Abstract
Purpose
To examine the clinical differences in manifestation, course, treatment, and prognosis of thyroid eye disease (TED) in patients younger than 40 years of age at diagnosis compared to older patients.
Methods
Medical record review of 131 TED patients was performed. The patients were divided into two age groups, Group 1 ≤ 40 years (23 patients) and Group 2 > 40 years (108 patients).
Results
Younger patients had more eyelid retraction and proptosis at initial presentation, whereas older patients were more likely to have diplopia (P = 0.001). Acute inflammatory signs were more common in the Group 2 patients (P = 0.04). Corrected visual acuity was 20/20 and 20/25 in both groups. Optic neuropathy was diagnosed only in Group 2 patients (n = 12; 11 %), and it resolved after steroids or orbital decompression surgery in all cases. The mean follow-up time was 36 months (36 ± 7.7; 59.3 ± 5.8). Systemic steroid use, orbital surgery, and strabismus surgery were more common in Group 2 (P < 0.0001, P < 0.05 respectively).
Conclusions
TED under the age of 40 years has different clinical features. In our group of younger patients, the clinical presentation was milder than in the older group with a higher rate of lid retraction and proptosis and lower rate of restrictive myopathy and optic neuropathy. Their disease course was less severe and required less aggressive medical treatment and less surgical procedures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Thyroid eye disease (TED) is the most frequent extra-thyroidal manifestation of Graves’ disease with an age-adjusted annual incidence of 16 per 100,000 in women and 2.9 per 100,000 in men and with an estimated prevalence of 0.25 % [1]. It is a progressive eye disorder characterized by immune-mediated inflammation of the extraocular muscles and orbital connective tissue [2–6]. The incidence rate of TED shows an apparent bimodal peak in men and women. However, both peaks occur on average 5 years earlier in women than in men (40–44 years old vs. 45–49 years old and 60–64 years old vs. 65–69 years old) [1].
TED patients show various degrees of severity of clinical manifestations of disease. Different factors for this variation were examined in the past including age [7–9, 8], gender [10–12], smoking [11, 13, 14], and family history [15]. The purpose of the current study is to examine clinical features, treatment modalities, and prognosis of an incidental cohort of TED patients in patients younger than 40 years of age at diagnosis compared to older patients.
Forty years old was defined as the age cut-off because few studies in the past reported that patients who are younger than 40 years old at diagnosis had a more severe Graves’ disease than patients who were diagnosed later. However, they found that thyroid ophthalmopathy is more severe in patients who are older than 40 years old [15, 16].
Nunery et al. separated the histopathological changes in TED to two subtypes: Type 1 was defined as a retrobulbar fat and connective tissue stimulation with increased fibroblastic activity; type 2 was defined as extraocular myositis with edema, lymphocytic infiltration and muscle necrosis. Patients with type 1 disease have proptosis, but a good or normal extraocular motility and rarely have neuropathy and diplopia, while type 2 patients have a greater risk of compressive neuropathy, diplopia, and acute orbital inflammation [17].
This study also examines if there is correlation between Nunery’s histopathological subtypes and epidemiological, clinical, treatment, and prognosis.
Patients and methods
A retrospective medical record review of all TED patients treated at the Goldschleger Eye Institute and the Department of Ophthalmology of Kaplan Medical Center from January 1997 to December 2005 was performed. Information regarding thyroid dysfunction and general medical status was recorded. History of symptoms was collected. Data regarding demographics, thyroid and general medical status, presenting signs and symptoms, visual acuity, visual field findings, comprehensive ophthalmic, and orbital examinations were collected.
Each participant performed visual field test (Humphrey 24–2). Intraocular pressure (IOP) was measured by Goldman tonometer.
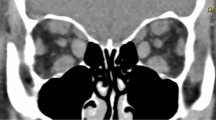
Review of computerized tomographic (CT) scans of the orbits data regarding medical treatment, prisms recommended, and surgeries performed were recorded and analyzed.
