Abstract
Summary
A new dye for vitreoretinal surgery comprised of soluble lutein/zeaxanthin 1 % and brilliant blue 0.025 % is advantageous compared with other dyes currently used for chromovitrectomy, and showed no signs of toxicity at 1 month of follow-up.
Purpose
To evaluate the feasibility and safety of a dye [soluble lutein/zeaxanthin (LZ) 1 % and brilliant blue (BB) 0.025 %] for improving removal of vitreous, epiretinal membranes (ERM), and internal limiting membranes (ILM) in humans.
Methods
We prospectively evaluated 18 eyes treated surgically for a macular hole or ERM. Eighteen surgeons performed chromovitrectomy using the dye, and completed a questionnaire to evaluate the efficacy and safety of the dye. . Examinations included best-corrected visual acuity and intraocular pressure measurements and optical coherence tomography, fluorescein angiography, and autofluorescence performed at baseline and days 1, 7, and 30 postoperatively.
Results
The green dye was deposited on the posterior pole; vigorous dye flushing into the vitreous cavity was unnecessary. All surgeons reported that the ILM stained greenish-blue; 94.4 % reported ILM peeling adequate; the ERM stained poorly. No evidence of toxicity was observed.
Conclusion
The new dye deposited on the posterior pole due to its higher density. The ability to stain the ILM was similar to BB. The new dye has ability to stain the vitreous, hyaloid, and especially the ILM satisfactorily. The new dye may be useful during chromovitrectomy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vitreoretinal surgery involves complex and delicate vitreoretinal techniques to manage many vitreoretinal diseases, macular hole (MH), epiretinal membrane (ERM), and vitreomacular traction syndrome. Chromovitrectomy [1] includes the use of vital dyes or crystals to improve visualization of the intraocular tissues during vitrectomy.
The ideal vital dye should be safe for intraocular use, selectively stain the intraocular membranes, and be eliminated rapidly from the eye. Many dyes are available for chromovitrectomy [1–7], i.e., trypan blue (TB), brilliant blue (BB), indocyanine green (ICG), and infracyanine green. ICG is currently used to stain the internal limiting membrane (ILM) to aid peeling, even though there are concerns about retinal toxicity [8]. TB is thought to be the ideal dye for ERM identification, ICG and BB are ideal for ILM peeling, and triamcinolone acetonide (TA) is useful for vitreous identification [1–7]. Despite this, the United States Food and Drug Administration has not approved any dyes for use during chromovitrectomy. Currently, BB is not approved for human use in the US, and other agents such as ICG, TB, and TA are considered off-label drugs to be used during vitreoretinal procedures. However, BB is approved for chromovitrectomy in Europe.
Lutein and zeaxanthin are lipophilic pigments belonging to the group of carotenoids traditionally found in fruits and vegetables [9, 10]. These carotenoids are also physiologically present in the macula lutea, an integral retinal structure in humans [11]. The carotenoids are structural isomers that have a hydroxyl group at the terminal part of the molecule, which partly explains their different polarities and tropism for certain biologic structures such as the macula [12–15]. Both are considered to be dyes, and are associated with prevention of age-related maculopathies due to their antioxidant effects and exclusive distribution in the macula [11, 16, 17].
Lutein- and zeaxanthin-based dyes alone or combined with BB also might be used effectively as intraocular dyes in human cadaveric eyes to stain different intraocular microstructures, including the ILM [18].
The current study evaluated the feasibility, advantages, and safety of a novel dye (soluble lutein/zeaxanthin [LZ] 1 % with BB 0.025 %) for improving identification and removal of the vitreous, hyaloid, ERM, and ILM performed by different surgeons.
