Abstract
Purpose
To evaluate and compare the temporal changes in pulse waveform parameters of ocular blood flow (OBF) between non-habitual and habitual groups due to caffeine intake.
Method
This study was conducted on 19 healthy subjects (non-habitual 8; habitual 11), non-smoking and between 21 and 30 years of age. Using laser speckle flowgraphy (LSFG), three areas of optical nerve head were analyzed which are vessel, tissue, and overall, each with ten pulse waveform parameters, namely mean blur rate (MBR), fluctuation, skew, blowout score (BOS), blowout time (BOT), rising rate, falling rate, flow acceleration index (FAI), acceleration time index (ATI), and resistive index (RI). Two-way mixed ANOVA was used to determine the difference between every two groups where p < 0.05 is considered significant.
Result
There were significant differences between the two groups in several ocular pulse waveform parameters, namely MBR (overall, vessel, tissue), BOT (overall), rising rate (overall), and falling rate (vessel), all with p < 0.05. In addition, the ocular pulse waveform parameters, i.e., MBR (overall), skew (tissue), and BOT (tissue) showed significant temporal changes within the non-habitual group, but not within the habitual group. The temporal changes in parameters MBR (vessel, tissue), skew (overall, vessel), BOT (overall, vessel), rising rate (overall), falling rate (overall, vessel), and FAI (tissue) were significant for both groups (habitual and non-habitual) in response to caffeine intake.
Conclusion
The experiment results demonstrated caffeine does modulate OBF significantly and response differently in non-habitual and habitual groups. Among all ten parameters, MBR and BOT were identified as the suitable biomarkers to differentiate between the two groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Caffeine is associated to promote alertness, attention, and task-switching [1]. It is estimated that an average cup of coffee contains 100 mg of caffeine. Approximately, 240 ml of brewed coffee contains 72 to 130 mg of caffeine while a shot of espresso contains 58 to 76 mg of caffeine. Caffeine is known for its effect on blood flow in the body. Caffeine increases blood vessel resistance and decreases blood flow in the human optical nerve head (ONH) [2] and there is a significant vasoconstriction response of the retinal vessel diameter 1 h after an intake of 200 mg caffeine in young healthy subjects [3]. There were studies on tolerance of caffeine among habitual consumers and comparison between those with different levels of caffeine consumption [4]. However, the difference in ocular blood flow (OBF) changes as a result of caffeine intake between non-habitual and habitual consumers is not known.
Laser speckle flowgraphy (LSFG) is a non-invasive method to quantify the velocity of blood flow in the ONH without the need of using any pupil dilation agent [5, 6]. The LSFG uses laser speckle phenomenon, an interference event where coherent light sources such as lasers are scattered by a diffusing surface, thus producing speckle pattern, which can be described statistically. In accordance with the movement of blood cells in the tissue, the structure of the speckle pattern varies according to blood flow velocity. The mean blur rate (MBR) represents the index of the blood velocity. Hence, the greater the movement of red blood cells, the higher rate of MBR. The LSFG device captures MBR images at 30 frames per second for a period of 4 s and its embedded software synchronizes the images with cardiac cycles. The averaged MBR of a heartbeat are displayed as heartbeat map and provides pulse waveform parameters [5].
The aim of this study is to evaluate the effects of caffeine on OBF between non-habitual and habitual caffeine consumers. Caffeine capsules were used to induce changes of OBF. To our best knowledge, this is the first comparative study about how ocular blood flow pulse waveform parameters differ in time series between habitual and non-habitual caffeine consumers.
Methods
Subjects
Healthy subjects (age 21–30) with no medical condition or history were recruited. Habitual coffee consumption was defined as daily coffee consumption, and non-habitual coffee consumption was defined as non-daily coffee consumption [7]. In this study, we defined habitual caffeine consumers as those who consumed more than three cups of coffee per day and non-habitual as those who do not take coffee or tea beverages at all. Exclusion criteria include any physical, mental, and eye diseases; intake of medications; smokers; obesity; and known hypersensitivity to caffeine. In total, 19 subjects were recruited; 8 subjects were classified as non-habitual consumers and 11 subjects were classified as habitual consumers. All subjects were briefed about the purpose, processes, and risks before the start of the study.
