Abstract
Purpose
The XEN45 Gel Stent is a flexible hydrophilic tube placed under the conjunctiva via the anterior chamber. This study investigates the IOP (intraocular pressure)-lowering potential, the risk profile, and the success rate of the XEN45 Gel Stent.
Methods
Two hundred and sixty-one eyes underwent surgery. The mean follow-up time was 8.5 months. The aim of the treatment was to achieve adequate IOP reduction without medication. Therefore, all patients who did not show sufficiently reduced IOP underwent a surgical revision with opening of the conjunctiva. To determinate the success rate, we carried out two kinds of analysis: 1) the primary success rate: eyes with appropiate IOP control without medication or surgical revision, and 2) overall success rate: one surgical revision was allowed.
Results
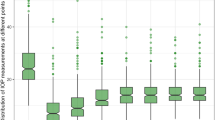
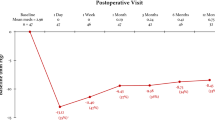
Intraocular pressure was lowered from 24.3 mmHg (SD 6.6) to 16.8 mmHg (SD 7.6), and the medication score was lowered from 2.6 (SD 1.1) to 0.2 (SD 0.7). Revisional surgery was performed in 80 eyes (34%). After a first revision, intraocular pressure was lowered to 14.0 mmHg (SD 5.1), and the medication score was lowered to 0.2 (SD 0.6). The primary success rate was 66% and the overall success rate 90%. The primary success rate was higher in pseudophakic eyes (73%) than in phakic eyes (53%) or combined surgery (55%).
Conclusions
We conclude from our data that the XEN45 Gel Stent has an IOP-lowering potential and few side-effects. Pseudophakic eyes seem to have a better primary prognosis compared to combined surgery or surgery in phakic eyes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Minimally invasive glaucoma surgery has become more popular in recent years. Trabectome (NeoMedix Corporation, Tustin, CA, USA) and iStent inject (Glaukos Corp., Laguna Hills, CA, USA) are recent developements in glaucoma surgery of the iridocorneal angle. They are regarded as safe techniques leading to a reduction of intraocular pressure (IOP).
However, they did not reach the low level of IOP which can be achieved by filtering surgery, especially by a trabeculectomy, which is regarded as the most common surgical or gold standard procedure in uncontrolled glaucoma [1,2,3,4]. These minimally invasive glaucoma surgery (MIGS) techniques do not ensure that the patient will no longer require pressure-lowering medication postoperatively. Several approaches were developed in the past to achieve a minimally invasive filtering surgery using varying caliber XEN Gel Stents. The XEN Gel Stent is a hydrophilic tube composed of a porcine gelatin crosslinked with glutaraldehyde and believed to cause no foreign body reaction. It is 6 mm long and has an outer diameter of 220 μm [5]. First studies reported the pressure-lowering effect of the XEN140 and XEN63 Gel Stents with a lumen diameter of 140 or 63 μm, respectively [6, 7]. The stent underwent further developments and is nowadays offered as the XEN45 Gel Stent (Allergan, CA, USA), which is a 6 mm flexible gelatine tube with a lumen of 45 μm diameter. The stent is 100 times more flexible than a silicone tube shunt. This characteristic, combined with the small outer diameter, promises minimal stress to the surrounding tissue, thus preventing erosion and migration [5]. According to the law of Hagen–Poiseuille, the stent is designed to avoid hypotony without a valve system. A reduced flow rate preserves an IOP level above 7.6 mmHg at a physiological flow rate of 2.5 μl/min, compared to a Baerveldt tube or Express shunt with an IOP level of 0.01 or 0.09 mmHg at a flow rate of 2.5 μl/min. Therefore, the authors concluded that the XEN45 stent creates a flow which should not lead to hypotony levels [8].
The stent is placed ab interno under the conjunctiva in the nasal superior quadrant by an injector system through the clear cornea via the anterior chamber angle. The stent immediately leads to a filtration zone from the anterior chamber under the conjunctiva without injuring it (Fig. 1). While using the same pathway as in a trabeculectomy, the most obvious difference lies in the fact that a foreign body is left in the tissue. This study investigates the IOP-lowering potential, the risk profile, and the success rate of the XEN45 Gel Stent.
Patients and methods
This is a retrospective single center study investigating the IOP-lowering potential, the risk profile, and success rate of the XEN45 Gel Stent in glaucoma patients. Our Ethics Committee ruled that their approval was not required in this study. Informed consent was obtained from all individual participants included in the study.
