Abstract
Background
We aimed to report on the clinical findings and long-term prognosis of patients with cytomegalovirus (CMV) anterior uveitis.
Methods
This was a retrospective observational study on 15 immunocompetent patients with CMV anterior uveitis and a follow-up longer than 24 months (mean: 62.1 ± 28.5 months).
Results
Uveitis was unilateral and hypertensive in all cases, with acute relapsing having the characteristics of Posner-Schlossman syndrome in nine (60 %) and chronic in nine patients (40 %), three of whom were clinically classified as Fuchs’ heterocromic iridocyclitis (20 %). All patients received topical antiviral and corticosteroid therapy, with six patients also receiving systemic therapy with valganciclovir or acyclovir. The mean number of uveitis relapses significantly decreased, before and after anti-CMV therapy, from 0.23 ± 0.17 to 0.03 ± 0.03 (p < 0.001), without significant differences among patients treated with topical therapy alone or combined topical and systemic therapy. Cataracts developed in nine out of 13 patients (69.2 %). A chronic raise in intraocular pressure (IOP) was found in 13 patients (86.6 %), with nine requiring surgery (60 %). At the end of the follow-up, all patients had a quiescent uveitis, with ten of them requiring topical low dose steroid therapy (66.6 %) and combined with systemic acyclovir in four cases. Eight patients (53.3 %) were on antiglaucomatous therapy. The last mean IOP value was 14.9 ± 3.6 mmHg (range 8–21 mmHg), and visual acuity was 0.89 ± 0.21.
Conclusions
CMV-associated anterior uveitis has a fairly good long-term visual prognosis. Antiviral therapy can reduce the frequency of relapses, but cataracts and a chronic raise in IOP are frequent complications often requiring a surgical approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cytomegalovirus (CMV) is a member of the human herpes virus family, and in the USA the seroprevalence of CMV infection among individuals aged 6–49 years old is 50.4 % [1] while in France and Italy it ranges between 49.5 and 73.3 %, respectively [2, 3].
CMV retinitis is a well-known entity described in immunocompromised hosts, while only recently it has been recognized as one of the possible etiologic agents of acute or chronic anterior uveitis in immunocompetent patients [4–8]. CMV anterior uveitis might present with either the characteristics of Posner-Schlossman syndrome, or those of a chronic anterior uveitis resembling Fuchs’ heterochromic iridocyclitis, and it might be associated with an acute relapsing or chronic raise in intraocular pressure (IOP) [7, 9]. Endotheliitis is another possible manifestation linked to a CMV infection of the anterior segment of the eye [10–12]. Although CMV-associated anterior uveitis has been usually considered a benign infection, few data are available on its long-term prognosis and complications. The aim of our study was to report on the clinical findings and long-term visual prognosis in immunocompetent patients with CMV anterior uveitis.
Patients and methods
A retrospective chart review was done on immunocompetent patients with unilateral hypertensive uveitis lasting for more than 24 months submitted to aqueous humor analysis by real time polymerase chain reaction (PCR) that resulted in positive for CMV. The patients were observed at our institution between 2004 and 2011. The study was carried out following the ethical standards of the Declaration of Helsinki, and all the patients have given an informed consent before being submitted to aqueous humor analysis. Briefly, in the operating room, after the eye was sterilized using 5 % diluted povidone-iodine as for any ocular surgical procedure and a sterile drape was positioned, an eyelid speculum was inserted to stabilize the eyelids and the tap was performed using a sterile syringe with a 27G needle. A sample 0.1–0.2 ml of humor aqueous was collected and sent immediately to the laboratory where standard PCR-real time procedure was performed for CMV, HSV1, HSV2, VZV, and EBV viruses, either immediately or within one week after storing the aqueous sample at −20 °C. After the aqueous tap, the patients received a combination of dexamethasone and tobramycin eyedrops, three times daily for seven days. All patients underwent a complete ophthalmologic evaluation and a medical history review before the aqueous tap procedure. They also had a complete workup to rule out any other cause of anterior uveitis (complete blood cell count, basic chemistry panel, serum angiotensin converting enzyme levels, venereal disease research laboratory (VDRL) test, a fluorescent treponemal antibody absorption test, erythrocyte sedimentation rate, C-reactive protein, antinuclear antibody, and rheumatoid factor), and an underlying condition of immunodepression (HIV test, T-cell subset, IgG, IgA, and IgM immunoglobulins). The presence of serum antibodies against CMV, HSV 1, HSV2, VZV, and EBV was also tested. All patients showed serum IgG for CMV and no IgM. All the three patients with Fuchs’ heterochromic iridocyclitis (FHI) were also tested for rubella virus in the serum and the result was negative.
