Abstract
Purpose
Recently, optical coherence tomography angiography (OCTA) has been used to successfully delineate vessels within the retina. This current study aims to assess corneal vascularization secondary to herpetic keratitis pre- and post-treatment using serial OCTA imaging adapted for the anterior segment.
Methods
All eyes were scanned using the split-spectrum amplitude decorrelation angiography (SSADA) algorithm on the AngioVue OCTA system (Optovue Inc. Fremont, CA, USA) with an anterior segment lens adapter. Multiple scans in the regions of interest (ROI) before and after treatment were analysed to assess change in corneal vascularization in response to each treatment modality.
Results
We analyzed a total of 12 OCTA scans in three eyes with corneal vascularization, comparing images pre- and 3 months post-treatment. We found that the OCTA was able to detect a significant decrease in area of vascularization in all eyes: including fine-needle diathermy (48 ± 7 to 41 ± 5 %, P = 0.048), subconjunctival bevacizumab (45 ± 7 to 38 ± 5 %, P = 0.015) and systemic steroid treatment following graft rejection (38 ± 1 to 32 ± 2 %, P = 0.003).
Conclusions
Our preliminary study of serial OCTA scans suggests that this may be a useful tool for objective quantification of corneal vascularization. Future development of image processing software will be needed for clinical use or trials to evaluate anti-vascular therapies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Optical coherence tomography (OCT) angiography is rapidly gaining popularity in the evaluation of retinal and retinal vascular diseases [1]. Its key feature is its ability to detect microvascular flow that was previously blocked by staining and leakage on flourescein angiography (FA), in the investigation, monitoring and treatment of retinal and choroidal vascular pathologies. In the cornea, a fine balance between angiogenic and anti-angiogenic factors maintains normal corneal vasculature and transparency [2]. Corneal vascularization represents pathological ingrowth of vessels in the normally avascular corneal stroma as a result of local expression of pro-angiogenic factors from a wide range of aetiologies: chemical injury, chronic hypoxic conditions from contact lens wear or even infections such as herpes or trachoma [3].
Although mild corneal vascularization may be asymptomatic, more severe forms predispose the cornea to inflammation, lipid exudation and scarring, leading to significant loss in visual function or even blindness. Furthermore, the loss of immune privilege compromises the success of subsequent transplants with higher rates of graft rejection [4]. Despite the variety of treatments available for corneal vascularization, there has yet to be a good non-invasive imaging technique for quantitative method of measuring corneal vascularization other than photography, to assess new interventions [5].
Current angiography techniques to visualise anterior segment vasculature mainly utilise intravenous injections of fluorescein and indocyanine green (ICG) [6]. However, these procedures are not only invasive, but require long acquisition times, with risks of serious adverse reactions, even in those with no risk factors or history of allergy. In our previous study, we described the novel technique of using split-spectrum amplitude decorrelation angiography (SSADA) to visualise normal limbal vasculature and corneal vascularization in a cross-sectional preliminary study with good repeatability and reproducibility results [7]. Therefore, this current study describes a prospective cases series of eyes with corneal vascularization comparing pre- and post-treatment with fine-needle diathermy, subconjunctival bevacizumab injections and oral steroidal therapy following graft rejection, to evaluate the use of serial OCTA imaging to monitor corneal vascular changes.
Materials and methods
We conducted this pilot prospective study in a case series of patients with corneal vascularization who were managed at Moorfields Eye Hospital from January 2015 to June 2015. All OCTA scans (6 × 6 mm volume cubes) were performed by the same operator on all subjects using the SSADA algorithm on the AngioVue OCTA system (Optovue Inc. Fremont, CA, USA) focused on the areas of corneal vascularization, with the anterior segment optical adaptor lens. This OCTA system is a non-invasive device with a scanning speed of 70,000 A-scans per second and is capable of providing volumetric flow information at a fixed point in time. The images are produced by comparing the decorrelation signals in sequential B-scans with an acquisition time of about 3 s. The system was calibrated by first selecting the Angiovue function. After the camera is fixed on the area of focus, “Auto F” and “Auto P” were selected in sequential order to automatically adjust the focus and polarization, respectively. Next, the B-scan reference is adjusted such that the corneal-limbal area is focused between the two red lines in the correct orientation and scans the area twice to produce the OCTA image. Each subject was reviewed clinically with OCTA images and the scans of corresponding areas in the region of interest (ROI), which were areas showing the most marked vascularization and analyzed comparing pre- and post-treatment. Our study adhered to the tenets of the Declaration of Helsinki and was conducted in accordance to human-subject research regulations and standards, with ethics approval obtained from our local Institutional Review Board.
