Abstract
Purpose
To explore how optic disc perfusion varies in patients with open-angle glaucoma (OAG) and how this correlates with glaucoma severity.
Methods
We performed a prospective and cross-sectional observational study that included 62 eyes from 62 patients with OAG, divided into three groups according to their visual field (VF) results, and 20 eyes from 20 normal control subjects. Optic disc perfusion was studied using optical coherence tomography angiography (angio-OCT), and flow index and vessel density were determined. The VF, mean deviation (MD), pattern standard deviation (PSD), retinal nerve fiber layer (RNFL) thickness, and ganglion cell complex (GCC) thickness were also recorded. The potential associations between disc perfusion and VF defects or structural loss were analyzed.
Results
In OAG patients, the disc flow index and vessel density were significantly lower than in normal controls (all p<0.001) and were correlated with the severity of glaucoma. In OAG eyes, the flow index and vessel density were significantly correlated with MD, RNFL, and GCC thickness (all p<0.01), but were not in the normal controls. The receiver operating characteristic (ROC) curve analysis also revealed that disc flow index and vessel density had the power to differentiate normal eyes from eyes with OAG (under the ROC curves: 0.82 and 0.80, respectively).
Conclusions
Angiograms demonstrated a reduced disc flow index and vessel density in glaucoma, and this reduction was closely related to GCC thickness. This indicated that measurement of disc perfusion by angio-OCT might be important for the monitoring of glaucoma.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Glaucoma is a major disease that potentially results in irreversible blindness. It is the second leading cause of induced vision loss worldwide. For a long period of time, elevated intraocular pressure (IOP) was recognized as the only cause of neural tissue loss at the optic nerve head (ONH), subsequently resulting in visual field loss [1–4]. However, many epidemiological studies have revealed that IOP reduction alone cannot prevent the progression of visual field loss in all patients [5–7]. Besides elevated IOP, a growing body of evidence has suggested that vascular factors play a critical role in the development of glaucoma [8–12]. Some prospective studies have demonstrated that in primary open-angle glaucoma (POAG), blood flow is diminished in the ophthalmic, retinal, choroid, and retrobulbar circulations [10, 13–16]. Although these trials have mainly used Doppler optical coherence tomography (OCT), which is not sensitive enough to measure accurately the low velocities of small vessels that make up the disc microcirculation, they have instigated a resurgence of interest in the metabolic assessment of glaucoma.
OCT, which is able to provide a measurement of retinal thickness, is commonly used in the diagnosis and management of retinal diseases and glaucoma [17–21]. Recently, a newly developed OCT angiography using split-spectrum amplitude-decorrelation angiography (SSADA) has demonstrated the ability to quantify retinal and disc blood flow rapidly and accurately [22–24]. It is a non-invasive technique that does not require the injection of any exogenous dye or contrast agent and provides near-automatic quantification of disc perfusion. Previous research showed that OCT angiography (angio-OCT) with SSADA offers excellent intra-visit repeatability and inter-visit reproducibility in the measurement of disc flow [25]. Its reliability has also been shown in the macular regions [26].
There is a general consensus that ocular blood flow is reduced in glaucoma and that vascular factors might be more prominent in open-angle glaucoma (OAG). Despite this, the study of disc perfusion in patients with OAG has been rare. Additionally, the relationship between the severity of damage of optic disc perfusion and the functional and anatomical changes of glaucoma has not been established. To explore the possible correlation between disc perfusion, neural structure, and visual field loss in OAG patients, we performed the following study using angio-OCT.
Methods
Participants
Eyes from 62 Chinese subjects with OAG and 20 normal control subjects who visited the glaucoma clinic of the Eye & ENT Hospital of Fudan University from November 2013 to April 2014 were prospectively collected. The study was approved by the institutional review board of the Eye & ENT Hospital and was performed in accordance with the tenets of the Declaration of Helsinki. Written informed consent was obtained from all subjects.