Patients and methods
We prospectively studied 18 eyes of 18 consecutive patients (16 women, two men; mean age, 67.2 ± 7.7 years; range, 50–85 years); 50 % of patients were Caucasian, 44 % were African-American, and 5.6 % were Hispanic. Patients had a diagnosis of macular hole or ERM, and underwent pars plana vitrectomy (PPV) using the combined soluble formulation of LZ 1 % with BB 0.025 %. Inclusion criteria allowed inclusion of eyes with chronic macular hole and/or chronic ERM. Tables 1 and 2 show the patient preoperative and postoperative data. The Ethics Committee of the Federal University of São Paulo approved the study, which was conducted according to the research guidelines of the Association of Research in Vision and Ophthalmology and the tenets of the Declaration of Helsinki. The protocol was registered at www.clinicaltrials.gov (number NCT01627977). All patients provided informed consent regarding the benefits and risks of the surgical procedure and the new dye tested.
Dye preparation
The preparatory technique described below is valid for lutein and zeaxanthin regardless of the chemical form, purity, crystallization, or degree of esterification. The primary steps in the current study were development of a water-soluble solution, characterization of the absorbance of the LZ solution with the Aquamate device™ (Thermo Spectronic, Cambridge, UK), and identification of the resultant color of the chromophore groups. The physicochemical parameters were tested for the optimum pH, osmolarity/osmolality, and concentration. We performed solubility tests in water and polyvinyl alcohol, with ultraviolet spectrophotometry, and analyzed blends comprised of different colors within the visible spectrum.
Preparation
For the final formulation, the active component BB G-B0770™ (Sigma-Aldrich, St. Gallen, Switzerland) and lutein and zeaxanthin were weighed using the H33AR™ balance (Mettler Toledo, Barueri, Brazil), and when stirred with the Q298-1™ device (Quimis, Diadema, Brazil), dissolved in a buffer solution (pH, 7.0-7.4); the pH was checked using the Q600M device™ (Quimis), and balanced saline solution (BSS) served as a control for the osmolarities. The syringes were filled in a sterile area with one 0.5-ml dose of the dye solution, and each syringe was connected to a rubber stopper and then crimped. The final solution was sterilized by autoclaving for 20 min at 121 °C in the Controller Odt-74 version 2.0™ (Wilson Autoclaves, São Paulo, Brazil).
The final dye solution contained LZ 1 % and BB 0.025 % (osmolarity, 280 mOsm; density, 1.1; pH, 7.00). The new 0.5-ml syringes were bottled and stored at 4–8 °C, and used within 30 days of production.
Inclusion and exclusion criteria
Patients of both genders were included if they were older than 18 years, not pregnant, and required an elective vitrectomy to treat a macular hole of any size and any BCVA level or an ERM with a BCVA below 20/25. Patients were excluded if they had any ocular condition that could limit or affect the postoperative results.
Physical evaluation and ocular examinations
All patients underwent a physical evaluation preoperatively that included measurement of the systemic blood pressure and heart rate. An ocular examination was performed preoperatively and 1, 7, and 30 days postoperatively, which included spectral-domain optical coherence tomography (SD-OCT) and fluorescein angiography (FA) using the Spectralis device (Heidelberg Engineering, Heidelberg, Germany), unless media opacity was present.
The BCVA was measured using the Early Treatment Diabetic Retinopathy Study (ETDRS) chart, and the intraocular pressure (IOP) was measured using a Goldmann tonometer; a slit-lamp evaluation also was performed.
Surgical procedures
Eighteen surgeons experienced in current chromovitrectomy performed the standardized surgical procedures. Phakic patients underwent standard combined phacoemulsification with IOL and then 3-port pars plana vitrectomy using 23-gauge instruments. After this, 0.3 ml of the new dye was delivered gently through the posterior pole using a 23-gauge soft-tip cannula (Synergetics, O’Fallon, MO, USA). Flushing of the dye was not needed because it was heavier than BSS (density, 1.1). After the vitreous was removed, a second flush of 0.3 ml of the combination dye was delivered through the posterior pole using the same technique as described previously. Octafluoropropane 15 % was injected into the vitreous cavity. The patients were instructed to remain prone for 3 days postoperatively.