Patients were classified as having anterior recurrent or chronic inflammation according to the SUN criteria [13].
Fuchs’ heterochromic iridocyclitis (FHI) was diagnosed in patients presenting diffuse stellate keratic precipitates, mild anterior chamber reaction with or without Koeppe’s nodules, atrophy and depigmentation of the iris with or without heterochromia, and a variable grade of vitreous inflammation, but who show no ciliary reaction, no posterior synechiae, and no retinal involvement unless the patient had been previously submitted to surgery. Posner-Schlossman syndrome (PSS) diagnosis was made after the following features were identified: recurrent attacks of unilateral mild anterior uveitis (few keratic precipitates, flare and cells ≤ 1+) with highly elevated IOP and initially rapid resolution after the administration of topical steroids and hypotensive drugs.
Data were collected on patients demographics, number of uveitis attacks before and after therapy, IOP values, onset of complications, required surgical procedures, changes in visual acuity from baseline and final visual acuity.
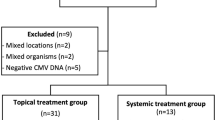
Fifteen patients, nine males (60 %) and six females (40 %), with CMV associated uveitis and a follow-up lasting longer than 24 months, fulfilled the inclusion criteria and were, therefore, included into this study. The mean follow-up was 62.1 ± 28.5 months (range: 24–112 months), with a median of 64 months. Statistical analysis was performed using the t test for paired and unpaired data and the Chi-square test. p values lower than 0.05 were considered statically significant.
Results
Table 1 reports the clinical characteristics of the patients. The mean age at the time of onset of uveitis was 36.1 ± 14.3 years (range: 17–59 years). Uveitis was unilateral and hypertensive in all cases. During the follow-up period, an acute relapsing course was observed in nine patients (60 %) and a chronic one in six (40 %). Clinical diagnoses at our first examination were: Posner-Schlossmann syndrome (PSS) in nine patients (60 %), Fuchs’ heterochromic iridocyclitis (FHI) in three patients (20 %) and chronic anterior uveitis in three cases (20 %). Aqueous humor analysis was performed after a mean period of 60.8 ± 46.4 months from uveitis symptoms onset (range: 13–168 months, median: 39 months).
During our follow-up, corneal involvement was found in two patients only (13.3 %) One patient presented with a corneal stromal infiltrate with endotheliitis during a relapse of uveitis, and the other one with an endotheliitis with IOP increase. Corneal oedema was never detected in patients with the diagnosis of FHI and chronic anterior uveitis, and was observed in four patients with a diagnosis of PSS, three of whom during IOP spikes and one concomitant with endotheliitis. The amount of cells detected in the anterior chamber varied from 0.5 to 4+ cells (mean: 1.4 ± 0.9 cells) and the maximum IOP varied from 26 to 60 mmHg (mean: 41.7 ± 9.1 mmHg). No patient presented posterior synechiae. Koeppe’s iris nodules were present in two patients (16.6 %), both of them carrying a diagnosis of FHI (66.6 % of the patients with FHI).
Thirteen patients (86.6 %) presented stromal iris atrophy, either diffuse (eight patients, 61.5 %), located superiorly or inferiorly (one case each, 7.7 %), peripupillary (two patients, 15.4 %), or sectoral (one case, 7.7 %). Endothelial precipitates, either at our first examination or during follow-up, were generally located centrally, inferiorly or diffusely, but in seven cases (46.6 %) they were also or exclusively located paracentrally or perilimbarly in the superior part of the cornea.