The diagnostic criteria for OAG included all of the following: 1) the presence of glaucomatous optic disc damage and abnormal thinning of the circumpapillary retinal nerve fiber layer (RNFL); 2) visual field defects, confirmed on at least two visual field examinations; 3) a normal apparent open angle on gonioscopic examination; and 4) no history of ocular or systemic diseases causing optic nerve damage. The eyes with OAG were divided into three groups based on the progression of their optic nerve damage as measured by visual field: mild (mean deviation [MD] > −6.0 dB), moderate (MD between −6.0 and −12.0 dB), and severe (MD < −12.0 dB). The inclusion criteria for the normal subjects were defined as normal-appearing ONH, intact neuroretinal rim and retinal nerve fiber layer (RNFL), normal standard automated perimetry (defined as a glaucoma hemifield test within normal limits and a pattern standard deviation within 95% confidence-interval limits), and IOP of ≤21 mmHg. The OAG and normal groups enrolled in this study also met the following criteria: 1) no ocular laser or incisional surgery in either eye (including cataract surgery); 2) no history of systemic medications (such as antihypertensive, antihyperlipidemic, or hypoglycemic agents); 3) reliable performance on visual field testing (fixation errors <20%, false-positives <15%, and false-negatives <33%) assessed via the 30–2 SITA standard program of the Humphrey Field Analyzer (HFA, Carl Zeiss Meditec, Dublin, CA, USA); and 4) refractive error within −6.0 diopters. Only one eye per subject was included in the study.
Examination
All subjects were interviewed regarding their medical history. Thorough ophthalmic examinations included refractive status, slit-lamp biomicroscopy, fundus examination, IOP, central corneal thickness (CCT), and gonioscopy, performed by glaucoma specialists. The retinal nerve fiber layer (RNFL) and ganglion cell complex (GCC) thickness were assessed with SD-OCT (RTVue OCT; Optovue Inc., Fremont, CA, USA). Fundus photography was performed with a retinal camera (TRC-NW200, Topcon). IOP was measured using Goldmann applanation tonometry and CCT was measured with an A-scan ultrasound (A-Scan Pachymeter, Ultrasonic, Exton, PA, USA). Both systemic blood pressure (BP) and pulse rate (PR) were measured in the left brachial artery at the height of the heart with an automated blood pressure monitor (Omron Corporation) with the subject in an upright sitting position. BP amplitude was calculated from systolic blood pressure (SBP) and diastolic blood pressure (DBP) according to the following formula: BP amplitude = SBP − DBP. Mean arterial pressure (MAP) was calculated according to the following formula: MAP = DBP + 0.42 (SBP−DBP) [27–29]. Ocular perfusion pressure (OPP) was calculated according to the following formula: OPP = 2/3 MAP-IOP [30]. At the time of the study, the frequency of topical medication use and the number of topical glaucoma medications for each patient were also recorded.
OCT data acquisition and processing
OCT angiography scans were obtained by the spectral domain system RTVue-XR Avanti (Optovue, Inc., software version 2.0.5.39). This system has an A-scan rate of 70 kHz per second, using a light source centered on 840 nm and a bandwidth of 45 nm. Both eyes of each participant were examined and scanned within the same visit. Three-dimensional (3D) OCT angiography scans were acquired over 3 x 3 mm regions by using five repeated B-scans at 216 raster positions, with each B-scan consisting of 216 A-scans. With a B-scan frame rate of 270 frames per second, each scan can be acquired in ~3.5 seconds. Four volumetric raster scans, including two horizontal priority (x-fast) and two vertical priority (y-fast) scans, were obtained consecutively. The best x-fast and y-fast scans were processed by the SSADA algorithm and the motion artifact was removed by 3D orthogonal registration and merging of two scans [23]. En face retinal angiogram was created by projecting the flow signal internal to the retinal pigment epithelium. All of these processes can be achieved using the contained software (version 2.0.5.39).
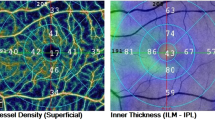
Optic disc perfusion measurements
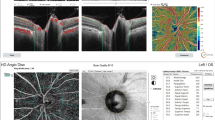
In order to quantify optic disc circulation, en face retinal angiograms were outputted and processed with ImageJ software (ImageJ2x 2.1.4.6 ud4, Wayne Rasband, National Institutes of Health, USA). The disc flow index and vessel density were calculated as previously described [22, 24]. In our study, the optic disc boundary for each image was manually delineated along the OCT reflectance images of normal (Fig. 1a and b) and the glaucoma (Fig. 1d-k) eyes. The boundaries were then transferred to the OCT angiogram map (Fig. 1c, f, i, l) for disc region segmentation. The disc flow index was defined as the average decorrelation value within the disc [22], given by:
where A was the disc area within the disc and D was the decorrelation value acquired by the SSADA algorithm.