Study protocol
The subjects were instructed not to consume any alcohol, energy, and carbonated drinks 1 week before (for the habitual group) and abstained from caffeinated beverages and vigorous physical activities 24 h before the experiment. This is to ensure washout period from previous caffeine consumption [8]. Next, subjects were instructed to have at least 6 h of sleep and female subjects confirmed not to be on a menstrual cycle. Subjects were allowed to have breakfast but with only plain water 2 h before the experiment. All experiments were carried out at the same time each day to avoid diurnal variation effect. All laboratory sessions started at 10 a.m. The session took place in a dark, quiet room with an ambient temperature maintained at 24 °C. Upon arrival, each subject was given 15-min rest in the room to maintain normal blood pressure. Blood pressure and several LSFG readings were taken 10 min before the experiment started. The session then started by giving two capsules of caffeine, equivalent in total to 180 mg of caffeine together with 200 ml of mineral water and LSFG measurements were taken immediately (marked as time point t1, 0 min). LSFG measurements were taken every 20 min for 2 h as shown in Fig. 1.
Caffeine capsule
Caffeine capsule used in this study is 250 mg guarana seed extract capsule (GNC Live Well Pharmacy, Malaysia)—vegetable capsule contained 36% (90 mg) of caffeine per capsule. Guarana capsule is a natural source of caffeine, which has the invigorating properties to promote stamina and physical performance [9]. The reason for using caffeine capsules is to avoid bias and to standardize the actual amount of caffeine as brewed coffee does not have a standardized amount of caffeine. Besides, the taste and add-ins such as sugar and dairy may vary according to the subjects.
Laser speckle flowgraphy measurements
Each subject was sat comfortably with his/her head positioned on a chin rest. The laser speckle flowgraphy system LSFG-NAVI (Softcare Co., Ltd., Japan) was used to measure the ocular blood flow. The LSFG-NAVI system was adjusted according to eye position. The subject’s head was then covered over with a lightweight dark scarf. LSFG measurements were taken in a dark room and were performed only on the right eyes for all subjects. Full ONH was fit to be captured within the frame and the focus was adjusted by looking at the live-capture image. The focus of the image was adjusted during the real-time image to eliminate any gap which otherwise appeared as horizontal dark lines [10]. Each LSFG measurement was taken over a period of 4 s and three consecutive recordings were acquired at each time point. LSFG analyzer software (LSFG analyzer Version 3.1.58; Softcare Co., Ltd., Japan) automatically detected the beginning and the end of each cardiac cycle which were recorded within the 4-s period and identical phases of cardiac cycle images were normalized to one image sequence representing a complete cardiac cycle. Average of signal intensity over the complete cardiac cycle was calculated producing a composite map, which represented the distribution of mean blood flow in one complete cardiac cycle in ONH [11]. An ellipse rubber band was manually set on ONH regions of interest, and pulse waveform parameters were extracted based on selected region of interest. Identical size and position of rubber bands were set for all subsequent images of the same subject. Through vessel segmentation function, pulse waveform parameters in vessel and tissue regions within the ONH area were determined. These were performed through digital cross-section analysis where it differentiated between visible vessels and tissue region within the ONH interest region. The pulse waveform parameter values of three separate regions were obtained: the overall (mean of all values), vessel, and tissue of the ONH (Fig. 2). The description and the calculation of each pulse waveform were described in detailed by Fukami [12].