Proptosis was defined as a protrusion of the globe greater than 17 mm or a difference of more than 2 mm between eyes as measured by Hertel exophthalmometer.
Lid lag was defined as the slowed descent of the eyelid during movement of the globe from primary position to down gaze.
The patients were divided into two groups according to whether they were ≤40 years of age (Group 1) or >40 years of age (Group 2).
The study was approved by the local institutional review board (IRB) of the two medical centers.
Statistical analysis
Statistical analysis was performed using a paired samples t-test to compare pre- and postoperative data. Independent samples t-test was used to calculate difference in parametric variables between the two groups. Cross tabs and chi-square analysis were used to calculate proportional difference between the two groups. For group less than 30 patients, data were analyzed using non-parametric analysis tests. The overall significance level was set to an alpha of 0.05. Snellen VA was converted to logMAR value. Statistical analysis was carried out using Microsoft Excel 2003 (Microsoft Corporation, Redmond, WA, USA) and SPSS software version 13.0 (SPSS, Inc., Chicago, IL, USA).
Results
Demographics
A total of 131 TED patients participated in the study. Group 1 consisted of 23 (15 females) patients aged ≤40 years (mean ± SD 29 ± 9 years, range 8–40), and Group 2 of 108 patients (76 females) >40 years of age (mean ± SD 56 ± 11 years, range 41–94). Demographics of the study population are summarized in Table 1. One patient was 8 years old, two patients were 16 years old, and two patients were 20 years old in Group 1. The range of the other 18 patients of Group 1 was 20–40 years. The peak ages were 32 and 40 years in Group 1 and 48 and 51 years in Group 2 (Fig. 1a and b).
Thyroid and general medical status
The thyroid status in most patients was hyperthyroidism at the initial presentation (85 % in Group 1 and 82 % in Group 2). At the time of referral to the eye center only 40 % of the Group 1 and 40 % of the Group 2 patients were hyperthyroid, whereas 45 % and 38 % were hypothyroid and 15 % and 22 % were euthyroid, respectively. Two patients in Group 1 had concomitant autoimmune diseases (9 %) compared to none in Group 2. Hypertension and ischemic heart disease were more common in Group 2 (three patients, 12 %) compared to Group 1 (none). Smoking was equally prevalent in both groups (10 %). Thyroid dysfunction treatments were similar in both groups and consisted of propylthiouracil (PTU) or mercaptizole (9/23, 39 % and 38/108, 35 %), radioactive iodine (RAI) (8/23, 35 % and 36/108, 33 %), surgery (1/23, 4 % and 9/108, 8 %), Eltroxin (1/23, 4 % and 3/108, 3 %), and steroids (0/23,0 % and 3/108, 3 %). These differences did not reach a level of significance (chi-square analysis).
Past ocular history was not significant in most of cases in both groups. Most patients with previous ocular disease belonged to Group 2 (cataract 2, glaucoma 5) and only one patient in Group 1 with corneal opacity.
Presenting signs and symptoms
Group 1 patients complained of eye bulging (65 %) and eyelid retraction (17 %) as the initial sign more frequently than the Group 2 patients who were more bothered by diplopia (54 %) followed by proptosis (41 %). Seventeen percent of Group 1 and 5 % of Group 2 patients had eyelid retraction as the presenting symptom. However, as presenting sign, retraction was seen in 15 (74 %) of Group 1 patients and in 28 (26 %) of Group 2 patients (Fig. 2, Table 1). These differences were highly significant (P = 0.001, chi-square test). Acute inflammatory signs, such as eyelid edema, chemosis, and punctate keratopathy, were significantly more common among the Group 2 patients (P = 0.04, chi-square test) (Table 1). The rate of bilateral disease was the same in both groups (5/23 and 23/108 or 21 % for each).