Disc photographs (a, d, g, j), optic coherence tomography (OCT) reflectance (b, e, h, k), and OCT angiograms (c, f, i, l) in the eyes of normal subjects (a–c) and OAG patients (d–l). Disc margins are marked by the red elliptical outlines (b, c, e, f, h, i, k, l). A dense microvascular network was visible on the OCT angiography of the normal disc (c). This network was greatly attenuated from mild to severe in the glaucomatous disc (f, i, l).
The vessel density was defined as the percentage area occupied by vessels in the disc, calculated by the following formula:
where A was the disc area within the disc. The threshold decorrelation value used to judge V as 1 or 0 was set at 0.202, two standard deviations above the mean decorrelation value in the noise region. Before calculation of the decorrelation values by SSADA, the central foveal avascular zone in the normal eyes was chosen as a noise region after we applied the same scanning pattern to the macular region.
Repeatability and reproducibility
Intra-visit repeatability of disc flow index was calculated from a subset of 16 normal subjects with two sets of scans performed in a single visit. The coefficient of variation (CV) and the intraclass correlation coefficient (ICC) were calculated by comparing two measurements obtained at the same location by the same operator. The subset of normal subjects used to calculate intra-visit repeatability were also used to calculate inter-visit reproducibility, obtained from two sets of scans performed on two separate visits. The CV and ICC were determined from measurements made by the same operator and obtained on separate visits of the subjects.
Statistical analysis
All analyses were performed using a statistical software package (SPSS for Windows, version 19.0; SPSS, Inc., Chicago, IL, USA). Data are shown as medians (interquartile range [IQR]). The Kruskal-Wallis test was used to analyze the significance of differences among the four groups. The Chi-square test was used for frequency data on gender while the Fisher’s exact test and the Row Mean Scores Differ test were used for frequency of topical medication use and number of topical glaucoma medications. Spearman’s rank correlation test was used to evaluate single correlations between variables. Multiple linear regression analysis was performed to determine independent variables affecting disc perfusion parameters. The receiver operating characteristic (ROC) curve for the disc parameters was plotted to determine the optimum cutoff point, and area under the ROC curve (AUC) was used to determine the discrimination power between the normal and OAG eyes. Repeatability and reproducibility were analyzed by using the CV and the ICC between-measurements. The CV is the standard deviation of the measurements divided by their mean, expressed as a percentage. The ICC measures the proportion of total variability in measurements contributed by variability in measurements between different subjects, and was determined using the random-effects mixed model. The significance level was set at p<0.05.
Results
Baseline clinical characteristics
A total of 62 eyes from 62 subjects with OAG were age-matched with 20 eyes from 20 normal controls. Table 1 summarizes the baseline clinical characteristics of each group; no significant differences were found among these (p-values ranged from 0.203 to 0.961) except for IOP. Compared to the normal controls, the glaucoma eyes demonstrated visual field loss with lower MD values and higher pattern standard deviation (PSD) values (p<0.001) (Table 2). Structural evaluation also identified loss of disc rim area, GCC thickness, and RNFL thickness (p<0.001).
Repeatability and reproducibility of optic disc perfusion measurements
For intra-visit repeatability, the CV and ICC values were 0.68% and 0.99 for the flow index and 0.68% and 0.98 for the vessel density, respectively. These values were based on measurements from 16 normal subjects. For inter-visit repeatability, the CV and ICC values among the 16 normal subjects were 2.8% and 0.82 for the flow index and 3.5% and 0.80 for the vessel density, respectively.
Optic disc perfusion measurements in four groups
Table 2 is an overview of the disc perfusion data of the four groups. Disc flow index (normal vs. mild: p=0.026, normal vs. moderate: p=0.01, normal vs. severe: p<0.001) and vessel density (normal vs. mild: p=0.046, normal vs. moderate: p=0.03, normal vs. severe: p<0.001) were significantly lower in the glaucoma eyes (Figs. 1 and 2) and were correlated with the severity of glaucoma (flow index: r=−0.52, p<0.001; vessel density: r=−0.52, p<0.001).