Questionnaire
After each procedure, the surgeons completed a questionnaire that compared the ability of the combination dye to stain the intraocular structures. The findings were compared with the surgeons’ experience with the dyes currently used in chromovitrectomy (Table 3).
Follow-up
The patients underwent a complete ophthalmologic examination on days 1, 7, and 30 postoperatively that included measurement of the BCVA, IOP measurement, and a slit-lamp evaluation. SD-OCT of the macular area was performed when the media was transparent preoperatively, and on days 1, 7, and 30 postoperatively. On postoperative day 30, fundus imaging, FA, and autofluorescence were performed. A parametric tailed Student's t-test was used for statistical analyses of the BCVA improvement and IOP variations. P < 0.05 was considered statistically significant.
Results
The final solution of the combination dye contained soluble LZ 1 % and BB 0.025 % (osmolarity, 280 mOsm; density, 1.1; pH, 7.00) and resulted in a green solution.
Clinical and intraoperative findings
Each of the 18 surgeons performed surgery on only one patient in this series, and no systemic effects were noted during the follow-up period. With regard to the causes leading to surgery, MH was diagnosed in 16 patients and ERM was observed in two eyes. The mean baseline number of ETDRS letters was 10.6 ± 11.6 (range, 0–37) and the mean number of ETDRS letters on day 30 postoperatively was 12.4 ± 10.6 (range, 0–35). All eyes were followed for 30 days.
Intraoperative findings
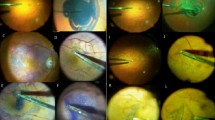
Phaco-vitrectomy was performed in 17 eyes, and vitrectomy alone in one pseudophakic eye. All procedures were performed uneventfully. Five intraoperative characteristics of the new dye were observed: first, the solution consisted of soluble orange LZ 1 % previously mixed with blue BB 0.025 %, which resulted in a green solution (Fig. 1). Second, the solution was deposited on the posterior pole due its higher density than BSS, and there was no need to flush vigorously (Fig. 2). Third, the dye indirectly showed the posterior hyaloid and the vitreous base by deposition of soluble lutein in the posterior vitreous. Fourth, the solution stained the ILM a marked greenish-blue (Fig. 3). Fifth, the solution had poor affinity for the ERM.
Follow-up
On postoperative day 30, no dye-related abnormalities were observed by FA, autofluorescence, or OCT. MH persisted in six cases, and IOP did not change significantly (P = 0.6061) (Table 1). No dye-related changes were observed by biomicroscopy or funduscopy, and no adverse event occurred during the follow-up period.
Questionnaire
The responses to the questionnaire that compared the ability of the soluble LZ-based dye to stain the distinct intraocular structures with the experience of the 18 surgeons who had been using the “gold-standard dyes” during chromovitrectomy indicated that all surgeons considered that the ILMs were stained similarly to their experience using BB; All surgeons considered satisfactory the staining of the dye; 44.4 % considered the stain to be a weak greenish-blue and 55.6 % considered it an intense greenish-blue (P < 0.001) (Table 3). Moreover, 94.4 % identified dye deposition in the vitreous (P < 0.001), although this was less effective than their experience with TA (Table 3); no lutein crystals were present due to the soluble solution. At the end of the procedure, one surgeon reported that the dye was in the vitreous base in one patient (5.6 %; P < 0.02). Other surgeons considered the washout satisfactory, with no evidence of the dye at the end of surgery (Table 3).
Discussion
A previous study reported that a solution containing LZ 1 % crystals and BB 0.025 % efficiently stained the vitreous, ILM, and posterior hyaloid in cadaver eyes [18]. Clinical, histologic, and electroretinographic evaluations after intravitreal injections of these dye concentrations in rabbit eyes showed no signs of toxicity (unpublished data). In addition, lutein crystals 1 % in combination with BB 0.025 % also were used safely in 12 eyes and were advantageous intraoperatively because only one dye was used to remove both the posterior hyaloid/vitreous base and the ILM; however, only one surgeon performed all the procedures [19]. All studies supported the decision to test the soluble formulation of LZ 1 % and BB 0.025 % during chromovitrectomy in human eyes, resulting a final green solution (Fig. 1) that was denser than BSS and did not require flushing of the posterior pole (Fig. 2).
