Abstract
Purpose
To describe the morphological macular changes detected by spectral domain optical coherence tomography (SD-OCT) in eyes with retinitis pigmentosa (RP) and to analyze their correlation with the visual function.
Methods
Twenty-two patients (44 eyes) patients affected by RP were recruited. The following structures were evaluated on SD-OCT: outer plexiform layer (OPL), outer nuclear layer (ONL), external limiting membrane (ELM), photoreceptor inner/outer segment (IS/OS) junction, photoreceptor outer segment/retinal pigmented epithelium (OS/RPE) junction, inner limiting membrane thickening (ILMT), ganglion cell complex (GCC), and cystoid macular edema (CME). The relation between each SD-OCT finding and BCVA was evaluated at uni- and multivariate analysis.
Results
Mean age and mean best-corrected visual acuity (BCVA) were 51 ± 17.5 years and 0.4 ± 0.5 LogMAR, respectively. Univariate linear regression model revealed a correlation between BCVA and the absence of ELM, IS/OS, ONL, and OS/RPE layers (R 2 values were, respectively, 0.51, 0.57, 0.48, and 0.68, with p values all <0.0001). At multivariate regression analysis, the absence of OS/RPE and ELM layers remained the only variables independently associated with a decrease of BCVA (R 2 = 0.85, t = 3.49, p = 0.0014).
Conclusions
Data show that in patients afflicted with RP, ELM and OS/RPE layers are independently associated with BCVA on multivariate regression analysis. These results highlight the key-role of external retinal layers in determining the visual function impairment attributable to RP.
Similar content being viewed by others

Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Retinitis pigmentosa (RP) is a heterogeneous group of diseases characterized by progressive degeneration of rod and cone cells. The clinical features of typical RP include “bone-spicule” retinal pigment, thinning and atrophy of the retinal pigment epithelium (RPE), “waxy pallor” of the optic nerve head, and attenuation of retinal arteries. The visual impairment involves night vision and peripheral vision, with gradual deterioration of the central visual acuity [1–3]. Optical coherence tomography (OCT) can considerably contribute to the clinical assessment of patients affected by RP. In particular, previous studies have indicated that RP is characterized by alterations of the photoreceptor inner/outer segment (IS/OS) junction, and the external limiting membrane (ELM) [4–10]. In particular, previous studies have shown that foveal outer segment/pigment epithelium (OS/RPE) thickness and integrity of IS/OS junction are correlated with the BCVA in eyes with RP [4, 5, 7]. Nevertheless, although many OCT alterations have been described in RP, no specific analysis has focused on the role of any specific OCT layer to the visual outcome. The aim of the present study is to describe correlations between foveal OCT findings and visual acuity.
Methods
A consecutive series of patients affected by RP were prospectively recruited at the Department of Ophthalmology of Vita-Salute University Hospital. Written informed consent was obtained from all subjects. The protocol was approved by the local IRB, and the procedures adhered to the tenets of the Declaration of Helsinki. All patients underwent a complete ophthalmic examination, including best-corrected visual acuity (BCVA) on ETDRS charts, biomicroscopy, applanation tonometry, biomicroscopic examination, spectral-domain OCT (SD-OCT), and microperimetry.
Inclusion criteria included a diagnosis of RP and clear media to allow adequate OCT examination. Patients were excluded if they had significant cataracts or other media opacities, and/or if they had other ocular diseases that could affect the results.
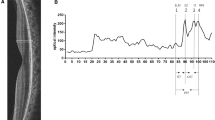
SD-OCT was carried out using the Spectralis HRA (Heidelberg Engineering, Heidelberg, Germany) by means of a horizontal line scan, centered on the fovea. In particular, the following structures were analyzed: outer plexiform layer (OPL), outer nuclear layer (ONL), external limiting membrane (ELM), photoreceptor inner/outer segment (IS/OS) junction, photoreceptor outer segment/retinal pigmented epithelium (OS/RPE) junction, inner limiting membrane thickening (ILMT), ganglion cell complex (GCC), and cystoid macular edema (CME) (Fig. 1). Best-corrected visual acuity (BCVA) was registered using standard ETDRS charts. Two examiners, masked to the purpose of the investigation, independently judged SD-OCT and graded each layer into three grades (grade 0: absent; grade 1: disrupted; grade 2: normal). BCVA was measured by another examiner in masked fashion.
a SD-OCT scan centered on the fovea of a patient affected by RP. The retinal structures and layers considered in the analysis are showed: inner limiting membrane (ILM), ganglion cell complex (GCC), outer plexiform layer (OPL), outer nuclear layer (ONL), external limiting membrane (ELM), photoreceptor inner/outer segment (IS/OS) junction, photoreceptor outer segment/retinal pigmented epithelium (OS/RPE) junction. In this specific case, the ONL looks thinned and disrupted, as well as the IS/OS and OS/RPE junctions. b SD-OCT scan centered on the fovea of a patient diagnosed with RP complicated by cystoid macular edema (CME). All the main retinal structures described above remain detectable, despite the presence of intra-retinal cysts
Primary outcome of the study is the identification of a correlation between SD-OCT findings and BCVA. Secondary outcome includes the evaluation of the frequency of each of the SD-OCT findings.