Optic disc perfusion measurements in four groups. (a) Disc flow index was significantly lower in glaucoma eyes (normal vs. mild: p=0.026, normal vs. moderate: p=0.01, normal vs. severe: p<0.001). (b) Disc vessel density (normal vs. mild: p=0.046, normal vs. moderate: p=0.03, normal vs. severe: p<0.001) was significantly lower in glaucoma eyes. * p<0.05, ** p<0.01
Correlation between optic disc perfusion measurements and other variables
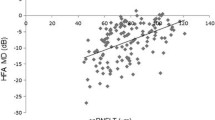
No correlations between the disc flow index, vessel density, age, gender, VF MD, VF PSD, rim area, C/D area ratio, RNFL thickness, or GCC thickness were found in the normal group (data not shown). In the glaucoma groups, the Spearman’s rank correlation test analysis showed that the disc flow index was significantly correlated with VF MD (r=0.379, p=0.003), RNFL thickness (r=0.406, p=0.001), and GCC thickness (r=0.413, p=0.001) (Table 4). Vessel density was significantly correlated with VF MD (r=0.404, p=0.001), VF PSD (r=−0.254, p=0.049), RNFL thickness (r=0.465, p<0.001), and GCC thickness (r=0.45, p<0.001) (Table 3). Also in the glaucoma group, the multiple linear regression analysis, in which the flow index and vessel density were considered the dependent variables (Table 4), showed that GCC thickness was a predictor of flow index and vessel density. Age, gender, VF MD, VF PSD, RNFL thickness, C/D area ratio, and rim area were not significant explanatory variables when grouped with GCC thickness in the multivariate models. This showed that disc perfusion was more strongly linked to GCC thickness than to any other variables.
The power of optic disc perfusion variables to differentiate between normal eyes and OAG eyes
The ROC curves for flow index and vessel density showed that the cutoff point was 0.2432 for flow index and 81.1% for vessel density between the controls and the OAG groups. The cutoff was 0.2431 for flow index and 79.6% for vessel density between the controls and the severe glaucoma groups. The AUCs for flow index (0.9) and vessel density (0.9) showed a greater power to differentiate between normal eyes and eyes with severe OAG (Table 5).
Discussion
In this study, we found a decrease in the disc flow index and vessel density in the glaucomatous eyes, which was correlated with the severity of glaucoma damage. Furthermore, analysis showed that altered flow index and vessel density were correlated with MD, RNFL, and GCC thickness. Altered flow index and vessel density values were also found to be good indicators of eyes with OAG, especially severe OAG. All of these data suggest that angio-OCT disc blood flow measurements showed excellent correlation with the severity of glaucoma.
Our study used a novel technique, SSADA-based angio-OCT, to measure the disc flow index and vessel density in OAG and normal eyes. The reproducibility and repeatability of disc flow index with angio-OCT have been examined primarily in normal subjects. Jia et al. reported that the intra-visit repeatability and inter-reproducibility were 1.2% and 4.2% CV, respectively, for disc flow index in four healthy subjects [22]. However, less information is available from reproducibility studies on disc vessel density. Of note, in our study, good levels of repeatability and reproducibility were found for the disc flow index and vessel density measurements among the 16 normal subjects.
Disc blood flow of patients with glaucoma was previously investigated by fluorescein angiography (FA), in which defects in the disc have been found in glaucomatous and ocular hypertensive eyes [31, 32]. FA, however, is not commonly used to monitor glaucoma because of its invasive nature and the difficulty in quantification. Laser Doppler flowmetry and laser speckle flowgraphy, which are noninvasive techniques, have also been reported as measures of disc perfusion. Studies using these two techniques found that the entire optic disc blood flow was significantly lower in the glaucoma group than in the control eyes [33–36]. Our results agree with these findings. Further, flow index was found to be closely correlated to the severity of both structural loss and visual field loss in glaucoma. Additionally, angio-OCT also offers a new index, disc vessel density measurement, which was also found to be reduced at every stage of OAG. The velocity of the blood flow as well as the vessel diameter might be contributors to the final flow index. Previously, only the flow has been reportedly lower in glaucoma patients. Whether this is the result of decreasing blood flow velocity or a reduction of both the velocity and the vascular system is not known. Here, we report that decreases of both the flow index and of vessel density were found at every stage of OAG. On the other hand, it is still unclear whether vascular changes are a primary or secondary consequence in glaucoma. As this is a cross-sectional study, our result did not answer this question. However, as angio-OCT was able to record the reduced blood flow at every stage of OAG, a follow-up study using angio-OCT might be able to improve our knowledge of this aspect.