In the current study, the posterior hyaloid and the vitreous base were identified easily after deposition of the LZ dye in 18 eyes. The ILM was identified easily and peeled promptly using an intraocular forceps (Fig. 3). The possibility of performing all the chromovitrectomy steps using only one dye for different structures is convenient, because currently two different substances are used for these distinct surgical maneuvers, i.e., TA is used to identify the posterior hyaloid/vitreous base and BB/ICG is used to identify the ILM [20].
In addition, because the LZ molecule has a physiologic antioxidant effect, the theoretical safety profile of the current dye may increase because the singlet oxygen generated by the BB molecule exposed to the endoillumination light may be quenched by the lutein molecule. Further basic and clinical studies are needed to validate this hypothesis [18, 21].
The BCVA improved compared with baseline in almost three-quarters (72 %) of patients, and the BCVA did not change in 28 % compared to the initial BCVA. No signs of toxicity [including retinal pigment epithelial (RPE) abnormalities at the subfoveal area] were seen during the 30-day follow-up period during ocular examinations, OCT, FA, and autofluorescence. The limited BCVA improvement should be correlated with the short follow-up period of 30 days and the inclusion criteria that allowed inclusion of eyes with chronic macular holes and/or a chronic ERM, which may limit visual improvement (Table 2).
The observation that six eyes had an unsealed macular hole may be related to the lack of postoperative positioning, size, and chronicity of the holes. The preoperative BCVA, mid-hole diameter, and base-hole diameter are correlated with anatomic success in MH surgery. The surgical prognosis is good for MHs with a mid-hole diameter from below 400 to 500 μm on OCT and base-hole less than 1,000 μm. In the current study, the macular holes persisted in six cases after vitrectomy. All patients had a macular hole larger than those values and a baseline BCVA worse than 20/400 (Tables 1 and 2). The BCVA of these patients remained unchanged despite a reduction in the diameter of macular hole.
The short follow-up period and the small number of eyes did not allow definitive conclusions about the dye. However, possible toxic effects of the dye in this series were unlikely based on the absence of deterioration in VA compared to baseline, absence of an inflammatory reaction by ophthalmic examinations, and favorable results of autofluorescence and FA.
In addition to the theoretical advantages of the use of a LZ-based dye for chromovitrectomy, three major differences were evident when the new dye was compared with the dyes currently used during chromovitrectomy. First, because the combination dye is heavier than BSS, it was deposited gently onto the posterior pole by turning off the infusion and positioning the soft-tip cannula at the center of the vitreous cavity; this avoided unnecessary aggressive maneuvers such as dye flushing into the posterior pole or an fluid–air exchange. Interestingly, the injection of the green dye into the vitreous cavity resulted in rapid deposition onto the posterior pole (Fig. 2). All surgeons except one considered that the dye was useful, and the ILM was stained greenish-blue in all eyes.
Second, the dye administration resulted in the deposit of the soluble LZ over the posterior hyaloid and within the peripheral vitreous fibers, leading to a green appearance of these structures. This resulted in easier manipulation of the posterior vitreous and the vitreous base; however, the surgeons reported that hyaloidal detachment and shaving of the vitreous base were more difficult than when using TA alone, suggesting that soluble LZ is also useful for this surgical maneuver, although less efficient than TA alone [20]. All surgeons identified the deposition of the dye in the vitreous, and 55.6 % reported intense deposition.
Third, the ability of the dye to stain the ILM resulted in easier ILM peeling in eyes with macular holes (Fig. 3). There was no evidence that intraocular lutein and zeaxanthin affected the IOP or induced an inflammatory reaction.