Definition of ONH region of interest. a ONH in the whole frame, region of interest was selected using ellipse rubber band and extracted out. b ONH region of interest, defined as overall ONH. c Vessel segmentation of ONH region into vessel area (white) and tissue area (black) within rubber band. A set of 10 pulse waveform parameters from each of three region (overall, vessel, and tissue) were extracted out
Statistical analysis
Statistical analysis was performed using SPSS statistical software version 23. The data were observed to follow normal distribution and outliers were removed. Two-way mixed ANOVA was conducted to determine the significant difference between groups at different measuring time points. This was then confirmed with one-way repeated measure (or Friedman’s test) when normality is violated for each group of pulse waveform separately. Each pulse waveform was compared based on (i) between-subject factor (non-habitual and habitual groups) and (ii) within-subject factor (time points). In this study, p < 0.05 is considered to be significantly different [13]. For the graph, all values were averaged and normalized according to the baseline reading for each group separately to permit comparisons between groups.
Result
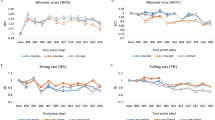
The analyses were based on the average of three captured images of 19 eyes (8 non-habitual and 11 habitual). The mean scores and standard deviation of each pulse waveform parameters were summarized for each region respectively (see supplementary table (Table S1, overall region; Table S2, vessel region; and Table S3, tissue region)). Graphs comparing two groups for each pulse waveform and region are presented in Figs. 3, 4, 5, 6, and 7.
Difference between non-habitual and habitual groups
The ocular pulse waveforms were analyzed separately based on the three defined regions and the following ten waveform parameters, namely mean blur rate (MBR), fluctuation, skew, blowout score (BOS), blowout time (BOT), rising rate, falling rate, flow acceleration index (FAI), acceleration time index (ATI), and resistive index (RI). Among all, several parameters that demonstrated significant difference between two groups are MBR (overall, vessel, and tissue regions), BOT (overall region), rising rate (overall region), and falling rate (vessel region), all with p < 0.05. All p values are summarized in Table 1.
Significant response to caffeine observed only in the non-habitual group
We identified several pulse waveform parameters that showed significant changes only in the non-habitual group in response to caffeine intake, i.e., MBR (overall), skew (tissue), BOS (tissue), and BOT (tissue). MBR for overall region showed a significant (p = 0.001) response at t5, 80 min after caffeine consumption. The skew in tissue region also showed significant difference (p = 0.013) between groups at multiple time points; the BOT in tissue region showed significant decrease within group (p = 0.005), and between groups at different time points (p = 0.007). Differences in p value between the groups are summarized in Table 2.
Significant response to caffeine intake regardless of being habitual or non-habitual
The following are pulse waveform parameters which have responded significantly to caffeine ingestion by both groups: the MBR in vessel region (non-habitual group, p = 0.01; habitual group, p = 0.024) and tissue region (non-habitual, p = 0.000 at t4, p = 0.05; t5, p = 0.05; t6, p = 0.027; and habitual, p = 0.001) shows significant difference; the skew in overall region (non-habitual, p = 0.0004; habitual, p = 0.002—Friedman, p = 0.01) and vessel region (non-habitual, p = 0.024; habitual, p = 0.015) both demonstrates significant increase; the BOT in overall (non-habitual, p = 0.0005; habitual, p = 0.015) and vessel regions (non-habitual, p = 0.004; habitual, p = 0.025) demonstrates significant decrease; the rising rate in overall region showed significant increase (non-habitual, p = 0.0021; habitual, p = 0.001) and temporal response showed significant difference between groups at time point t1, p = 0.000; t2, p = 0.002; and t3, p = 0.013; the falling rates in overall (non-habitual, p = 0.025; habitual, p = 0.002) and vessel regions (non-habitual-vessel, p = 0.007; habitual vessel, p = 0.007) both demonstrate significant increase and temporal response showed significant difference in mean at different time points, p = 0.000; the FAI in tissue region (non-habitual-tissue, p = 0.000; habitual, p = 0.047) and temporal response showed significant difference in mean at different time points, p = 0.000. p values reporting significant difference within groups at each region are summarized in Table 3.
Discussion
Our experimental results found that the pulse waveform parameters differing significantly between the two groups were MBR in all three different regions, BOT in overall region, rising rate in overall region, and falling rate in vessel region. Primarily, in this study, the index of blood velocity (i.e., MBR) demonstrated significant difference between these two groups in all three regions. Of overall region, the non-habitual group showed highly significant irregular temporal pattern of MBR, while no similar change was observed in the habitual group. Moreover, the non-habitual group had significant changes observed in several pulse waveform parameters, namely MBR (overall), skew (tissue), BOS (tissue), and BOT (tissue).