Intraocular pressure and exophthalmometry
The average IOP was within normal limits in primary and in up-gaze (Table 2). A significant rise in IOP in up-gaze was more common in both eyes of Group 2 patients: it rose from 17 and 18 mmHg primary gaze to 24 and 23 mmHg in up-gaze. These differences were less apparent after treatment and at last follow-up. Topical glaucoma medications were prescribed to 11 patients in Group 2 with IOP elevation in primary position and none in Group 1.
Average exophthalmometry measurements were 21.5 and 22.5 mm in Groups 1 and 2 at the initial visit and 19.8 and 20.8 mm after treatment at the last visit, respectively (Table 2).
Visual acuity and visual field findings
Most patients had mild-to-moderate disease, and so the presenting and final corrected VAs were excellent in both groups (Table 2): 20/20 in both eyes at the first and last visit for Group 1 and 20/25 in both eyes at the first visit and 20/25 right eye (OD) and 20/40 left eye (OS) at last follow-up for Group 2. Visual field defects in one or both eyes were relatively more common in the Group 2 patients: nine eyes showed quadrant defects (six of which involved two quadrants), and eight eyes had concentric narrowing of the visual field. One in Group 1 had a single quadrant defect and one eye had a two-quadrant defect (P = not significant, chi-square test). None of the younger patients had dysthyroid optic neuropathy (DON).
DON
Although optic neuropathy (unilateral or bilateral) was found only in Group 2 patients (12/108, 11 % vs. 0/23, 0 %) this difference was not significant (P = 0.09, chi-square test). The right eye was more commonly involved (8/12 patients, 67 %), and one patient had bilateral optic neuropathy (1/12, 8.3 %). VA improved from 20/30 at presentation to 20/20 after treatment (P = not significant, Wilcoxon signed rank test). Exophthalmometry assessments using Hertel measurements showed an average 3-mm decrease, from 23 mm to 20 mm post-treatment (P = 0.04). The MD visual field improved from −7.0 dB to −1.6 dB (P = 0.018). Visual field defects in the DON patients were quadrant defect (50 %), concentric (33 %), and two quadrants (16 %). DON was not associated with older age or systemic cardiovascular diseases in Group 2. DON in the Group 2 patients was more common in males (7/12, 58 %, P = 0.02), diplopia on initial presentation (11/12, 92 %, P = 0.049), and with fusiform enlargement of all extraocular muscles on CT scan (5/12, 42 %, P = 0.06). Only one patient with DON had glaucoma. DON patients had more severe restriction in up-gaze as reflected by IOP increase in up-gaze: IOP increased on average from 20 mmHg in primary gaze to 34 mmHg in up-gaze. IOP in patients without neuropathy increased from 18 mmHg to 22 mmHg (P = 0.0001, chi-square test). Treatment efficacy as measured by improvement in VA, color vision, and visual field was achieved in patients with DON. Specifically, 11/12 (92 %) of all DON patients in Group 2 showed improvement in all three parameters after anti-inflammatory treatment or orbital decompression surgery (Table 3).
Imaging
All patients underwent CT scans to establish the diagnosis of TED and to evaluate the orbital apex in the 12 patients with DON. They also served to plan orbital decompression surgery according to bony anatomy of the orbit and paranasal sinuses. CT abnormal findings were significantly more prevalent in the Group 2 patients (Table 4). The most common finding was inferior rectus enlargement, followed by medial rectus muscle enlargement and superior rectus muscle enlargement. All four recti muscles involvement with fusiform enlargement was more common in the Group 2 patients with DON. Nine of the 96 patients without neuropathy (9.4 %) showed muscle enlargement in the four recti muscles, and five out of the 12 patients with DON (42 %) had similar findings (P = 0.002, chi-square test).
Type 1 and type 2 histopathological subtypes
Type 1 consisted of 118 patients and type 2 consisted of 13 patients. The mean age at diagnosis of type 1 was 51.86 years old (mean ± SD 51.86 ± 14.11 years) and of type 2 was 51.00 years old (mean ± SD 51.00 ± 20.16 years).