All OCTA scans were automatically processed using the inbuilt program (ReVue, version 2014.2.0.15; Optovue Inc.) to reduce transverse saccadic and axial motion artefacts. Scans were then exported from the system as a portable image file into ImageJ 1.50b (NIH, Bethesda, MD) for analysis using our previously described protocol [8, 9]. Briefly, the ‘adjust threshold’ function was first applied to reduce the surrounding noise and highlight the blood vessels; and all images were converted to 8-bit type and the “FFT Bandpass Filter” function was used to remove motion artefacts [5]. Next, we used a selective filter to produce the vessels as a binary image, with pixel resolution (mm/pixel) defined as the ratio between the diameter of the cornea (mm) and the number of pixels measured from the image.
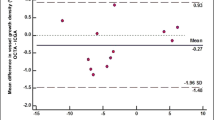
We analyzed all scan images and compared the average of the OCTA scans with the best signal strength pre- and post-treatment on 3-month follow-up after each intervention. Image analysis was performed in the various ROI using circular boundaries (1.5 mm radius) where the fractal dimension (Df) value, a measure of image complexity or how its detail changes with scale [6], and the area of vascularization was determined in percentages (%) within the ROI (‘1’ for black pixels over the vessels, ‘0’ for the white background) using a previously described method [10]. A P-value < 0.05 (paired t-test) was considered statistically significant for comparisons between pre- and post-treatment area of vascularization. Statistical Package for the Social Sciences version 17.0 (SPSS Inc., Chicago, IL) was used to analyze the data.
Results
In summary, we analyzed a total of 12 OCTA scans in eyes with corneal vascularization, comparing pre- and post-treatment. We found that the OCTA was able to detect a significant decrease in area of vascularization in all eyes 3 months post-treatment: including fine-needle diathermy (Case 1, 48 ± 7 to 41 ± 5 %, P = 0.048), subconjunctival bevacizumab (Case 2, 45 ± 7 to 38 ± 5 %, P = 0.015) and systemic steroid treatment following graft rejection (Case 3, 38 ± 1 to 32 ± 2 %, P = 0.003).
Case 1
A 46-year-old male with recurrent herpetic stromal keratitis developed large areas of secondary lipid keratopathy and scarring with corneal vascularization, evident at 12 o’clock (one prominent artery and vein) extending beyond the limbus and invading the central cornea; with another area of vascularization at 6 o’clock. The patient underwent successful fine-needle corneal vessel diathermy using a previously described method [7]. We found a significant decrease in area of vascularization (48 ± 7 % vs. 41 ± 5 %, P = 0.048) and decrease in Df value (1.883 vs. 1.873) comparing pre- and post-treatment OCTA scans, respectively.
Case 2
A 30-year-old female patient suffered herpetic keratitis that led to resultant corneal scarring with persistent vascularization and was treated with subconjunctival injection of bevacizumab using a recognized clinical protocol [11] Fig. 1. We observed pronounced vessel regression 3 months post-injection on slit-lamp examination with corresponding decrease in OCTA vascular measurements: Df value decreased from 1.878 to 1.862; while the area of vascularization decreased from 45 ± 7 to 38 ± 5 % (P = 0.015).
Example of serial optical coherence tomography angiography imaging in Case 2. a: Corneal scar with vascularization secondary to previous herpetic keratitis. b: Slit-lamp photograph after subconjunctival injection of bevacizumab. c: Optical coherence tomography angiography (OCTA) scan with region of interest (ROI, radius 1.5 mm) at the corneal limbus before treatment. d: Follow-up OCTA scan of the same ROI demonstrating significant decrease in area of vascularization
Case 3
A 42-year-old male with a history of herpetic keratitis presented 3 months after deep anterior lamellar keratoplasty with an episode of acute graft rejection, increased corneal graft vascularisation and mild anterior chamber activity. He was successfully treated with topical and systemic steroids with resolution of his clinical signs of graft rejection within 10 days. Comparison of OCTA scans pre- and 3 months post-treatment showed reduction in Df value from 1.850 to 1.831; and reduction in area of vascularization of 38 ± 1 to 32 ± 2 % (P = 0.003).