Our research was consistent with the tenets of the Declaration of Helsinki.
From 2015 until 2017, a total of 261 eyes underwent surgery with the XEN45 Gel Stent alone or XEN45 Gel Stent combined with phacoemulsification at the St. Martinus-Hospital in Düsseldorf, Germany. During this period XEN Gel Stent surgery replaced trabeculectomy in patients requiring filtering surgery at our center. Follow-up appointments were scheduled after 1 month, 3 months, 6 months, 12 months and 18 months after surgery. Patients were seen at shorter intervals when they did not show a proper filtering zone. Patients were also seen by their referring doctors at other times.
All patients with a minimal follow-up period of 1 month or who presented earlier because of a bleb failure were included in this study. Two hundred and thirty-four eyes of 261 patients were left for analysis. These were open-angle glaucomas, including eyes with pseudoexfoliation glaucoma (n = 44), secondary glaucoma (n = 6), juvenile glaucoma (n = 1) and pigmentary glaucoma (n = 2).
Surgery was performed as a stand-alone procedure in pseudophakic eyes (n = 139) and in phakic eyes (n = 45), or as a combination procedure with cataract surgery and lens implantation (n = 49).
Some eyes had had prior surgery: selective laser trabeculoplasty and Argon laser trabeculoplasty (n = 39), Trabectome surgery (n = 31), trabeculectomy (n = 17), pars plana vitrectomy (n = 6) and deep sclerectomy (n = 6).
The mean follow-up of these eyes was 8.5 (SD 5.9) months, with a range between 1 and 23 months. The mean age of the patients was 73 years (SD 11), mean visual acuity 0.4 logMAR (SD 0.5), mean IOP 24.3 mmHg (SD 6.6), mean medication score 2.6 (SD 1.1) and mean cup to disc ratio of 0.8 (SD 0.2) prior to surgery. There were 141 eyes of women and 92 eyes of men.
The IOP was measured by Goldmann applanation tonometry. The preoperative value was the mean value of the last three preoperative measurements. Visual acuity was measured by standard Snellen charts.
During XEN Gel Stent surgery as a stand-alone procedure, first 0.1 ml mitomycin C (0.1 mg/ml) was injected under the conjunctiva, 6 mm from the limbus. Then a temporal paracentesis and a paracentesis at the 5 or 7 o’clock position were made. After filling the anterior chamber with high-viscosity viscoelastic, the stent was placed with the injector. The apex of the injector was pushed through the trabecular meshwork and through the sclera, aiming a 3 mm distance from the limbus. Then the stent was injected under the conjunctiva and the injector removed from the anterior chamber. The position of the stent was confirmed by gonioscopy, and the viscoelastic substance was removed by irrigation.
Performing combined XEN Gel Stent and cataract surgery, a 2.8 mm temporal corneal incision was made after mitomycin C was injected under the conjunctiva. Two paracenteses were positioned at 12 and 6 o’clock. After standard phacoemulsification and lens implantation, the procedure was performed as described above.
All patients received an antibiotic and a steroidal ointment three times daily after surgery. The pressure lowering medication was discontinued.
Following discharge, the patients were seen after 1 month, 3 months, 6 months, 12 months and 18 months, and by their referring doctors at other times.
The clinical endpoint of the study was the intraocular pressure. The aim of the treatment was adequate IOP reduction without medical treatment. Therefore, all patients who did not present with sufficiently reduced intraocular pressure underwent a surgical revision. The revision started with preparation of the conjunctiva from the limbus as we would do during a trabeculectomy. Scar tissue was removed from the stent and the conjunctiva was refixated at the limbus with two 9.0 absorbable sutures.
The success rates were defined based on different scores, so that they might be comparable to other studies. Score A equals the number of eyes which did not need a revision and showed a proper IOP according to their glaucoma stage. We also calculated scores B, C, and D. Success according to scores B, C, and D is defined as no re-surgery and depending on IOP reduction and the IOP at follow-up. This means for score B IOP reduction > 20%, IOP < 18, no resurgery; for score C IOP reduction > 20%, IOP < 21 mmHG. Score D means IOP reduction ≥ 40%, IOP ≤ 15 mmHg, which is in accordance with the criteria of the World Glaucoma Association [9].
The results in terms of visual acuity, medication score, and success rates are presented in two ways. First, we analyzed the results assuming that a revison is a re-surgery and therefore a failure (primary success). Second, we anticipated one revison as part of the treatment strategy and thus did not regard it as a failure (overall success). If more than one revision was necessary, we regarded this a failure.