Among type 2 patients, no acute inflammatory signs were more common than among type 1 patients (18.80 % vs. 30. 76 %, respectively). Eyelid edema was more common among type 1 patients than among type 2 patients (43.58 % vs. 15. 38 %). These differences were statistically significant (P = 0.0.41, chi-square test).
Of type 1 patients, 35.59 % underwent surgery (lid surgery, strabismus operation or decompression surgery), while none of the type 2 patients had surgery (P = 0.0.009, chi-square test).
Parameters regarding demographics, thyroid and general medical status, IOP and exophthalmometry, visual acuity and visual field findings, DON, imaging, and other treatment except for surgery and outcome were not statistically different.
Treatment of TED and outcome
Fourteen (61 %) patients in Group 1 and 59 (55 %) patients in Group 2 received supportive measures consisting of observation or topical eye lubricants. Anti-inflammatory treatment, such as systemic steroids, somatostatin analogues, IVIG (Intravenous immunoglobulin), or orbital irradiation, was more common in the Group 2 patients (P < 0.0001, chi-square). Similarly, Group 2 patients more commonly underwent surgical procedures such as orbital decompression (19 vs. 1 in Group 1) or strabismus (14 vs. 0 in Group 1) surgeries (P < 0.05). Eyelid repositioning surgery was performed similarly in both groups (5 for Group 1 vs. 20 for Group 2, 20 %). Treatment modalities are summarized in Table 5 and Fig. 3. At the end of follow-up, anti-glaucoma medications were prescribed to one Group 1 patient (4 %) and 11 Group 2 patients (10 %). These percentages did not change significantly at the last follow-up.
Optic neuropathy improved in all Group 2 patients. The VA, IOP, and exophthalmometry measurements did not change from initial visit to last follow-up in any of the patients (Table 3). DON patients had significant improvement in the following parameters after treatment: globe retro-positioning of 3 mm, IOP decrease of 6 mmHg, mean deviation visual field of 5.5 dB (P values of 0.01, 0.004, and 0.01, respectively, one sample t test of the difference).
Treatment efficacy was monitored and recorded in all patients according to no change (signs and symptoms), improvement or worsening. Twelve Group 1 patients (52 %) had no change under treatment, four (17 %) improved, and none (0 %) had worsening of the thyroid orbitopathy. Forty-two Group 2 patients (39 %) had no change, 39 (36 %) improved and seven (6.5 %) had worsening of the thyroid orbitopathy (P = 0.02, between the two groups, chi square test).
Mean follow-up time was 29 months in Group 1 and 45 months in Group 2 (P = 0.2, NS).
Discussion
Our findings suggest that TED may have different features in patients who are younger and older than 40 years of age, and that restrictive myopathy and optic neuropathy are more common in the older patients. This is in line with previous reports [7–9, 15]. Moreover, the mean age at diagnosis in most of the case series that were published was around 40 years old [7–9, 18]. Furthermore, it is known that some signs and symptoms of the diseases how little change with age until passing the fifth decade [19].
Finding the correlation between age at diagnosis and prognosis will help us to plan a personalized treatment according to each patient’s prognosis. Moreover, we will be able to give more accurate information to the patients about their prognosis.
Exophthalmos and eyelid retraction are described as being the most common signs of TED in many published series [12, 20, 21]. In our patients, lid retraction was more characteristic to younger patients. The average exophthalmometry measurements were 21.5 in the younger patients and 22.5 in the older patients, although the former were more bothered by proptosis. Eyelid retraction as the initial sign was present in 17 % and 5 % of Groups 1 and 2, respectively (Table 1). Other investigators reported a relatively higher risk of eyelid retraction of up to 90 % and exophthalmos of up to 63 % in cases of TED [20]. Occurrence of all features, i.e., eyelid retraction, exophthalmos, optic nerve dysfunction, extraocular muscle involvement, and hyperthyroidism, is relatively uncommon [20].