In response to caffeine ingestion, several pulse waveform parameters reacted significantly in both the groups. Some of them were more significant in the non-habitual group while the rest in the habitual group; the earlier include MBR (vessel and tissue regions), skew (overall), BOT (overall), and FAI (tissue); the latter were rising rate and falling rate. We further observed skew (overall and vessel regions) in both groups was significantly increase in time; when examined closer, skew in the non-habitual group was higher significantly compared to the habitual group, indicating that blood flow would rise in speed faster in the non-habitual than in the habitual group in response to caffeine. When blood flow rises quickly, both the rising rate and the falling rate also increase and descend quickly.
BOT represents how long the MBR stays above the average value over its entire waveform. High BOT indicates that the blood flow volume in the vasculature is at a high level for a long time between heartbeats [14]. In this study, BOT (overall and vessel regions) was observed to decrease over time in both the groups. However, the non-habitual group showed highly significant decrease when compared to the habitual group, and the mean BOT graph of both groups as plotted in Fig. 5 shows the BOT level of the habitual group is higher. These results validate that vessel resistance in the habitual group is stronger compared to that in the non-habitual group most likely as a result of the adaptation to long-term caffeine consumption. They also support the suggestion that the BOT can serve as an important vascular resistance biomarker [15]. Vessel resistances are essential in maintaining vascular homeostasis, ensuring sufficient blood flow for nutrient delivery. In turn, impaired vessel resistance will provide important information on retinal and cerebrovascular diseases [16].
Our experimental results are consistent with the exaggerated effect on cerebral blood flow due to caffeine as observed in non-habitual consumers while no effect shown in habitual consumers [17]. Cerebral blood flow was found to decrease in low and moderate caffeine consumers compared to high caffeine consumers. This can be explained where habitual caffeine consumers are known to adapt or tolerate the effect of caffeine on their bodies as long-term caffeine consumption promotes the additional build-up of adenosine receptors [18] to compensate the vasoconstriction effect due to caffeine intake [17]. Hence, it would take an extra dose of caffeine to exert the same effect as the non-habitual consumers. The study by Bell et al. [8] further showed that non-caffeine consumers benefit more from caffeine supplementation. Our experiment results demonstrated that the non-habitual group experienced a greater effect on OBF pulse waveform in comparison to the habitual group.
In this study, we excluded physiological factors such as gender, age, and BMI although they might affect MBR [11, 19]. For instance, smaller size individuals might have a greater effect of caffeine compared to larger size individuals. Furthermore, caffeine normally starts to take effect 15 min after ingestion; however, this varies depending on one’s individual metabolism. Some response with an acute rise in blood pressure, while some do not see increase in their blood pressure [3, 20]. Besides, to avoid diurnal variation, this study was conducted at the same time, i.e., 10 a.m., as several reports showed significant diurnal variation in healthy subjects, from 9 a.m. to 12 p.m. [21,22,23]. This is because heart rate is strongly correlated with LSFG pulse waveform as the number of frames, 30 per seconds reflect the duration of heartbeat [5], and heart rate is known to be low in the morning and high in the evening [22]. Next, increase in sympathetic activity will constrict blood vessels and the level of sympathetic activity is usually high in the morning [12, 24].
Admittedly, this study presents several limitations. First, all subject were university students and finding non-habitual caffeine subjects was challenging, leading to limited sample size. As such, the sample size was too small for subdivision of gender, for instance. Next, we did not compare the readings between both eyes as we assumed them to experience the same effect. Moreover, there was no comparison with other modalities to measure ocular blood flow and vascular changes such as optical coherence tomography.
In conclusion, despite the presence of variability in physiological factors such as gender, age, and BMI, this study demonstrates a significant microcirculation changes in ONH in terms of caffeine effects between habitual and non-habitual consumers. In addition, our results indicated pulse waveform parameters MBR and BOT might serve as important biomarkers to differentiate between non-habitual and habitual caffeine consumers.