Statistical analysis was carried out using the paired t-test and the chi square test with the software package Graphpad Prism 6.0 (Graphpad Software Inc., San Diego, CA, USA).
Results
Intraocular pressure and medication score were significantly (p < 0.001) reduced at mean follow-ups of 8.5 months (range 1–23). Intraocular pressure was lowered from 24.3 mmHg (SD 6.6) to 16.8 mmHg (SD 7.7), and the medication score was significantly (p < 0.001) lowered from 2.6 (SD 1.1) to 0.2 (SD 0.7). After a first revision, intraocular pressure was lowered (p < 0.001) to 14.0 mmHg (SD 5.1), and the medication score was lowered (p < 0.001) to 0.2 (SD 0.6). The changes of IOP over time are presented in Table 1. The primary success rate was 66% (revision regarded as a failure) and the overall success rate 90% (one revision allowed). Success rates with all criteria are shown in Table 2 and Table 3. The primary success rate was higher in pseudophakic eyes receiving a stand-alone procedure (73% success) compared to phakic eyes receiving a stand-alone procedure (53% success) or combined procedures in phakic eyes (55% success). Dividing the eyes into pseudophakic and phakic eyes, the difference was statistically significant (p = 0.002).
The rate of surgical revision was 34% (80 eyes), and the rate of more than one surgical revision or with another pressure-lowering surgical method after the first revision was 10% (23 eyes). The mean time interval between stent implantation and revisional surgery was 5.0 months (SD 4.2), and the mean time interval between revisional surgery and last follow-up was 5.2 months (SD 4.8).
The overall success rate of all eyes with previous glaucoma surgery according to score A, B, C, and D was 88%, 84%, 86%, and 55% after trabeculoplasty, 100%, 96%, 100%, and 60% after trabeculectomy/sclerectomy, and 87%, 84%, 87%, and 47% after trabectome.
Side effects are listed in Table 4. Postoperative hyphaema occurred and resolved spontaneously. One eye presented with a shallow anterior chamber and required a filling with viscoelastics in the early postoperative period. After the procedure, the anterior chamber remained stable. Choroidal detachment resolved within the first 2 weeks and did not require intervention. Twenty of 225 eyes showed an avascular filtering bleb (Fig. 2). Two stents eroded the conjunctiva (Fig. 3). Both were removed immediately. One patient received a new stent and developed a filtration bleb. The other patient developed a filtration bleb without a new stent.
Discussion
In our study, the XEN45 Gel Stent was able to lower intraocular pressure to values between 13 and 15 mmHg after a mean follow-up of 8.3 months. This is comparable to previous findings of Perez-Torregrosa and coworkers after combined surgery with the XEN45 stent in a small case series [10].
Gedde and coworkers found that the mean IOP one year after trabeculectomy was 12.7 mmHg with a medication score of 0.5 during the Tube versus Trabeculectomy study [3]. Kaplowitz and coworkers described a mean IOP around 16 mmHg with a medication score less than one after Trabectome surgery, and Arriola-Villalobos and coworker reported a final mean IOP of 16.75 mmHg after surgery utilizing the iStent [4]. In conclusion, the IOP decrease to values between 13 and 15 mmHg following the XEN Gel Stent implantation seems to be higher than after a trabeculectomy but lower than following MIGS surgery modifying the anterior chamber angle [3, 4, 11].
The XEN Gel Stent has the potential to keep the patient free of IOP-lowering medication which is not the case in other MIGS procedures [10, 12].
Comparing the success rates of our subgroups, we found that the XEN Gel Stent in pseudophakic eyes has the most favorable primary success rate compared to phakic eyes and combined surgery with phacoemulsification. This has influenced our treatment schedule to such an extent that, in phakic eyes with glaucoma which require cataract surgery, we prefer to combine it with a chamber angle procedure such as Trabectome or iStent Inject. These procedures leave the conjunctiva untouched, and therefore a XEN stent or filtering surgery can follow later without disadvantages [13].
The implantation of the XEN Gel Stent follows the principles of filtering surgery and involves a quadrant of conjunctiva. Therefore, in our opinion a comparison to filtering surgery appears appropriate. Our goal was to gain an adequate IOP without medication postoperatively. If this was not achieved, we strictly recommended surgical revision, which led to a rate of 34% revisional surgery. This is comparable to a previous publications reporting needling rates of 31% and 43% [14, 15].