DON is one of the most serious sequelae of TED, and if left untreated, it can lead to permanent visual loss or permanent visual field loss [22]. Other studies suggested that although orbital inflammation is a common feature in DON patients, it is not always essential [23]. Most DON patients have a VA of 20/30 or worse, reduced color vision, and visual field defects. Half of those patients may have optic nerve swelling [23]. In the current study, the mean corrected pre-treatment VA was 20/30 and the mean proptosis was 23 mm, values similar to previous reports. Steroids and orbital decompression surgery were reported as being very effective in treating DON [23, 24].
Precise measurements of treatment response are a prerequisite to correct interpretation of therapeutic benefit. This is sometimes difficult in TED [25]. In general, steroids (oral or IV) are effective in treating severe inflammatory signs and optic neuropathy. Orbital irradiation is used to treat inflammation, optic neuropathy, and diplopia secondary to inflammation [26]. Marcocci et al. [27] examined the role of orbital radiotherapy along with oral or IV steroids in patients with severe Graves’ orbitopathy and found that both treatments are equally effective in proptosis and eyelid retraction reduction as well as amelioration of diplopia, but that intravenous (IV) glucocorticoids (along with orbital radiotherapy) were more effective in reducing the clinical activity score. Although optic neuropathy improved by a higher percentage under IV treatments, the difference was not significant. IV glucocorticoids were better tolerated by their patients than oral glucocorticoids and with fewer side effects. Those authors concluded that both treatments are effective in severe TED patients; however, the IV route seems to be more tolerable with fewer systemic side effects.
Most of our patients were treated conservatively: systemic steroids were used in two (9 %) of the Group 1 patients and 27 (25 %) of the Groups 2 patients. Orbital decompression surgery was performed more commonly among the Group 2 patients (19/108, 18 %) since it was almost absent in the Group 1 patients.
Restrictive myopathy was more common in Group 2, resulting in frequent complain of diplopia (54 %) and also strabismus surgery that was performed in 14 (13 %) of the older patients and in none of the younger ones.
Eyelid reposition surgery was performed at a similar rate in both groups (20 %).
According to Nunery histopathological subtypes and our findings, we can conclude that patients under 40 years old have type 1 ophthalmopathy and patients older than 40 have type 2 ophthalmopathy. Our results are similar to previous studies, reporting that patients under 40 years of age tend to demonstrate fat expansion, whereas patients over 60 years of age display more extraocular muscle swelling [28, 29]. We found that among patient with type 2 ophthalmopathy acute external inflammatory signs were less common compared to patients with type 1 ophthalmopathy. We assume it is because type 1 patients have more proptosis and lid lag. None of the patients of type 2 ophthalmopathy underwent surgery.
Most TED patients have mild disease with preserved vision and ocular exam. Good response to anti-inflammatory treatments or surgery when indicated can be anticipated.
Patients under the age of 40 years at onset were less common among our TED series. Moreover, there were only five patients under 21 years old. This is in accordance with the fact that pediatric Graves’ ophthalmopathy is fairly rare [30].
The clinical presentation of the younger group is milder than in the older group, i.e. higher rate of lid retraction and proptosis and lower rate of restrictive myopathy and optic neuropathy. This is in accordance with previous reports. Although there are reports about severe ophthalmopathy in patients younger than 40 years of age, most of the studies revealed increasing severity with older age. This was attributed to the severity of Graves’ disease, which also advances with older age. However, the similarity of the anti-thyroid treatment in both of our groups preclude this explanation for the difference in our TED patients.
Our study is limited by the lack of classification, i.e. clinical activity scores or NOSPECS although it could be helpful in analysing the data. It stems from its retrospective nature and inclusion of participants from two medical centres, which causes lack of uniformity in the allocation of patients.
Our study with long follow-up demonstrates that both groups had favorable outcome although the older group needed more aggressive treatment and surgical interventions. This information may be valuable at the time of diagnosis for planning future management alternatives.