Prior to the diagnosis of CMV uveitis, the patients received a combination of topical steroids and IOP-lowering drugs with or without mydriatics. From the available history and during our follow-up before aqueous humor analysis was performed, they presented 174 relapses in 886 months of follow-up, with a mean of 0.013 uveitis recurrence/month of follow-up/patient.
After the PCR results became available, all patients were treated with topical dexamethasone 0.2 % (4–6 drops daily as loading dose, than gradually reduced) along with topical ganciclovir, five times daily for two weeks and then three times daily for at least four weeks, with no side effects. Corticosteroid therapy was completely stopped in five cases, while ten patients (66.6 %) did not discontinue therapy with dexamethasone 0.2 % one drop/day (seven patients) and one drop every other day (three patients). Two patients also received oral valganciclovir (900 mg twice daily for 21 days, then 450 mg twice daily for the following months), but both of them stopped the therapy because of supervening leukopenia (WBC 3500 cell/mmc and 3450 cell/mmc), five months after starting therapy. Leukopenia resolved without any treatment in 30 days after therapy suspension. One of the patients succeeded in stopping every topical therapy, while the other was on dexamethasone eye drops once daily at the moment of the last visit. Four patients received chronic oral acyclovir (800 mg/day) for a mean period of 16.5 ± 3 months (range: 12–18 months), reporting no side effects. All these patients were on topical dexamethasone once daily in three cases and every other day in the fourth.
During and after the aforementioned therapy, we have observed 23 relapses in 714 months of follow-up, with a mean of 0.002 uveitis recurrence/month of follow-up/patient.
The mean number of uveitis relapses significantly decreased, before and after the diagnosis of CMV anterior uveitis and the administration of the specific therapy, from 0.23 ± 0.17 to 0.03 ± 0.03 (t = 4.395, p < 0.001).
The mean number of uveitis recurrence/month of follow-up/patient did not differ between patients who received topical and systemic antiviral therapy (0.03 ± 0.02) compared with those who received topical therapy only (0.03 ± 0.03, t = 0, p = 1), neither there was a difference in the pre-treatment period (0.19 ± 0.12 versus 0.26 ± 0.2, t = -0.76, p = 0.46). Moreover, with a similar follow-up (68.3 ± 28.2 months versus 58 ± 29.6 months, t = 0.67 p = 0.51), patients treated with systemic and topical antiviral drugs showed the same final IOP (mean: 14 ± 4.1 mmHg versus 15.6 ± 3.3 mmHg, t = −0.84 p = 0.42) and the same final visual acuity (mean: 0.87 ± 0.24 versus 0.9 ± 0.2, t = −0.26 p = 0.8) than those treated with antiviral topical therapy only.
Two out of 15 patients (13.3 %) developed CMV uveitis six months and three months after uneventful cataract surgery. In one patient there was a diagnosis of senile cataract, while the other patient underwent cataract surgery for refractive purposes. Both of them, who had been treated with a four week course of tobramycin and dexamethasone after cataract surgery, presented a chronic uveitis at the time of our first examination with macular oedema. They were treated after the diagnosis of CMV uveitis with topical ganciclovir five times/day for 14 days, thrice/day for 30 days and then once/day and with dexamethasone eye drops, six time/day as a loading dose and then gradually reduced, in combination with beta blockers (both patients) and brimodine (one subject only) to control the IOP (maximum values: 36 and 26 mmHg). In both cases three peribulbar injections of triamcinolone acetonide 40 mg were also administered along with acetazolamide at one half of a tablet thrice/daily to treat macular edema, which resolved after two months, and did not reappear subsequently.
Cataract developed in nine patients (69.2 % of the phakic patients) after a mean period of 61.5 ± 48.3 months from the onset of uveitis (range: 8–156 months, median 48 months). At our first examination one patient had already undergone cataract surgery, six patients presented cataracts and other two patients developed cataract during our follow-up. Standard phacoemulsification with in the bag IOL implantation was performed in eight patients without any complication. One patient presented a macular pucker 172 months after the onset of uveitis and 48 months after cataract surgery. The pucker was responsible for a progressive reduction in visual acuity from 1 to 0.4 and the patient was subjected to vitrectomy and macular peeling with stabilization of visual acuity. The mean final visual acuity of the patients who underwent cataract surgery in our center was 0.81 ± 0.26 (range 0.4 to 1) with 62.5 % of the cases reaching a visual acuity of 1.