Discussion
In this preliminary report of a small case series of eyes with corneal vascularization, we present promising results that support the potential use of a novel OCTA imaging technique for monitoring changes in corneal vascular areas, comparing pre- and post-treatment imaging after a variety of interventions. All the cases of previous herpetic keratitis illustrated here had varying degrees of corneal vascularization and a variety of treatments such as fine-needle diathermy [12], anti-VEGF for corneal neovascularization [7], and monitoring of corneal graft related rejection or inflammation [10]. Previous studies have described the use of invasive angiography techniques such as FA, where leakage may be used as a measure of vessel maturity [13]. ICG stays within normal capillaries, and; hence, leakage may indicate loss of vessel integrity secondary to pathologic inflammatory or vascular damage [14]. Therefore, the novel OCTA imaging system described in this study, although mainly used in research currently, may emerge as a potential rapid, non-invasive alternative to objectively monitor treatment response in eyes with corneal vascularization – which requires larger studies to confirm.
The clinical applications of angiography in the anterior segment have been well described. In 1985, Watson and Bovey [15] first described the use of FA in scleral inflammation to differentiate benign non-destructive and necrotising forms of anterior scleritis, illustrating how decreased flow, leakage and permanent occlusive features of capillaries in progressive scleritis, could result in peripheral corneal destruction. ICG angiography (ICGA) has also been used to demonstrate successful reconstruction of the marginal corneal vascular arcades with increased vessel density and lacunarity following limbal-conjunctival autograft ransplantation after pterygium excision [16]. These studies highlight the potential for research in scleral and corneal diseases, including ocular surface diseases and limbal stem cell deficiency, where use of vascular imaging such as OCTA may provide useful information for the diagnosis and monitoring of treatment.
The advantages of this rapid, non-invasive OCTA for the anterior segment compared to the current FA and ICGA techniques have been previously discussed [17]. Our study, to the best of our knowledge, is the first to describe the analysis of OCTA imaging in corneal vascularization pre- and post- treatment. However, the use of objective parameters to measure changes in vascular areas over time could be an improvement over current subjective scoring of corneal vascularization. While promising, further improvements are required as the currently available OCTA systems are optimized for the retina rather than the anterior segment [18]. For example, we observed that the lack of a fixation target or eye tracking system led to multiple motion artefacts, which were compensated by taking four scans in each with good signal strength. Moreover, we noted that imaging the superior quadrants of the corneal limbus was more difficult due to the lashes, on occasion the upper eyelid required assistance to be retracted by the operator to avoid optical shadows cast by the eyelashes in the scans. Image analysis could improve with time as well, such as semi-automated methods to quantify corneal vascularization in vivo [6], and with digital images using threshold analyses and filters [19]. Although semi-automated techniques are useful [20, 21], limitations with current software [10] means that many researchers still rely on manually calculating parameters such as the total vascular area as a proportion of the total cornea and mean diameter of vessels [7].
Therefore, many studies, including this study, still rely on subjective scores for corneal vascularization and grading [22]. We also recognize the limitations of this early case series in a small number of eyes to describe a novel OCTA technique for the cornea. In spite of this, we managed to demonstrate the ability of the OCTA in detecting significant change in vessel parameters corresponding to the gross changes seen on colour photograph as shown.
Moreover, as improvements to OCT image enhancement [23], and processing are introduced [24–27], better scan quality may be achieved, such as the use of filtering techniques used here to remove most of the larger microsaccadic artefacts. A larger study on OCTA and the sensitivities and specificities in detecting corneal vascularization, with comparison to other imaging modalitites such as slit-lamp photography or ICGA, may be useful to ascertain its practicality for use as an investigative modality for the future. Nonetheless, this study could highlight many potential future developments, including improvements to the inbuilt OCTA software to allow for serial comparisons in the same eye over time. Furthermore, the OCTA may be developed for other clinical indications, such as assessing epsicleral venous flow in open angle glaucoma secondary to carotid-cavernous fistulas or dilated episcleral veins, or rubeosis iridis and other vascular complications of the anterior segment in ischaemic diseases [28].