References
McLellan TM, Caldwell JA, Lieberman HR (2016) A review of caffeine’s effects on cognitive, physical and occupational performance. Neurosci Biobehav Rev 71:294–312. https://doi.org/10.1016/j.neubiorev.2016.09.001
Okuno T, Sugiyama T, Tominaga M, Kojima S, Ikeda T (2002) Effects of caffeine on microcirculation of the human ocular fundus. Jpn J Ophthalmol 46(2):170–176
Terai N, Spoerl E, Pillunat LE, Stodtmeister R (2012) The effect of caffeine on retinal vessel diameter in young healthy subjects. Acta Ophthalmol 90(7):e524–e528. https://doi.org/10.1111/j.1755-3768.2012.02486.x
Kennedy DO, Haskell CF (2011) Cerebral blood flow and behavioural effects of caffeine in habitual and non-habitual consumers of caffeine: a near infrared spectroscopy study. Biol Psychol 86(3):298–306. https://doi.org/10.1016/j.biopsycho.2010.12.010
Sugiyama T, Araie M, Riva CE, Schmetterer L, Orgul S (2010) Use of laser speckle flowgraphy in ocular blood flow research. Acta Ophthalmol 88(7):723–729. https://doi.org/10.1111/j.1755-3768.2009.01586.x
Sato T, Sugawara J, Aizawa N, Iwama N, Takahashi F, Nakamura-Kurakata M, Saito M, Sugiyama T, Kunikata H, Nakazawa T, Yaegashi N (2017) Longitudinal changes of ocular blood flow using laser speckle flowgraphy during normal pregnancy. PLoS One 12(3):e0173127. https://doi.org/10.1371/journal.pone.0173127
Zimmermann-Viehoff F, Thayer J, Koenig J, Herrmann C, Weber CS, Deter HC (2016) Short-term effects of espresso coffee on heart rate variability and blood pressure in habitual and non-habitual coffee consumers—a randomized crossover study. Nutr Neurosci 19(4):169–175. https://doi.org/10.1179/1476830515Y.0000000018
Bell DG, McLellan TM (2002) Exercise endurance 1, 3, and 6 h after caffeine ingestion in caffeine users and nonusers. J Appl Physiol 93(4):1227–1234. https://doi.org/10.1152/japplphysiol.00187.2002
Portella Rde L, Barcelos RP, da Rosa EJ, Ribeiro EE, da Cruz IB, Suleiman L, Soares FA (2013) Guarana (Paullinia cupana Kunth) effects on LDL oxidation in elderly people: an in vitro and in vivo study. Lipids Health Dis 12:12. https://doi.org/10.1186/1476-511X-12-12
Aizawa N, Yokoyama Y, Chiba N, Omodaka K, Yasuda M, Otomo T, Nakamura M, Fuse N, Nakazawa T (2011) Reproducibility of retinal circulation measurements obtained using laser speckle flowgraphy-NAVI in patients with glaucoma. Clin Ophthalmol 5:1171–1176. https://doi.org/10.2147/OPTH.S22093
Luft N, Wozniak PA, Aschinger GC, Fondi K, Bata AM, Werkmeister RM, Schmidl D, Witkowska KJ, Bolz M, Garhofer G, Schmetterer L (2016) Ocular blood flow measurements in healthy white subjects using laser speckle flowgraphy. PLoS One 11(12):e0168190. https://doi.org/10.1371/journal.pone.0168190
Fukami M, Iwase T, Yamamoto K, Kaneko H, Yasuda S, Terasaki H (2017) Changes in retinal microcirculation after intravitreal ranibizumab injection in eyes with macular edema secondary to branch retinal vein occlusion. Invest Ophthalmol Vis Sci 58(2):1246–1255. https://doi.org/10.1167/iovs.16-21115
Laerd S (2015) Two-way mixed ANOVA using SPSS statistics. Statistical tutorials and software guides. https://statistics.laerd.com/premium/spss/twma/two-way-mixed-anova-in-spss-24.php. Accessed 8 Jan 2018