However, in our patients we found that needling alone did not sufficiently impact the massive scar tissue to ensure a working filtering bleb. Therefore, we devised a technique opening the conjunctiva from the limbus similar to a trabeculectomy starting from a limbal incision towards the stent emersion point, where we frequently found the stent surrounded by solid scar tissue (Fig. 4).
We removed all scar tissue entirely from the stent, which usually appeared fully functional. Finally, the conjunctiva was refixated with two absorbable sutures.
It was striking that large filtering zones developed after this kind of revisional surgery, usually even larger after this revision procedure than after the initial stent positioning. Therefore, we adopted surgical scar removal as our treatment strategy in all patients with scarring of the bleb following XEN Gel Stent surgery.
Now, patients are informed prior to surgery that there is a 34% revision rate. Accepting this as a treatment strategy in XEN stent implantation, we found success rates between 84 and 92% in all subgroups, with an advantage in pseudophakic eyes over phakic eyes and over eyes with combined surgery in scores B, C, and D.
Postoperative bleeding and choroidal detachment occurred after surgery but resolved spontaneously. There was one patient with a shallow anterior chamber, and a viscoelastic agent was instilled to protect the lens in a phakic eye. There was no other eye with a shallow anterior chamber. Macula edema in four eyes occurred only after combined surgery and not following stand-alone procedures, implying post-phacoemulsification Irvine–Gass syndrome as the most likely reason for macula edema. In our opinion, side-effects are few and usually do not require intervention, as they do in trabeculectomy [16].
However, one special clinical finding did require immediate intervention. In two patients, the stent eroded the conjunctiva and was removed. In one eye, a new stent was successfully implanted. In the other eye, a filtering bleb showed and remained even after stent explantation. The management of these two cases was uneventful, but in principle there is a potential for endophthalmitis when erosion of the conjunctiva occurs, which makes an immediate revision inevitable. During postoperative follow-up examinations, characteristic warning signs may reveal the process of a stent eroding the conjunctiva. In the beginning, patients present with a thin mitomycin-induced avascular conjunctiva, with the stent superficially pressing against the outer wall of the thin filtering bleb.
These patients should be monitored closely or be considered for revision straight away. In one patient, we performed revisional surgery prior to a potential extrusion of the stent through the conjunctiva.
In former reports without erosion of the conjunctiva, surgery was conducted without mitomycin [6, 7]. Due to the fact that mitomycin alters the conjunctiva, erosion predominantly occurs in patients with an avascular conjunctiva. The injection of mitomycin carries the risk of an avascular conjunctiva which is vulnerable even to a small and pliable stent. An important criterion of minimally invasive glaucoma surgery is that the conjunctiva is conserved [7]. The XEN implant can compromise the conjunctiva from the effects of Mitomycin. Whether the XEN is really a MIGS procedure is debatable.
We conclude from our data that the XEN Gel Stent has IOP-lowering potential and few side-effects. Because there were no serious side-effects in this large cohort study, one might conclude that XEN Gel Stent surgery might have fewer risks than trabeculectomy, although a recent study comparing the side-effects of XEN Gel Stent surgery with trabeculectomy did not show a difference [15]. As the aim is complete omission of anti-glaucoma medication, re-surgery is necessary in 27% of pseudophakic eyes and in 47% of phakic eyes or 45% after combined surgery.
Since we did not permit pressure-lowering medication after surgery, we cannot estimate the outcome with additional medical therapy.
Other limitations of the study are the heterogeneity of the patients and the short follow-up time, with the inclusion of patients with a follow-up of 1 month. There is a paucity of published studies on the XEN Gel Stent to date. Therefore, we felt that this analysis provides an impression on how to handle these patients and how to discuss the expectations with the patient.
In our clinical routine, we use the XEN Gel Stent when filtering surgery is necessary, but we explain to the patient that around 34% of patients require additional surgery, with a favorable prognosis and success rates between 84 and 92%.
We conclude from our data that pseudophakic eyes have a better primary prognosis compared to combined surgery or surgery in phakic eyes. Therefore, it might be an option to use cataract surgery combined with angle-related surgery, keeping in mind that later XEN stent surgery is possible with a better outcome in the pseudophakic eye. Further investigation is recommended into whether the opening of the conjunctiva and the removal of scar tissue has a more favorable outcome than needling, or if the injection of 5 FU after surgery enhances the success rates.