An IOP rise requiring chronic therapy or surgery was found in 13 out of 15 patients (87 %) after a mean period of 53.1 ± 65.8 months from uveitis onset (range: 1–228 months, median: 24 months). At our first examination, 13 patients were already on chronic antiglaucomatous drugs. Patients were offered a surgical approach for IOP reduction if the IOP was higher than 24 mmHg on maximum tolerated antiglaucoma medication with or without the presence of visual field and/or optic nerve IOP-related alterations.
Nine patients (60 % of all the patients, 69.2 % of those on chronic antiglaucomatous drugs) did not respond adequately to medical therapy and received trabeculectomy with or without mytomicin. One of these patients required two trabeculectomies, five years apart. Another patient received a Baerveldt valve implantation six months after the first trabeculectomy because of uncontrolled IOP despite maximum medical therapy. A complete success of the surgery (IOP < 21 mmHg without therapy) was achieved in four patients (44.4 %), while five (55.5 %) reached a good control of the IOP with medications (qualified success; mean number of drugs/day: 2.6 ± 1.1, range: 1–4) after a mean follow-up of 43.7 ± 29.5 months from the first surgery (range: 18–81 months). Seven out of nine patients with Posner-Schlossman syndrome required glaucoma surgery (77.7 %), while only two out of six patients with Fuchs’ heterochromic iridocyciclitis or chronic anterior uveitis received trabeculectomy (33.3 %) (χ 2: 1.4, p = 0.24).
At the end of follow-up (mean: 62.1 ± 28.5 months) all patients had a quiescent uveitis, with ten of them (66.6 %), under topical low dose steroid therapy (dexamethasone 0.2 % 1 drop/day: seven patients, 1 drop every other day: three patients), combined in four cases with systemic acyclovir 800 mg/day. None of the patients developed retinal lesions. Eight patients (53.3 %) were on antiglaucoma therapy with a mean of 2.38 ± 0.74 drugs/day. At the last examination the mean IOP was 14.9 ± 3.6 mmHg (range 8–21 mmHg), and mean visual acuity was 0.89 ± 0.21, with only the patient operated on for macular pucker presenting a visual acuity reduction from the baseline level.
Discussion
CMV anterior uveitis in immunocompetent patients is a newly recognized uveitis entity [4–9]. This might be because an aqueous tap is not universally performed in patients with anterior uveitis; therefore, many cases of anterior uveitis, mainly hypertensive, are classified as either viral, without definite conclusion of the precise virus involved, or idiopathic. Nevertheless the first description of the pathogenic role of CMV in anterior uveitis dated back to 1987, when Bloch-Michel clearly demonstrated that CMV could be responsible for the onset of Posner-Schlossman syndrome [14]. Fifteen years later, CMV was proven to be the etiologic agent of other uveitic entities in immunocompetent patients [4–9], but few studies debated on the clinical course and long-term visual prognosis of European immunocompetent patients with CMV anterior uveitis [4–6]. In our series we have found that CMV anterior uveitis is more frequent in males (60 %), but without statistical difference from the usual distribution between genders found in our uveitis series (1,417 patients; males: 47 %, females 52.9 %) [15]; this male prevalence seems similar in different ethnic groups, ranging from 60 % to 85.7 % [5–8, 16–18]. Differently from the series reported in Singapore [7], we have observed three patterns of clinical presentation of CMV uveitis: the most frequent was Posner-Schlossman syndrome (60 % of the cases) showing a sudden, limited and acute course, followed by FHI (20 %) and chronic iridocyclitis, not fulfilling the usually accepted diagnostic clinical criteria for the previous entities (20 %). Therefore, CMV might be responsible for a uveitis showing either a sudden, limited and acute course or an insidious persistent and chronic course. It has been reported that in Posner-Schlossman syndrome and in CMV anterior uveitis there is usually a mild degree of inflammation in the anterior chamber, with cells ≤ 2+ according to SUN classification [5, 7, 16, 19]. This is also our experience, where 93.3 % of the patients were found to have anterior chamber cells ≤ 2+. The only patient who showed more than 2+ cells in the anterior chamber developed a CMV anterior uveitis six months after uneventful cataract surgery. Patients