In conclusion, our observations from this early clinical study have highlighted the potential of a novel OCTA imaging technique in evaluating changes in corneal vascularization in response to various treatments.
References
Spaide RF, Klancnik JM, Cooney MJ (2015) Retinal vascular layers imaged by fluorescein angiography and optical coherence tomography angiography. JAMA Ophthalmol 133:45–50. doi:10.1001/jamaophthalmol.2014.3616
Qazi Y, Maddula S, Ambati BK (2009) Mediators of ocular angiogenesis. J Genet 88:495–515
Lee P, Wang CC, Adamis AP (1998) Ocular neovascularization: an epidemiologic review. Surv Ophthalmol 43:245–269
Ang M, Mehta JS, Sng CC, Htoon HM, Tan DT (2012) Indications, outcomes, and risk factors for failure in tectonic keratoplasty. Ophthalmology 119:1311–1319. doi:10.1016/j.ophtha.2012.01.021
Cursiefen C, Colin J, Dana R, Diaz-Llopis M, Faraj LA, Garcia-Delpech S, Geerling G, Price FW, Remeijer L, Rouse BT, Seitz B, Udaondo P, Meller D, Dua H (2012) Consensus statement on indications for anti-angiogenic therapy in the management of corneal diseases associated with neovascularisation: outcome of an expert roundtable. Br J Ophthalmol 96:3–9. doi:10.1136/bjo.2011.204701
Ang M, Cai Y, MacPhee B, Sim DA, Keane PA, Sng CC, Egan CA, Tufail A, Larkin DF, Wilkins MR (2016) Optical coherence tomography angiography and indocyanine green angiography for corneal vascularisation. Br J Ophthalmol. doi:10.1136/bjophthalmol-2015-307706
Ang M, Sim DA, Keane PA, Sng CC, Egan CA, Tufail A, Wilkins MR (2015) Optical coherence tomography angiography for anterior segment vasculature imaging. Ophthalmology 122:1740–1747. doi:10.1016/j.ophtha.2015.05.017
Hsu CC, Chang HM, Lin TC, Hung KH, Chien KH, Chen SY, Chen SN, Chen YT (2015) Corneal neovascularization and contemporary antiangiogenic therapeutics. J Chin Med Assoc 78:323–330. doi:10.1016/j.jcma.2014.10.002
Gonzalez L, Loza RJ, Han KY, Sunoqrot S, Cunningham C, Purta P, Drake J, Jain S, Hong S, Chang JH (2013) Nanotechnology in corneal neovascularization therapy—a review. J Ocul Pharmacol Ther 29:124–134. doi:10.1089/jop.2012.0158
Ang M, Cai Y, Shahipasand S, Sim DA, Keane PA, Sng CC, Egan CA, Tufail A, Wilkins MR (2015) En face optical coherence tomography angiography for corneal neovascularisation. Br J Ophthalmol. doi:10.1136/bjophthalmol-2015-307338
Sharma A, Bettis DI, Cowden JW, Mohan RR (2010) Localization of angiotensin converting enzyme in rabbit cornea and its role in controlling corneal angiogenesis in vivo. Mol Vis 16:720–728
Zheng Y, Kaye AE, Boker A, Stewart RK, Tey A, Ahmad S, Willoughby CE, Bron AJ, Kaye SB (2013) Marginal corneal vascular arcades. Invest Ophthalmol Vis Sci 54:7470–7477. doi:10.1167/iovs.13-12614
Spiteri N, Romano V, Zheng Y, Yadav S, Dwivedi R, Chen J, Ahmad S, Willoughby CE, Kaye SB (2015) Corneal angiography for guiding and evaluating fine-needle diathermy treatment of corneal neovascularization. Ophthalmology 122:1079–1084. doi:10.1016/j.ophtha.2015.02.012
Petsoglou C, Balaggan KS, Dart JK, Bunce C, Xing W, Ali RR, Tuft SJ (2013) Subconjunctival bevacizumab induces regression of corneal neovascularisation: a pilot randomised placebo-controlled double-masked trial. Br J Ophthalmol 97:28–32. doi:10.1136/bjophthalmol-2012-302137
Papathanassiou M, Theodoropoulou S, Analitis A, Tzonou A, Theodossiadis PG (2013) Vascular endothelial growth factor inhibitors for treatment of corneal neovascularization: a meta-analysis. Cornea 32:435–444. doi:10.1097/ICO.0b013e3182542613