The ability to detect OAG with a non-invasive examination such as angio-OCT can become a useful part of annual health examinations. Karczewicz et al. previously reported that blood flow in the ophthalmic artery and the central retinal artery was significantly decreased in patients with myopia and POAG as compared to that in myopic eyes without POAG [37]. Together with our results, this suggests that disc blood flow index and vessel density may aid in the diagnosis of OAG, especially in myopic eyes, in which shallow cupping and pale neuroretinal rims make ONH assessment difficult, and where RNFL thickness measured by OCT has been less effective at discriminating glaucoma [38]. The close correlation between the flow index/vessel density and MD, RNFL, and GCC thickness suggests that angio-OCT might also be useful in monitoring the progression of OAG.
The present study was limited by its cross-sectional design. Though no significant difference was found in the number of glaucoma medications among groups with different stages of OAG, the effects of anti-glaucoma medication might have a potential influence on the findings herein. This study measured blood flow and vessel density in the entire disc; further measurements of the flow in hemispheres or quadrants using angio-OCT might provide more information in this field.
In conclusion, our study demonstrated that disc blood flow measurement may be useful in glaucoma assessment. The authors’ analysis indicated that reduced disc blood flow was associated with structural loss and visual field loss. The data also suggest that disc vascular changes might be secondary in glaucoma. Measurement of disc perfusion by angio-OCT may be important for the monitoring of glaucoma, and further studies with long-term follow-up periods might tell us the prognostic value of this angiogram.
References
Resnikoff S, Pascolini D, Etya’ale D et al (2004) Global data on visual impairment in the year 2002. Bull World Health Organ 82:844–851
Caprioli J (2007) Intraocular pressure fluctuation: an independent risk factor for glaucoma? Arch Ophthalmol 125:1124–1125
Caprioli J, Coleman AL (2008) Intraocular pressure fluctuation a risk factor for visual field progression at low intraocular pressures in the Advanced Glaucoma Intervention Study. Ophthalmology 115:1123–1129
Pan Y, Varma R (2011) Natural history of glaucoma. Indian J Ophthalmol 59:S19–S23
Heijl A, Leske MC, Bengtsson B, Hyman L, Hussein M (2002) Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol 120:1268–1279
Musch DC, Gillespie BW, Lichter PR, Niziol LM, Janz NK (2009) Visual field progression in the Collaborative Initial Glaucoma Treatment Study: the impact of treatment and other baseline factors. Ophthalmology 116:200–207
Collaborative Normal-Tension Glaucoma Study Group (1998) The effectiveness of intraocular pressure reduction in the treatment of normal-tension glaucoma. Am J Ophthalmol 126(4):498–505
Flammer J, Orgul S, Costa VP et al (2002) The impact of ocular blood flow in glaucoma. Prog Retin Eye Res 21:359–393
Schmidl D, Garhofer G, Schmetterer L (2011) The complex interaction between ocular perfusion pressure and ocular blood flow - relevance for glaucoma. Exp Eye Res 93:141–155
Emre M, Orgul S, Gugleta K, Flammer J (2004) Ocular blood flow alteration in glaucoma is related to systemic vascular dysregulation. Brit J Ophthalmol 88:662–666
Leske MC (2007) Open-angle glaucoma: an epidemiologic overview. Ophthalmic Epidemiol 14:166–172
Bonomi L, Marchini G, Marraffa M et al (2000) Vascular risk factors for primary open angle glaucoma: the Egna-Neumarkt Study. Ophthalmology 107:1287–1293
Rojanapongpun P, Drance SM, Morrison BJ (1993) Ophthalmic artery flow velocity in glaucomatous and normal subjects. Br J Ophthalmol 77:25–29
Chung HS, Harris A, Kagemann L, Martin B (1999) Peripapillary retinal blood flow in normal tension glaucoma. Br J Ophthalmol 83:466–469
Yin ZQ, Vaegan, Millar TJ, Beaumont P, Sarks S (1997) Widespread choroidal insufficiency in primary open-angle glaucoma. J Glaucoma 6:23–32
Januleviciene I, Sliesoraityte I, Siesky B, Harris A (2008) Diagnostic compatibility of structural and haemodynamic parameters in open-angle glaucoma patients. Acta Ophthalmol 86:552–557