with ocular CMV infection can present with corneal involvement. It usually appears as an endotheliitis, and it has been reported in approximately 30 % of Asian or European patients with CMV uveitis [5, 8]. In our series, endotheliitis was not a prominent clinical feature, being found in 16.6 % of the patients only, all responding well to topical antiviral and corticosteroid therapy. Iris atrophy is another clinical feature typically reported in patients with anterior uveitis due to different viruses. It might be caused by either a viral invasion of the iris stroma and/or by ischemic necrosis due to occlusive vasculitis, while recurrent episodes of IOP increase might also contribute to its development [5]. In patients with a CMV proven anterior uveitis, the rate of iris atrophy is variable, ranging from 0 to 100 % of the patients [4–8, 19]. We have found iris atrophy in 86.6 % of our patients, but we were unable to define the exact time of its development, because all patients had a long-standing uveitis at the time of our first examination. It is reasonable to believe that different pathogenic mechanisms can produce iris atrophy in patients with CMV anterior uveitis, and the different frequency found in the literature might be due to the different duration of the disease, in our patients being on average more than five years. Iris nodules (Koeppe’s nodules) were present in two patients only (13.3 %), both of them carrying the diagnosis of FHI (66.6 % of patients with FHI). No patient developed posterior synechiae, which have been reported only in 40 % of French patients [6].
Cataract is the second most frequent complication of CMV uveitis (69.2 % of our patients) with a median delay of 48 months from the onset of uveitis. It seems again reasonable to correlate the onset of cataract with the duration of the corticosteroid therapy, and in some cases, to the underlying uveitis as well. From our data, it is impossible to ascertain whether a prompt specific uveitis treatment would be able to avoid or to delay cataract formation, because 75 % of our patients had cataract since our first examination. Nevertheless, we have experienced that cataract extraction with phacoemulsification and in the bag IOL implantation is a safe procedure in this patient population, and that a good visual rehabilitation can be achieved (final visual acuity of 10/10 in 62.5 % of the patients), without a negative effect on the clinical course of uveitis. On the other hand, we have to stress the possibility that CMV anterior uveitis might follow an uneventful cataract extraction in otherwise healthy patients. Zamir and colleagues. reported the case of a Chinese-Australian patient with bilateral long-standing uveitis who developed CMV-related corneal endotheliitis after cataract surgery in one eye [12]. Both our patients who developed CMV uveitis after cataract extraction resulted IgG positive and IgM negative for CMV in the serum as long as they had been diagnosed. Both of them have had no systemic symptoms suggestive of CMV systemic infection after surgery; therefore, it is difficult to determine whether CMV uveitis has occurred because of a surgery-driven reactivation of a previous asymptomatic ocular infection or if it was due to a newly acquired infection. Another explanation of the onset of a CMV anterior uveitis after cataract surgery is the possibility that topical corticosteroids given postoperatively favoured a viral infection, despite considering that the onset was observed two and five months after the discontinuation of the steroid therapy, respectively. IOP increase is usually present in patients with viral anterior uveitis, as well as in those with CMV anterior uveitis [5–7]. It seems to be a typical feature of patients with CMV anterior uveitis: we have found a chronic IOP raise in 93.3 % of our patients, in agreement with other observations done in Chinese, Malay, French, Dutch and Japanese patients (100 % of the cases) [5–7, 20]. In a recent study on PSS, Sobolewska and colleagues. have found an IOP increase with spikes in all patients, and ten out 11 (90.9 %) of them needed antiglaucomatous drugs or surgery at various end-points during their follow-up [16]. The mechanism of IOP increase may be variable in those patients over time: initially the IOP increase is almost exclusively due to trabeculitis, but over a long time, chronic changes in the trabecular meshwork