The lutein and zeaxanthin molecules absorb light in the visible spectrum (around 446 nm), which coincides with the blue region of the electromagnetic spectrum. For this reason, lutein and zeaxanthin may be natural absorbers of blue light, which may decrease harmful effects on the lens and retina [22]. However, this possible protective effect may be better elucidated by additional basic and clinical studies. ILM peeling guided by ICG staining currently is performed worldwide to treat macular holes, especially in the United States [20]; however, RPE atrophy may occur after ILM peeling guided by ICG staining during macular hole surgery, because of the high osmolarity of the ICG solution, decomposition of ICG, iodine effect, carbolinic complex formation, and the oxidative effect due to singlet-oxygen release from ICG after light exposure from the light pipe during PPV [23–25]. We hypothesized that the combination of lutein, zeaxanthin, and BB in one dye solution may have a good safety profile, and provides antioxidant and light-scavenging properties to protect the retina and RPE.
The study limitations were the small number of eyes, the absence of a control group, and the fact that multifocal electroretinography and microperimetry were not performed.
A more extensive evaluation of potential toxicity would probably have limited value, since alterations secondary to ILM peeling (macular manipulation) could lead to inconclusive results. In addition, the main objective of this study was to evaluate peeling of the ILM and ERM in humans during chromovitrectomy performed by different surgeons; because 18 surgeons performed the procedures, the potential for erroneous personal impressions about the staining capacity of the dyes was minimized.
In summary, the current study showed that a new dye comprised of soluble LZ 1 % and BB 0.025 % is useful for chromovitrectomy. The dye improved the intraoperative identification of the ILM similar to BB and the posterior hyaloid/vitreous base identification. Although less effective than TA, the combination solution facilitates injection of only one heavy solution into the posterior pole, and has a theoretically good safety profile. The different surgeons found that the dye might be useful for vitreoretinal surgery, with improved ILM peeling in 100 % of eyes and improved removal of the posterior hyaloid/vitreous base in 94.4 % of eyes. Additional multicenter studies are needed to confirm these findings.
References
Burk SE, Da Mata AP, Snyder ME, Rosa RH Jr, Foster RE (2000) Indocyanine green-assisted peeling of the retinal internal limiting membrane. Ophthalmology 107(11):2010–2014
Rodrigues EB, Meyer CH, Farah ME, Kroll P (2005) Intravitreal staining of the internal limiting membrane using indocyanine green in the treatment of macular holes. Ophthalmol J Int Ophtalmol Int J Ophthalmol Z Augenheilkd 219(5):251–262
Teba FA, Mohr A, Eckardt C, Wong D, Kusaka S, Joondeph BC et al (2003) Trypan blue staining in vitreoretinal surgery. Ophthalmology 110(12):2409–2412
Kumar A, Prakash G (2004) Differential staining with indocyanine green and trypan blue dye. Indian J Ophthalmol 52(4):339
Perrier M, Sebag M (2003) Epiretinal membrane surgery assisted by trypan blue. Am J Ophthalmol 135(6):909–911
Feron EJ, Veckeneer M, Parys-Van Ginderdeuren R, Van Lommel A, Melles GR, Stalmans P (2002) Trypan blue staining of epiretinal membranes in proliferative vitreoretinopathy. Arch Ophthalmol 120(2):141–144
Peyman GA, Cheema R, Conway MD, Fang T (2000) Triamcinolone acetonide as an aid to visualization of the vitreous and the posterior hyaloid during pars plana vitrectomy. Retina 20(5):554–555
Engelbrecht NE, Freeman J, Sternberg P Jr, Aaberg TM Sr, Aaberg TM Jr, Martin DF et al (2002) Retinal pigment epithelial changes after macular hole surgery with indocyanine green-assisted internal limiting membrane peeling. Am J Ophthalmol 133(1):89–94