References
Bartley GB (1994) The epidemiologic characteristics and clinical course of ophthalmopathy associated with autoimmune thyroid disease in Olmsted County, Minnesota. Trans Am Ophthalmol Soc 92:477–588
Gerding MN, van der Meer JW, Broenink M, Bakker O, Wiersinga WM, Prummel MF (2000) Association of thyrotrophin receptor antibodies with the clinical features of Graves’ ophthalmopathy. Clin Endocrinol (Oxf) 52(3):267–271
Hondur A, Konuk O, Dincel AS, Bilgihan A, Unal M, Hasanreisoglu B (2008) Oxidative stress and antioxidant activity in orbital fibroadipose tissue in Graves’ ophthalmopathy. Curr Eye Res 33(5):421–427. doi:10.1080/02713680802123532
Bagnasco M, Bossert I, Pesce G (2006) Stress and autoimmune thyroid diseases. Neuroimmunomodulation 13(5–6):309–317. doi:10.1159/000104859
Konuk O, Hondur A, Akyurek N, Unal M (2007) Apoptosis in orbital fibroadipose tissue and its association with clinical features in Graves’ ophthalmopathy. Ocul Immunol Inflamm 15(2):105–111. doi:10.1080/09273940601186735
Saverino D, Brizzolara R, Simone R, Chiappori A, Milintenda-Floriani F, Pesce G, Bagnasco M (2007) Soluble CTLA-4 in autoimmune thyroid diseases: relationship with clinical status and possible role in the immune response dysregulation. Clin Immunol 123(2):190–198. doi:10.1016/j.clim.2007.01.003
Lin MC, Hsu FM, Bee YS, Ger LP (2008) Age influences the severity of Graves’ ophthalmopathy. Kaohsiung J Med Sci 24(6):283–288. doi:10.1016/S1607-551X(08)70154-2
Perros P, Crombie AL, Matthews JN, Kendall-Taylor P (1993) Age and gender influence the severity of thyroid-associated ophthalmopathy: a study of 101 patients attending a combined thyroid-eye clinic. Clin Endocrinol (Oxf) 38(4):367–372
Kendler DL, Lippa J, Rootman J (1993) The initial clinical characteristics of Graves’ orbitopathy vary with age and sex. Arch Ophthalmol 111(2):197–201
Kavoussi SC, Giacometti JN, Servat JJ, Levin F (2014) The relationship between sex and symmetry in thyroid eye disease. Clin Ophthalmol 8:1295–1300. doi:10.2147/OPTH.S61041
Putta-Manohar S, Perros P (2010) Epidemiology of Graves’ orbitopathy. Pediatr Endocrinol Rev 7(Suppl 2):182–185
Lim SL, Lim AK, Mumtaz M, Hussein E, Wan Bebakar WM, Khir AS (2008) Prevalence, risk factors, and clinical features of thyroid-associated ophthalmopathy in multiethnic Malaysian patients with Graves’ disease. Thyroid 18(12):1297–1301. doi:10.1089/thy.2008.0044
Prummel MF, Wiersinga WM (1993) Smoking and risk of Graves’ disease. JAMA 269(4):479–482
Kimball LE, Kulinskaya E, Brown B, Johnston C, Farid NR (2002) Does smoking increase relapse rates in Graves’ disease? J Endocrinol Invest 25(2):152–157
Manji N, Carr-Smith JD, Boelaert K, Allahabadia A, Armitage M, Chatterjee VK, Lazarus JH, Pearce SH, Vaidya B, Gough SC, Franklyn JA (2006) Influences of age, gender, smoking, and family history on autoimmune thyroid disease phenotype. J Clin Endocrinol Metab 91(12):4873–4880. doi:10.1210/jc.2006-1402
Allahabadia A, Daykin J, Holder RL, Sheppard MC, Gough SC, Franklyn JA (2000) Age and gender predict the outcome of treatment for Graves’ hyperthyroidism. J Clin Endocrinol Metab 85(3):1038–1042. doi:10.1210/jcem.85.3.6430