usually appear, leading to reduced aqueous humor outflow [6] and permanent IOP increase, sometimes unresponsive to medical therapy. In our series 60 % of the patients did not respond adequately to medical treatment and needed a surgical procedure. The indication we have used for surgical procedure was the presence of an IOP higher than 24 mmHg on maximum tolerated medical therapy, with or without visual field and/or optic nerve alterations, and this can explain why the rate of surgical procedure is so high. It is of note that the need for surgery to control the IOP was more frequent, although not statistically significant, in patients with PSS (78 % of the cases), rather than in other uveitic entities (33.3 %). In China it has been reported that 33.3 % of the patients with CMV anterior uveitis need surgery to control IOP before a specific treatment was given [19], while Sobolewska and colleagues reported that 36.4 % of the patients required glaucoma surgery in addition to valganciclovir therapy for uncontrolled IOP [16]. Nevertheless in their series many other patients have undergone several glaucoma procedures before entering their study [16]. The high frequency of IOP increase we found might be either due to the long-term follow-up of our patients and/or to the long period of time occurring between the onset of the disease and the referral to a tertiary eye care center. In this setting, it has been reported that a prompt diagnosis and appropriate therapy in PSS affected patients can contribute to a better control of the IOP and to a reduced rate of surgical procedures [16]. Among the surgical procedures we performed trabeculectomy, with or without the use of perioperative topical mytomicin C. One of the operated patients needed a second trabeculectomy five years later and another patient required a valve implant six months after the previous trabeculectomy, because of uncontrolled IOP despite maximum tolerated medical therapy. At the end of follow-up a complete control of the IOP (mean: 14.9 ± 3.6) was obtained in all cases, with the 44.4 % not needing any therapy (complete success), and the 55.5 % being on a hypotensive therapy with a mean of 2.38 ± 0.74 drugs/day (qualified success).
One limitation of our study is that only patients tapped once for the research of CMV DNA in aqueous humor were considered. As a consequence, there may be the possibility not to include those patients whose aqueous humor resulted negative for viruses, although their clinical diagnosis was compatible with PSS. Negative results in the PCR analysis of the aqueous humor might be due to the small volume of aqueous tested or to the short-lived DNA [16]; therefore, some authors suggest to repeat the tap especially if the clinical findings are equivocal or if a systemic treatment with potential side effects carrying agents is advisable [7, 9, 16].
The most appropriate therapy for CMV anterior uveitis in immunocompetent patients has not yet been established . Some authors suggest using systemic ganciclovir, valganciclovir and/or intravitreal ganciclovir [4–8, 17–19]. It is important to note that ganciclovir is a virustatic and not virucidal agent; therefore, a therapeutic course might not be able to eradicate the virus from the infected organ. This is the reason why Chee and colleagues observed a recurrence of uveitis in 80 % of cases, even in patients treated systemically with a 12-week course of valganciclovir, and in 100 % of those treated with intravitreal injections [17]. A recurrence rate varying from 0 to 100 % has been reported in other small case series treated with either systemic therapy or intravitreal injections [4–8, 17–19]. Furthermore, it is important to stress that ganciclovir or valganciclovir systemic therapy to control CMV uveitis needs a prolonged course with a greater potential for morbidity, as we have encountered in two of our patients who received such a therapy. In the Posner-Schlossman syndrome, for affected patients who received a long-term treatment, Sobolewska and colleagues. were able to achieve a resolution of the inflammatory activity in 63.6 % of patients, and to discontinue the treatment in 86 % of them. Nevertheless, in 33.3 % of cases, they have experienced a relapse [16]; no systemic side effects were described for such a long-term therapy, but 36.4 % of patients required glaucoma surgery in addition to systemic therapy to control the IOP [16].