Puliafito CA, Hee MR, Lin CP et al (1995) Imaging of macular diseases with optical coherence tomography. Ophthalmology 102:217–229
Hee MR, Puliafito CA, Wong C et al (1995) Optical coherence tomography of macular holes. Ophthalmology 102:748–756
Hee MR, Baumal CR, Puliafito CA et al (1996) Optical coherence tomography of age-related macular degeneration and choroidal neovascularization. Ophthalmology 103:1260–1270
Schuman JS, Hee MR, Puliafito CA et al (1995) Quantification of nerve fiber layer thickness in normal and glaucomatous eyes using optical coherence tomography. Arch Ophthalmol 113:586–596
Schuman JS, Hee MR, Arya AV et al (1995) Optical coherence tomography: a new tool for glaucoma diagnosis. Curr Opin Ophthalmol 6:89–95
Jia Y, Morrison JC, Tokayer J et al (2012) Quantitative OCT angiography of optic nerve head blood flow. Biomed Opt Express 3:3127–3137
Jia Y, Tan O, Tokayer J et al (2012) Split-spectrum amplitude-decorrelation angiography with optical coherence tomography. Opt Express 20(4):4710–4725
Wang X, Jia Y, Spain R et al (2014) Optical coherence tomography angiography of optic nerve head and parafovea in multiple sclerosis. Br J Ophthalmol 98:1368–1373
Jia Y, Wei E, Wang X et al (2014) Optical coherence tomography angiography of optic disc perfusion in glaucoma. Ophthalmology 121(7):1322–1332
Wei E, Jia Y, Tan O, Potsaid B, Liu JJ et al (2013) Parafoveal retinal vascular response to pattern visual stimulation assessed with OCT angiography. PLoS One 8(12):e81343
Kaeser P, Orgul S, Zawinka C, Reinhard G, Flammer J (2005) Influence of change in body position on choroidal blood flow in normal subjects. Br J Ophthalmol 89:1302–1305
Longo A, Geiser MH, Riva CE (2004) Posture changes and subfoveal choroidal blood flow. Invest Ophthalmol Vis Sci 45:546–551
Sayegh FN, Weigelin E (1983) Functional ophthalmodynamometry. Comparison between brachial and ophthalmic blood pressure in sitting and supine position. Angiology 34:176–182
Riva CE, Grunwald JE, Petrig BL (1986) Autoregulation of human retinal blood flow. An investigation with laser Doppler velocimetry. Invest Ophth Vis Sci 27:1706–1712
Talusan E, Schwartz B (1977) Specificity of fluorescein angiographic defects of the optic disc in glaucoma. Arch Ophthalmol 95:2166–2175
Schwartz B, Rieser JC, Fishbein SL (1977) Fluorescein angiographic defects of the optic disc in glaucoma. Arch Ophthalmol 95:1961–1974
Piltz-Seymour JR, Grunwald JE, Hariprasad SM, Dupont J (2001) Optic nerve blood flow is diminished in eyes of primary open angle glaucoma suspects. Am J Ophthalmol 132:63–69
Hamard P, Hamard H, Dufaux J, Quesnot S (1994) Optic nerve head blood flow using a laser Doppler velocimeter and haemorheology in primary open angle glaucoma and normal pressure glaucoma. Br J Ophthalmol 78:449–453
Michelson G, Langhans MJ, Groh MJ (1996) Perfusion of the juxtapapillary retina and the neuroretinal rim area in primary open angle glaucoma. J Glaucoma 5:91–98
Yokoyama Y, Aizawa N, Chiba N et al (2011) Significant correlations between optic nerve head microcirculation and visual field defects and nerve fiber layer loss in glaucoma patients with myopic glaucomatous disk. Clin Ophthalmol 5:1721–1727
Karczewicz D, Modrzejewska M (2004) Assessment of blood flow in eye arteries in patients with myopia and glaucoma. Klin Oczna 106(1–2 Suppl):214–216
Melo GB, Libera RD, Barbosa AS, Pereira LM, Doi LM, Melo LJ (2006) Comparison of optic disk and retinal nerve fiber layer thickness in nonglaucomatous and glaucomatous patients with high myopia. Am J Ophthalmol 142:858–860
Funding statement
Project supported by the National Major Scientific Equipment program (Grant No. 2012YQ12008003, China), by the Special Scientific Research Project of Health Professions (Grant No. 201302015, China)
Conflict of interest
Tony Ko is an employee of Optovue, Inc.
Author information
Authors and Affiliations
Corresponding author
Additional information
Xiaolei Wang and Chunhui Jiang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Wang, X., Jiang, C., Ko, T. et al. Correlation between optic disc perfusion and glaucomatous severity in patients with open-angle glaucoma: an optical coherence tomography angiography study. Graefes Arch Clin Exp Ophthalmol 253, 1557–1564 (2015). https://doi.org/10.1007/s00417-015-3095-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-015-3095-y