Nunery WR (1991) Ophthalmic Graves’ disease: a dual theory of pathogenesis. OphthalmolClin North Am 4:73–87
Kozaki A, Inoue R, Komoto N, Maeda T, Inoue Y, Inoue T, Ayaki M (2010) Proptosis in dysthyroid ophthalmopathy: a case series of 10,931 Japanese cases. Optom Vis Sci 87(3):200–204. doi:10.1097/OPX.0b013e3181ce5702
Nordyke RA, Gilbert FI Jr, Harada AS (1988) Graves’ disease. Influence of age on clinical findings. Arch Intern Med 148(3):626–631
Bartley GB, Fatourechi V, Kadrmas EF, Jacobsen SJ, Ilstrup DM, Garrity JA, Gorman CA (1996) Clinical features of Graves’ ophthalmopathy in an incidence cohort. Am J Ophthalmol 121(3):284–290
Cockerham KP, Hidayat AA, Brown HG, Cockerham GC, Graner SR (2002) Clinicopathologic evaluation of the Mueller muscle in thyroid-associated orbitopathy. Ophthal Plast Reconstr Surg 18(1):11–17
Neigel JM, Rootman J, Belkin RI, Nugent RA, Drance SM, Beattie CW, Spinelli JA (1988) Dysthyroid optic neuropathy. The crowded orbital apex syndrome. Ophthalmology 95(11):1515–1521
McKeag D, Lane C, Lazarus JH, Baldeschi L, Boboridis K, Dickinson AJ, Hullo AI, Kahaly G, Krassas G, Marcocci C, Marino M, Mourits MP, Nardi M, Neoh C, Orgiazzi J, Perros P, Pinchera A, Pitz S, Prummel MF, Sartini MS, Wiersinga WM, European Group on Graves O (2007) Clinical features of dysthyroid optic neuropathy: a European Group on Graves’ Orbitopathy (EUGOGO) survey. Br J Ophthalmol 91(4):455–458. doi:10.1136/bjo.2006.094607
Ben Simon GJ, Syed HM, Douglas R, Schwartz R, Goldberg RA, McCann JD (2006) Clinical manifestations and treatment outcome of optic neuropathy in thyroid-related orbitopathy. Ophthalmic Surg Lasers Imaging 37(4):284–290
Gorman CA (1998) The measurement of change in Graves’ ophthalmopathy. Thyroid 8(6):539–543
Cockerham KP, Kennerdell JS (2002) Does radiotherapy have a role in the management of thyroid orbitopathy? View 1. Br J Ophthalmol 86(1):102–104
Marcocci C, Bartalena L, Tanda ML, Manetti L, Dell’Unto E, Rocchi R, Barbesino G, Mazzi B, Bartolomei MP, Lepri P, Cartei F, Nardi M, Pinchera A (2001) Comparison of the effectiveness and tolerability of intravenous or oral glucocorticoids associated with orbital radiotherapy in the management of severe Graves’ ophthalmopathy: results of a prospective, single-blind, randomized study. J Clin Endocrinol Metab 86(8):3562–3567. doi:10.1210/jcem.86.8.7737
Bahn RS (2010) Graves’ ophthalmopathy. N Engl J Med 362(8):726–738. doi:10.1056/NEJMra0905750
Forbes G, Gorman CA, Brennan MD, Gehring DG, Ilstrup DM, Earnest F (1986) Ophthalmopathy of Graves’ disease: computerized volume measurements of the orbital fat and muscle. AJNR Am J Neuroradiol 7(4):651–656
Eha J, Pitz S, Pohlenz J (2010) Clinical features of pediatric Graves’ orbitopathy. Int Ophthalmol 30(6):717–721. doi:10.1007/s10792-010-9351-6
Acknowledgments
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ben Simon, G.J., Katz, G., Zloto, O. et al. Age differences in clinical manifestation and prognosis of thyroid eye disease. Graefes Arch Clin Exp Ophthalmol 253, 2301–2308 (2015). https://doi.org/10.1007/s00417-015-3156-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-015-3156-2