Ganciclovir gel was also given to treat CMV uveitis in immunocompetent patients [17, 21]. Its response rate was unpredictable: two thirds of patients were responsive, but 57 % of cases with acute recurrent uveitis and 25 % of those with chronic uveitis, relapsed [17]. Systemic acyclovir is effective as a prophylactic treatment in patients with herpetic epithelial and stromal keratitis [22], not carrying important side effects, but it was not demonstrated that it might exert any effect on patients with CMV associated uveitis. In solid organ recipients, it showed a significantly greater prophylactic power against CMV infections compared to placebo, but lower than ganciclovir [23]. Valaciclovir was proven effective in treating one patient with CMV anterior uveitis [24] and it seems to have the same effect as acyclovir in preventing CMV infection in solid organ transplant patients [23]. The dilemma on the therapeutic choice in CMV anterior uveitis relies on the consideration that the great majority of reported patients showed mild to moderate inflammation (cells ≤ 2+), and few, if any, sight-threatening complications have been reported so far. Therefore, an accurate risk to benefit ratio in the therapeutic decision needs to be found. All our patients were treated with topical antiviral and corticosteroid therapy, and six of them received also a systemic therapy (acyclovir, four patients; valganciclovir, two cases), and a prolonged therapy with topical low-dose corticosteroids after the antiviral treatment was also given to ten patients. Overall, such a treatment lead to a significant reduction in the mean recurrence/month of follow-up rate (from 0.013 to 0.002), with the mean number of relapses significantly decreased after this therapeutic strategy from 0.23 ± 0.17 to 0.03 ± 0.03 (p < 0.001). No statistically significant difference was found comparing the patients treated with topical therapy to those receiving systemic and topical antiviral treatment in terms of uveitis recurrence, IOP value, and visual acuity at the last examination.
It is important to stress that our study was not a prospective one, its primary aim was not to report on different therapeutic regimens, and that a limited number of patients was included in both arms. Therefore, the results cannot allow definite conclusions on the most appropriate therapeutic strategy for CMV anterior uveitis and further prospective studies on this topic are warranted.
Finally, CMV anterior uveitis might be more common than usually thought in immunocompetent patients, even in non-Asian patients. It might present either as a sudden onset entity with an acute, limited course, as it was described in Posner-Schlossman syndrome, or with an insidious onset and a persistent chronic course. Glaucoma is the most common complication, in many cases needing surgery in long-term follow-up. Cataract is also frequent: it might be principally due to the corticosteroid therapy, and its surgical approach is usually safe and a good visual rehabilitation is possible. The absence of posterior complications, the virustatic properties of every anti-cytomegalovirus available therapy, and the possible related side effects, might be a concern about the use of systemic anti-cytomegalovirus drugs. Uveitis control can be achieved with topical therapy, but further studies are needed to investigate whether a systemic therapy might prevent the onset of complications and decrease the need for surgery.
References
Bate SL, Dollard SC, Cannon MJ (2010) Cytomegalovirus seroprevalence in the United States: the national health and nutrition examination surveys, 1988-2004. Clin Infect Dis 50:1439–1447
Lepage N, Leroyer A, Cherot-Kornobis N, Lartigau I, Miczek S, Sobaszek A (2011) Cytomegalovirus seroprevalence in exposed and unexposed populations of hospital employees. Eur J Clin Microbiol Infect Dis 30(1):65–70
De Mattia D, Stroffolini T, Arista S, Pistoia D, Giammanco A, Maggio M, Chiaramonte M, Moschen ME, Mura I, Rigo G, Scarpa B (1991) Prevalence of cytomegalovirus infection in Italy. Epidemiol Infect 107(2):421–427