Yemelyanov AY, Katz NB, Bernstein PS (2001) Ligand-binding characterization of xanthophyll carotenoids to solubilized membrane proteins derived from human retina. Exp Eye Res 72(4):381–392
Ahmed SS, Lott MN, Marcus DM (2005) The macular xanthophylls. Surv Ophthalmol 50(2):183–193
Nolan JSJ, Mellerio J, Godhinio M, Neelam K, Beatty S (2006) Monthly consistency of macular pigment optical density and serum concentrations of lutein and zeaxanthin. Curr Eye Res 31:199–213
Gale CHN, Phillips D, Martyn C (2001) Plasma antioxidant vitamins and carotenoids and age-related cataract. Ophthalmology 108:1992–1998
Snodderly DHG, Adler AJ (1991) Distribution of individual macular pigment carotenoids in central retina of macaque and squirrel monkeys. Invest Ophthalmol Vis Sci 32:268–279
Sommerburg OKJ, Bird A, van Kuijk F (1998) Fruits and vegetables that are sources for lutein and zeaxanthin: the macular pigment in human eyes. Br J Ophthalmol 82:907–910
Mares-Perlman JBW, Klein R et al (1995) Serum antioxidants and age-related macular degeneration in a population-based case–control study. Arch Ophthalmol 113:1518–1523
Falsini BPM, Iarossi G, Fadda A, Merendino E, Valentini P (2003) Influence of short-term antioxidant supplementation on macular function in age-related maculopathy. Ophthalmology 110:51–61
Bone RALJ, Mayne ST, Gomez CM, Tibor SE, Twaroska EE (2001) Macular pigment in donor eyes with and without AMD: a case-control study. Invest Ophthalmol Vis Sci 42:235–240
Sousa-Martins D, Maia M, Moraes M, Lima-Filho AA, Rodrigues EB, Chen J et al (2012) Use of lutein and zeaxanthin alone or combined with Brilliant Blue to identify intraocular structures intraoperatively. Retina 32(7):1328–1336
Maia M, Furlani BA, Souza-Lima AA, Martins DS, Navarro RM, Belfort R Jr (2013) LUTEIN: a new dye for chromovitrectomy. Retina.
Farah ME, Maia M, Rodrigues EB (2009) Dyes in ocular surgery: principles for use in chromovitrectomy. Am J Ophthalmol 148(3):332–340
Junghans A, Sies H, Stahl W (2001) Macular pigments lutein and zeaxanthin as blue light filters studied in liposomes. Arch Biochem Biophys 391(2):160–164
Kijlstra A, Tian Y, Kelly ER, Berendschot TT (2012) Lutein: more than just a filter for blue light. Prog Retin Eye Res 31(4):303–315
Maia M, Margalit E, Lakhanpal R, Tso MO, Grebe R, Torres G et al (2004) Effects of intravitreal indocyanine green injection in rabbits. Retina 24(1):69–79
Maia M, Haller JA, Pieramici DJ, Margalit E, De Juan E Jr, Farah ME et al (2004) Retinal pigment epithelial abnormalities after internal limiting membrane peeling guided by indocyanine green staining. Retina 24(1):157–160
Maia M, Kellner L, De Juan E Jr, Smith R, Farah ME, Margalit E et al (2004) Effects of indocyanine green injection on the retinal surface and into the subretinal space in rabbits. Retina 24(1):80–91
Acknowledgments
Many thanks to the study coordinator Luci Silva for the efforts to conclude this study.
Proprietary interest
The use of the combination of lutein/zeaxanthin and brilliant blue in human eyes is protected by international patent law (international patent number 61/468,838). The study was sponsored by Kemin Inc., Des Moines, IA, USA.
Author information
Authors and Affiliations
Corresponding author
Additional information
Clinical trial registration number: NCT01627977
Local ethics committee number: 00553212.8.0000.5505
Rights and permissions
About this article
Cite this article
Badaro, E., Furlani, B., Prazeres, J. et al. Soluble lutein in combination with brilliant blue as a new dye for chromovitrectomy. Graefes Arch Clin Exp Ophthalmol 252, 1071–1078 (2014). https://doi.org/10.1007/s00417-013-2539-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-013-2539-5