Tsuda S, Kunikata H, Shimura M, Aizawa N, Omodaka K, Shiga Y, Yasuda M, Yokoyama Y, Nakazawa T (2014) Pulse-waveform analysis of normal population using laser speckle flowgraphy. Curr Eye Res 39(12):1207–1215. https://doi.org/10.3109/02713683.2014.905608
Enaida H, Nagata S, Takeda A, Nakao S, Ikeda Y, Ishibashi T (2016) Changes in chorioretinal blood flow velocity and cerebral blood flow after carotid endarterectomy. Jpn J Ophthalmol 60(6):459–465. https://doi.org/10.1007/s10384-016-0472-y
Bettermann K, Slocomb J, Shivkumar V, Quillen D, Gardner TW, Lott ME (2017) Impaired retinal vasoreactivity: an early marker of stroke risk in diabetes. J Neuroimaging : Official J Am Soc Neuroimaging 27(1):78–84. https://doi.org/10.1111/jon.12412
Addicott MA, Yang LL, Peiffer AM, Burnett LR, Burdette JH, Chen MY, Hayasaka S, Kraft RA, Maldjian JA, Laurienti PJ (2009) The effect of daily caffeine use on cerebral blood flow: how much caffeine can we tolerate? Hum Brain Mapp 30(10):3102–3114. https://doi.org/10.1002/hbm.20732
Meredith SE, Juliano LM, Hughes JR, Griffiths RR (2013) Caffeine use disorder: a comprehensive review and research agenda. J Caffeine Res 3(3):114–130. https://doi.org/10.1089/jcr.2013.0016
Yanagida K, Iwase T, Yamamoto K, Ra E, Kaneko H, Murotani K, Matsui S, Terasaki H (2015) Sex-related differences in ocular blood flow of healthy subjects using laser speckle flowgraphy. Invest Ophthalmol Vis Sci 56(8):4880–4890. https://doi.org/10.1167/iovs.15-16567
Chandrasekaran S, Rochtchina E, Mitchell P (2005) Effects of caffeine on intraocular pressure: the Blue Mountains Eye Study. J Glaucoma 14(6):504–507
Pemp B, Georgopoulos M, Vass C, Fuchsjager-Mayrl G, Luksch A, Rainer G, Schmetterer L (2009) Diurnal fluctuation of ocular blood flow parameters in patients with primary open-angle glaucoma and healthy subjects. Br J Ophthalmol 93(4):486–491. https://doi.org/10.1136/bjo.2008.148676
Fukami M, Iwase T, Yamamoto K, Ra E, Murotani K, Terasaki H (2017) Diurnal variation of pulse waveform parameters determined by laser speckle flowgraphy on the optic nerve head in healthy subjects. Medicine 96(44):e8312. https://doi.org/10.1097/MD.0000000000008312
Iwase T, Yamamoto K, Ra E, Murotani K, Matsui S, Terasaki H (2015) Diurnal variations in blood flow at optic nerve head and choroid in healthy eyes: diurnal variations in blood flow. Medicine 94(6):e519. https://doi.org/10.1097/MD.0000000000000519
Panza JA, Epstein SE, Quyyumi AA (1991) Circadian variation in vascular tone and its relation to alpha-sympathetic vasoconstrictor activity. N Engl J Med 325(14):986–990. https://doi.org/10.1056/NEJM199110033251402
Funding
The project was funded by the Ministry of Higher Education Malaysia under HICoE scheme to CISIR. The sponsor had no role in the design or conduct of the research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
ESM 1
(DOCX 28.7 kb)
Rights and permissions
About this article
Cite this article
Ismail, A., Bhatti, M.S., Faye, I. et al. Pulse waveform analysis on temporal changes in ocular blood flow due to caffeine intake: a comparative study between habitual and non-habitual groups. Graefes Arch Clin Exp Ophthalmol 256, 1711–1721 (2018). https://doi.org/10.1007/s00417-018-4030-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-018-4030-9