Markomickelakis NN, Canakis C, Zafirakis P, Marakis T, Mallias I, Theodossiadis G (2002) Cytomegalovirus as a cause of anterior uveitis with sectoral iris atrophy. Ophthalmology 109:879–882
van Boxtel LAA, van der Lelij A, van der Meer J, Los LI (2007) Cytomegalovirus as a cause of anterior uveitis in immunocompetent patients. Ophthalmology 114:1358–1362
de Schryver I, Rozenberg F, Cassoux N, Michelson S, Kestelyn P, LeHoang P, Davis JL, Bodaghi B (2006) Diagnosis and treatment of cytomegalovirus iridocyclitis without retinal necrosis. Br J Ophthalmol 90:852–855
Chee SP, Bacsal K, Jap A, Se-Thoe SY, Cheng CL, Tan BH (2008) Clinical features of cytomegalovirus anterior Uveitis in immunocompetent patients. Am J Ophthalmol 145:834–840
Park SW, Yu HG (2013) Association of cytomegalovirus with idiopathic chronic anterior with ocular hypertension in Korean patients. Ocul Immunol Inflamm 21:192–196
Kongyai N, Sirirungsi W, Pathanapitoon K, Tananuvat N, Kunavisarut P, Leechanachai P, De Groot-Mijnes JD, Rothova A (2012) Viral causes of unexplained anterior uveitis in Thailand. Eye 26:529–534
Chee SP, Bacsal K, Jap A , Se-Thoe SY, Cheng CL, Tan BH (2007) Corneal endotheliitis associated with evidence of cytomegalovirus infection. Ophthalmology 114:798–803
Alfawaz A (2013) Cytomegalovirus-related corneal endotheliitis: a review article. Saudi J Ophthalmol 27:47–49
Zamir E, Stawell R, Jhanjii V, Vajpayee RB (2011) Corneal endotheliitis triggered by cataract surgery in a Chinese patient with cytomegalovirus anterior uveitis. Clin Exp Ophthalmol 39:913–915
The standardization of uveitis nomenclature (SUN) working group (2005) Stadardization of uveitis nomenclature for reporting clinical data. Results of the first international workshop. Am J Ophthalmol 140:509–516
Bloch-Michel E, Dussaix E, Cerqueti P, Patarin D (1987) Possible role of cytomegalovirus infection in the etiology of Posner-Schlossman syndrome. Int Ophthalmol 11:95–96
Pivetti-Pezzi P, Accorinti M, La Cava M, Colabelli Gisoldi RAM, Abdulaziz MA (1996) Endogenous uveitis: an analysis of 1,417 cases. Ophthalmologica 210:234–238
Sobolewska B, Deuter C, Doycheva D, Zierhut M (2014) Long-term oral therapy with valganciclovir in patients with Posner-Schlossman syndrome. Graefes Arch Clin Exp Ophthalmol 252:117–124
Chee SP, Jap A (2010) Cytomegalovirus anterior uveitis: outcome of treatment. Br J Ophthalmol 94:1648–1652
Wong VW, Chan CK, Leung DY, Lai TY (2012) Long-term results of oral valganciclovir for treatment of anterior segment inflammation secondary to cytomegalovirus infection. Clin Ophthalmol 6:595–600
Hwang YS, Lin KK, Lee JS, Chang SH, Chen KJ, Lai CC, Huang JC, Kuo YK, Hsiao CH (2010) Intravitreal loading injection of ganciclovir with or without adjunctive oral valganciclovir for cytomegalovirus anterior uveitis. Graefes Arch Clin Exp Ophthalmol 248:263–269
Miyanaga M, Sugita S, Shimizu N, Morio T, Miyata K, Maruyama K, Kinoshita S, Mochizuki M (2010) A significant association of viral loads with corneal endothelial cell damage in cytomegalovirus anterior uveitis. Br J Ophthalmol 94:336–340
Pavan-Langston D, Welch CL, Zegans ME (2012) Ganciclovir gel for cytomegalovirus keratouveitis. Ophthalmology 119:2411
The Herpetic Eye Disease Study Group (1998) Acyclovir for the prevention of recurrent herpes simplex virus eye disease. N Engl J Med 339:300–306
Hodson EM, Ladhani M, Webster AC, Strippoli GF, Craig JC (2013) Antiviral medications for preventing cytomegalovirus disease in solid organ transplant recipients (review). Cochrane Database Syst Rev. doi:10.1002/14651858, PMID: 23450543
Sira M, Murray PI (2007) Treatment of cytomegalovirus anterior uveitis with oral valaciclovir. Ocul Immunol Inflamm 15:31–32
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
All authors approved the revised version.
Rights and permissions
About this article
Cite this article
Accorinti, M., Gilardi, M., Pirraglia, M.P. et al. Cytomegalovirus anterior uveitis: long-term follow-up of immunocompetent patients. Graefes Arch Clin Exp Ophthalmol 252, 1817–1824 (2014). https://doi.org/10.1007/s00417-014-2782-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-014-2782-4