We tested the differences between groups using the non-parametric Mann–Whitney U test or Kruskal–Wallis test, as appropriate. Univariate and multivariate linear regression models were also performed to show the effect of all variables on BCVA. All tests were two-sided and a p value less than 0.05 was considered significant. All analyses were performed using SAS V 9.3 (SAS software, SAS Institute Inc. Cary, NC, USA).
Results
Overall, 22 patients (44 eyes) fulfilling the inclusion and exclusion criteria were recruited for the study. Mean age of the patients was 51 ± 17.5 years. Ten patients (45 %) were females. Mean BCVA was 0.4 ± 0.5 LogMAR (approximately corresponding to 20/50 Snellen equivalent) at baseline. A mild or moderate ILM thickening was detected in 33 eyes (75 %), while nine eyes (20 %) presented with a macular pucker. Mean choroid thickness was 248 ± 71 μm. CME was detected in seven eyes (16 %). Baseline characteristics of the SD-OCT layers considered are listed in Table 1.
The correlation between BCVA and all OCT findings was at first separately investigated by means of univariate analysis. A preserved OPL layer was associated with a better BVCA: mean BCVA for patients presenting with normal, disrupted and absent OPL were, respectively, 0.2, 0.6, and 1.1 (p = 0.0035). Moreover, a preserved ONL layer was coupled with a better BVCA: mean BCVA for patients presenting with normal, disrupted, and absent ONL were, respectively, 0.1, 0.6, and 1.5 (p = 0.0001). ELM layer integrity was also related to a better BVCA: mean BCVA for patients presenting with normal, disrupted, and absent ELM were, respectively, 0.1, 0.4, and 0.9 (p < 0.0001). A preserved IS/OS layer turned out to be associated with a better BVCA: mean BCVA for patients presenting with normal, disrupted, and absent IS/OS were, respectively, 0.1, 0.5, and 1.4 (p < 0.0001). OS/RPE layer was linked to a better BVCA: mean BCVA for patients presenting with normal, disrupted, and absent OS/RPE were, respectively, 0.1, 0.4, and 1.4 (p < 0.0001). No differences were found regarding the presence or absence of CME, the ILM thickening, and the choroidal thickness. GCC layer thickness was 14.2 ± 15, and no correlation was found between BCVA and GCC layer thickness.
Subsequently, the univariate linear regression model highlighted the correlation between poor BCVA and the absence of ELM, IS/OS, ONL, and OS/RPE layers (R 2 values were, respectively, 0.51, 0.57, 0.48, and 0.68, with p values all <0.0001) (Table 2).
Lastly, confounding factors were controlled by the multivariate regression analysis. The absence of OS/RPE and ELM layers remained the only variables independently associated with a decrease of BCVA (R 2 = 0.85, t = 3.49, p = 0.0014) (Table 2).
Discussion
The early histopathological alterations typical of RP are represented by shortening of the photoreceptor outer segments [1, 2], with consequent gradual degeneration of the cones and central vision impairment [1–3]. SD-OCT can greatly contribute to the morphological assessment, disclosing many changes of the retinal layers, including also inner limiting membrane thickening ILMT, and CME [4–11]. However, no study has specifically investigated the relationship between each OCT layer change and BCVA. The purpose of this study was to evaluate, with univariate and multivariate analyses, the effects of altered SD-OCT findings on the residual visual acuity in patients affected by RP.
With univariate analysis, both absence and disruption of OPL, ONL, ELM, IS/OS, and OS/RPE layers turned out to be significantly associated with a BCVA decline. However, when analyzing the data with a linear regression model, just the absence of ELM, IS/OS, ONL, and OS/RPE layers was linked to BCVA changes. After multivariate regression analysis, only the absence of ELM and OS/RPE remained independently associated with a BCVA impairment.
Previous investigations provided interesting results regarding the correlation of OCT findings and visual function. In particular, Sandberg et al. reported that the decline in visual acuity for decreasing retinal thickness was steeper in eyes with an absent third high-reflectance band [4]. Matsuo et al. found that the identification of more external retinal layers correlated with a greater BCVA [5]. Aizawa et al. reported that the integrity and the length of the IS/OS was significantly correlated with the BCVA [6]. Mitamura and colleagues reported a significant relationship between IS/OS length and BCVA [7]. The length of the IS/OS layer has also been linked with a better contrast sensitivity and a better color vision in the paper by Yioti et al. [8]. However, it is important to note that all of the previous studies performed just a univariate analysis, which only offers an incomplete appraisal.
