010) Efficacy of biological disease-modifying antirheumatic drugs: a systematic literature review informing the 2013 update of the EULAR recommendations for the management of rheumatoid arthritis. Ann Rheum Dis 73:516–528
Raychaudhuri SP, Wilken R, Sukhov AC, Raychaudhuri SK, Maverakis E (2017) Management of psoriatic arthritis: early diagnosis, monitoring of disease severity and cutting edge therapies. J Autoimmun 76:21–37
Lim WC, Wang Y, MacDonald JK, Hanauer S (2016) Aminosalicylates for induction of remission or response in Crohn's disease. Cochrane Database Syst Rev 7:CD008870
Chen J, Liu C (2005) Sulfasalazine for ankylosing spondylitis. Cochrane Database Syst Rev (2):CD004800. https://doi.org/10.1002/14651858.CD004800.pub2
Chen J, Liu C, Lin J (2006) Methotrexate for ankylosing spondylitis. Cochrane Database Syst Rev (4):CD004524. https://doi.org/10.1002/14651858.CD004524.pub3
Schaap-Fogler M, Amer R, Friling R, Priel E, Kramer M (2013) Anti-TNF-alpha agents for refractory cystoid macular edema associated with noninfectious uveitis. Graefes Arch Clin Exp Ophthalmol = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie 252:633–640
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study design conforms to the standards currently applied in Germany. No institutional review board approval or informed consent is required for chart review studies based on fully anonymized data as provided to the study directly by the treating physician.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
zu Hoerste, M.M., Walscheid, K., Tappeiner, C. et al. The effect of methotrexate and sulfasalazine on the course of HLA-B27-positive anterior uveitis: results from a retrospective cohort study. Graefes Arch Clin Exp Ophthalmol 256, 1985–1992 (2018). https://doi.org/10.1007/s00417-018-4082-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-018-4082-x