Abbreviations
- IOP:
-
intraocular pressure
- SD:
-
standard deviation
- MIGS:
-
minimally invasive glaucoma surgery
References
Kirwan JF, Lockwood AJ, Shah P et al (2013) Trabeculectomy in the 21st century: a multicenter analysis. Ophthalmology 120:2532–2539. https://doi.org/10.1016/j.ophtha.2013.07.049
Grehn F (2008) Surgery of primary open angle glaucoma. Klin Monatsbl Augenheilkd 225:30–38. https://doi.org/10.1055/s-2008-1027124
Gedde SJ, Schiffman JC, Feuer WJ et al (2009) Three-year follow-up of the tube versus trabeculectomy study. Am J Ophthalmol 148:670–684. https://doi.org/10.1016/j.ajo.2009.06.018
Kaplowitz K, Bussel II, Honkanen R et al (2016) Review and meta-analysis of ab-interno trabeculectomy outcomes. Br J Ophthalmol 100(5):594–600. https://doi.org/10.1136/bjophthalmol-2015-307131
Lewis RA (2014) Ab interno approach to the subconjunctival space using a collagen glaucoma stent. J Cataract Refract Surg 40:1301–1306. https://doi.org/10.1016/j.jcrs.2014.01.032
Sheybani A, Lenzhofer M, Hohensinn M et al (2015) Phacoemulsification combined with a new ab interno gel stent to treat open-angle glaucoma: pilot study. J Cataract Refract Surg 41:1905–1909. https://doi.org/10.1016/j.jcrs.2015.01.019
Sheybani A, Dick HB, Ahmed IIK (2016) Early clinical results of a novel Ab Interno gel stent for the surgical treatment of open-angle glaucoma. J Glaucoma 25:e691–e696. https://doi.org/10.1097/IJG.0000000000000352
Sheybani A, Reitsamer H, Ahmed IIK (2015) Fluid dynamics of a novel micro-fistula implant for the surgical treatment of glaucoma. Invest Ophthalmol Vis Sci 56:4789–4795. https://doi.org/10.1167/iovs.15-16625
Shaarawy TM, Grehn F, Sherwood MB (2009) Guidelines on design and reporting of glaucoma surgical trials. Kugler Publications, The Hague
Pérez-Torregrosa VT, Olate-Pérez Á, Cerdà-Ibáñez M et al (2016) Combined phacoemulsification and XEN45 surgery from a temporal approach and 2 incisions. Arch Soc Esp Oftalmol 91:415–421. https://doi.org/10.1016/j.oftal.2016.02.006
Arriola-Villalobos P, Martinez-De-La-Casa JM, Díaz-Valle D et al (2012) Combined iStent trabecular micro-bypass stent implantation and phacoemulsification for coexistent open-angle glaucoma and cataract: a long-term study. Br J Ophthalmol 96:645–649. https://doi.org/10.1136/bjophthalmol-2011-300218
Gonnermann J, Bertelmann E, Pahlitzsch M et al (2017) Contralateral eye comparison study in MICS & MIGS: Trabectome® vs. iStent inject®. Graefes Arch Clin Exp Ophthalmol 255:359–365. https://doi.org/10.1007/s00417-016-3514-8
Jea SY, Mosaed S, Vold SD, Rhee DJ (2012) Effect of a failed trabectome on subsequent trabeculectomy. J Glaucoma 21:71–75. https://doi.org/10.1097/IJG.0b013e31820bcfda
Galal A, Bilgic A, Eltanamly R, Osman A (2017) XEN glaucoma implant with Mitomycin C 1-year follow-up: result and complications. J Ophthalmol 2017:5457246. https://doi.org/10.1155/2017/5457246
Schlenker MB, Gulamhusein H, Conrad-Hengerer I et al (2017) Efficacy, safety, and risk factors for failure of standalone Ab Interno gelatin microstent implantation versus standalone trabeculectomy. Ophthalmology 124:1579–1588. https://doi.org/10.1016/j.ophtha.2017.05.004
Gedde SJ, Herndon LW, Brandt JD et al (2012) Postoperative complications in the tube versus trabeculectomy (TVT) study during five years of follow-up. Am J Ophthalmol 153:804.e1–814.e1. https://doi.org/10.1016/j.ajo.2011.10.024
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the national research committee (Zentrale Ethikkommission der Bundesärztekammer) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Widder, R.A., Dietlein, T.S., Dinslage, S. et al. The XEN45 Gel Stent as a minimally invasive procedure in glaucoma surgery: success rates, risk profile, and rates of re-surgery after 261 surgeries. Graefes Arch Clin Exp Ophthalmol 256, 765–771 (2018). https://doi.org/10.1007/s00417-018-3899-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-018-3899-7