Indeed, our data confirm the influence of the ELM on BCVA worsening. On the other hand, the IS/OS junction does not seem to be independently linked to BVCA. In fact, the multivariate model revealed that the OS/RPE layer is only independently associated with BCVA. The IS/OS layer association detected on univariate analysis can be considered as a confounding factor, which is probably due to the linear association between IS/OS and OS/RPE layers. Thus, multivariate regression analysis indicates that both ELM and OS/RPE are related to visual acuity changes.
Our results confirm the data previously published by Witkin and colleagues who reported a reduced OS/RPE thickness in RP patients and a positive correlation between this measurement and BCVA [9]. Moreover, the role of a preserved outer photoreceptor segment in RP patients with good BCVA has been recently highlighted also by Ki Yoon and colleagues [10]. Such a strong association between the absence of OS/RPE and a worse BCVA reflects the functional importance of the RPE and its junction with the photoreceptor layer. This importance is also highlighted by the study of Robson et al., where patients with a preserved hyper-autofluorescence macular ring (reflecting preserved outer retinal layers) showed a better visual outcome [12].
In conclusion, this study, designed to evaluate the functional importance of the retinal layer changes in RP patients, revealed that ELM and OS/EPR are independently associated with BCVA outcomes on multivariate regression analysis.
References
Berson EL (1993) Retinitis pigmentosa. The Friedenwald Lecture. Invest Ophthalmol Vis Sci 34:1659–1676
Milam AH, Li ZY, Fariss RN (1998) Histology of the human retina in retinitis pigmentosa. Prog Retin Eye Res 17:175–205
Hartong DT, Berson EL, Dryja TP (2006) Retinitis pigmentosa. Lancet 368:1795–1809
Sandberg MA, Brockhurst RJ, Gaudio AR, Berson EL (2005) The association between visual acuity and central retinal thickness in retinitis pigmentosa. Invest Ophthalmol Vis Sci 46:3349–3354
Matsuo T, Morimoto N (2007) Visual acuity and perimacular retinal layers detected by optical coherence tomography in patients with retinitis pigmentosa. Br J Ophthalmol 91:888–890
Aizawa S, Mitamura Y, Baba T, Hagiwara A, Ogata K, Yamamoto S (2008) Correlation between visual function and photoreceptor inner/outer segment junction in patients with retinitis pigmentosa. Eye 23:304–308
Mitamura Y, Aizawa S, Baba T, Hagiwara A, Yamamoto S (2009) Correlation between retinal sensitivity and photoreceptor inner/outer segment junction in patients with retinitis pigmentosa. Br J Ophthalmol 93:125–126
Yioti GG, Kalogeropoulos CD, Aspiotis MB, Stefaniotou MI (2012) Contrast sensitivity and color vision in eyes with retinitis pigmentosa and good visual acuity: correlations with SD-OCT findings. Ophthalmic Surg Lasers Imaging 43(6 Suppl):S44–S53
Witkin AJ, Ko TH, Fujimoto JG, Chan A, Drexler W, Schuman JS et al (2006) Ultra-high resolution optical coherence tomography assessment of photoreceptors in retinitis pigmentosa and related diseases. Am J Ophthalmol 142:945–952
Yoon CK, Yu HG (2013) The structure-function relationship between macular morphology and visual function analyzed by optical coherence tomography in retinitis pigmentosa. J Ophthalmol 2013:821460
Triolo G, Pierro L, Parodi MB, De Benedetto U, Gagliardi M, Manitto MP, Bandello F (2013) Spectral domain optical coherence tomography findings in patients with retinitis pigmentosa. Ophthalmic Res 50:160–164
Robson AG, Tufail A, Fitzke F, Bird AC, Moore AT, Holder GE, Webster AR (2011) Serial imaging and structure-function correlates of high-density ring of fundus autofluorescence in retinitis pigmentosa. Retina 31(8):1670–1679
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Financial disclosures
Dr. Bandello F:
Advisory Board Member: ALLERGAN, INC.; NOVARTIS PHARMACEUTICALS CORPORATION; FARMILA-THEA; BAYER SCHERING PHARMA; PFIZER, INC.; ALCON, INC.; BAUSCH AND LOMB; GENENTECH, INC.; ALIMERA SCIENCES, INC; THROMBOGENICS, INC.
Ethical approval
For this type of study formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Battaglia Parodi, M., La Spina, C., Triolo, G. et al. Correlation of SD-OCT findings and visual function in patients with retinitis pigmentosa. Graefes Arch Clin Exp Ophthalmol 254, 1275–1279 (2016). https://doi.org/10.1007/s00417-015-3185-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-015-3185-x