Ang M, Mehta JS, Arundhati A, Tan DT (2009) Anterior lamellar keratoplasty over penetrating keratoplasty for optical, therapeutic, and tectonic indications: a case series. Am J Ophthalmol 147(697–702):e692. doi:10.1016/j.ajo.2008.10.002
Kirwan RP, Zheng Y, Tey A, Anijeet D, Sueke H, Kaye SB (2012) Quantifying changes in corneal neovascularization using fluorescein and indocyanine green angiography. Am J Ophthalmol 154:850–858.e852. doi:10.1016/j.ajo.2012.04.021
Nieuwenhuizen J, Watson PG, Emmanouilidis-van der Spek K, Keunen JE, Jager MJ (2003) The value of combining anterior segment fluorescein angiography with indocyanine green angiography in scleral inflammation. Ophthalmology 110:1653–1666. doi:10.1016/S0161-6420(03)00487-1
Watson PG, Bovey E (1985) Anterior segment fluorescein angiography in the diagnosis of scleral inflammation. Ophthalmology 92:1–11
Chan CM, Chew PT, Alsagoff Z, Wong JS, Tan DT (2001) Vascular patterns in pterygium and conjunctival autografting: a pilot study using indocyanine green anterior segment angiography. Br J Ophthalmol 85:350–353
Kim YJ, Yoo SH, Chung JK (2014) Reconstruction of the limbal vasculature after limbal-conjunctival autograft transplantation in pterygium surgery: an angiography study. Invest Ophthalmol Vis Sci 55:7925–7933. doi:10.1167/iovs.14-15288
Conrad TJ, Chandler DB, Corless JM, Klintworth GK (1994) In vivo measurement of corneal angiogenesis with video data acquisition and computerized image analysis. Lab Invest 70:426–434
Girard MJ, Ang M, Chung CW, Farook M, Strouthidis N, Mehta JS, Mari JM (2015) Enhancement of corneal visibility in optical coherence tomography images using corneal adaptive compensation. Transl Vis Sci Technol 4:3. doi:10.1167/tvst.4.3.3
Bock F, Onderka J, Hos D, Horn F, Martus P, Cursiefen C (2008) Improved semiautomatic method for morphometry of angiogenesis and lymphangiogenesis in corneal flatmounts. Exp Eye Res 87:462–470. doi:10.1016/j.exer.2008.08.007
Bock F, Konig Y, Kruse F, Baier M, Cursiefen C (2008) Bevacizumab (Avastin) eye drops inhibit corneal neovascularization. Graefes Arch Clin Exp Ophthalmol 246:281–284. doi:10.1007/s00417-007-0684-4
Cursiefen C, Bock F, Horn FK, Kruse FE, Seitz B, Borderie V, Früh B, Thiel MA, Wilhelm F, Geudelin B, Descohand I, Steuhl KP, Hahn A, Meller D (2009) GS-101 antisense oligonucleotide eye drops inhibit corneal neovascularization: interim results of a randomized phase II trial. Ophthalmology 116:1630–1637. doi:10.1016/j.ophtha.2009.04.016
Ang M, Chong W, Huang H, Tay WT, Wong TY, He MG, Aung T, Mehta JS (2013) Comparison of anterior segment optical tomography parameters measured using a semi-automatic software to standard clinical instruments. PLoS One 8:e65559. doi:10.1371/journal.pone.0065559
Ang M, Sng C, Milea D (2016) Optical coherence tomography angiography in dural carotid-cavernous sinus fistula. BMC Ophthalmol 16:93. doi:10.1186/s12886-016-0278-1
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Singhealth Research Foundation (R1275/81/2015)
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Cai, Y., Alio del Barrio, J.L., Wilkins, M.R. et al. Serial optical coherence tomography angiography for corneal vascularization. Graefes Arch Clin Exp Ophthalmol 255, 135–139 (2017). https://doi.org/10.1007/s00417-016-3505-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-016-3505-9