Abstract
Purpose
To evaluate the predictive value of clinical parameters, including biomechanical properties on the outcome of selective laser trabeculoplasty (SLT) in medically uncontrolled open angle glaucoma (OAG).
Methods
Sixty-eight eyes from 68 patients with OAG and IOP insufficiently regulated by topical medications were enrolled. Patients’ follow-up occurred 6 and 12 months after the procedure. The recorded parameters intraocular pressure (IOP), angle characteristics, central corneal thickness (CCT) and biomechanical properties of the eyes, including corneal hysteresis CH and corneal resistance factor CRF measured with the Ocular Responses Analyzer (ORA, Reichert Ophthalmic Instruments) were tested on their predictive value of SLT-induced IOP lowering effect using correlation analyses and regression models.
Results
Mean IOP reduction 12 months after SLT was 4.2 ± 5.7 mmHg (23.2 %, from baseline 18.1 ± 5.2 mmHg). The preoperative IOP correlated significantly with IOP reduction (maximum Spearman’s correlation r = 0.75, p < 0.001). In linear regression analysis, the corneal biomechanical properties (CH and CRF) together with the baseline IOP revealed good modelling for the IOP lowering effect of SLT (R2 = 0.64, respectively).
Conclusions
In addition to the baseline IOP biomechanical properties (CH and CRF) are significant predictors of SLT induced IOP lowering effect in medically uncontrolled OAG.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Glaucoma is the leading cause of irreversible blindness, and 70 million people are affected worldwide. However, it can be prevented by early diagnosis and treatment [1]. Pharmacological treatment strategies including reduction of aqueous humor production by topical beta receptor blockers such as timolol, or stimulation of the uveoscleral outflow by prostaglandin F2α analoga are generally accepted as first-line treatment option in open angle glaucoma. Nonetheless, for an efficient lowering of intraocular pressure (IOP), there are patients that need additional treatment (medically uncontrolled glaucoma) and there are patients for which pharmacotherapy is not applicable. The first treatment of the trabecular meshwork (TM) by laser application in patients with open angle glaucoma (OAG) was reported in 1972 by Krasnov [2]. In that context, argon laser trabeculoplasty (ALT) became the most widely used technique and has been studied intensively. Nevertheless, as an invasive procedure with a questionable repeatability and as in a significant number of ALT patients IOP increases again after a while, ALT never supplanted pharmacotherapy as primary treatment in patients with newly diagnosed OAG.
Introduced in 1995 by Park and Latina [3], selective laser trabeculoplasty (SLT) is based on the concept of selective photothermolysis. Using a 532-nm frequency-double q-switched Nd:YAG laser that delivers a low-energy, large spot, very brief pulse (3 ns) it targets selectively cells of the trabecular meshwork (TM) and therefore appears to be less invasive, compared to ALT, but results in equivalent mean IOP reduction [4, 5]. Although the exact mechanism of action for reducing the IOP is not known aqueous outflow is improved by SLT, with no or little photocoagulation-induced thermal damage [3, 6, 7]. SLT may therefore be used as first-line treatment in patients with OAG [8].
It has been reported that there is a correlation between successful SLT and age, baseline IOP and the amount of laser energy delivered, although most other clinical parameters like angle characteristics or underlying diagnosis had no predictive value [9–11].
Alterations of ocular biomechanical properties have been implicated as risk factors for development and progression of visual fields defects and optic nerve head damage in certain types OAG [12]. The Ocular Response Analyzer (ORA; Reichert Ophthalmic Instruments, Depew, NY, USA) provides measurement of corneal tissue properties including corneal hysteresis (CH) and corneal resistance factor (CRF). A decrease in CH and therefore a loss of viscous damping in the corneal tissue has been closely linked to glaucomatous optic nerve head degeneration and progression of glaucomatous visual field damage [13]. However, there is no data on biomechanical properties such as CH or CRF as potential predictive parameters regarding the outcome of SLT.
This study investigates corneal biomechanics, as predictors measured by ORA, on SLT treatment in medically uncontrolled OAG.
Patients and methods
Patients with OAG and insufficiently regulated IOP by topical medications were recruited at the glaucoma unit of the Department of Ophthalmology, Ludwig-Maximilians-University, Munich, Germany. Ethical approval of the study was obtained from the Institutional Review Board of the University Eye Hospital Munich in Germany and all the patients who agreed to participate signed a consent form. The study adheres to the tenets of the Declaration of Helsinki. Exclusion criteria were congenital, juvenile, inflammatory, or neovascular glaucoma, closed-angle glaucoma, corneal opacities interfering with angle visualization and any earlier ophthalmic surgery other than uncomplicated phacoemulsification. Patients that underwent glaucoma surgery because of uncontrolled glaucoma despite SLT during the 12-month period after the procedure were not enrolled. All study participants underwent a full ophthalmic examination, including slit-lamp biomicroscopy, IOP measurement with Goldmann applanation tonometry (GAT), gonioscopy, fundus examination by indirect ophthalmoscopy and central corneal thickness (CCT) measurement by ultrasound pachymetry. The observers taking the IOP measurements were not masked as a potential bias was supposed to be very low. Inclusion criteria were age >18 years and spherical refraction between −8.0 and +4.0 diopters. IOP measurements were performed at baseline and 1 day, 6 months and 12 months after the SLT procedure.
Classification of the irido-corneal angle
The irido-corneal angle was graded using the most detailed and recommended grading system of Spaeth [14]. The insertion of the iris root had to be on the scleral spur (C), behind the scleral spur (D) or on the ciliary band (E). In a few patients, the angle was quite narrow (B), but enough TM was visible to attempt the procedure. The curvarture of the iris was noted as steep (s), regular (r) or queer (q). The TM had to be visualized over 360° for proper application of the laser spots. The angular approach was graded between 15°–20°, 25°–30° and 35°–50°. The level of pigmentation was graded between 1+ (low pigmentation), 2+ (moderate pigmentation) and 3+ (intense pigmentation).
Visual field was assessed using the Humphrey Field Analyzer (HFA), SITA 30–2 Standard, generating the standard visual field parameters mean deviation (MD) and the pattern standard deviation (PSD). A reliable visual field test was defined as having a <25 % rate of fixation losses, and <20 % false positive and false negative.
SLT procedure
All SLT procedures were performed by one surgeon (CH). Tetracaine (0.5 %) was used for topical anaesthesia. A Latina goniolens and the Ellex (Ellex SoloTM, Adelaide, Australia) system were used to perform SLT procedures. The fixed spot size of 400 μm and pulse duration of 3 ns was implemented. Nonoverlapping spots were applied to the 360° of the TM. The initial energy level was selected by the grade of angle pigmentation with at least 0.8 mJ. Postoperative medications after SLT included flurbiprofene (0.03 %) four times a day for 3 days. Patients’ preoperative prescriptions for glaucoma were continued in the immediate phase after SLT, and then modified at follow-up visits according to their IOP measurements when necessary.
Assessment of corneal biomechanics by ORA
In addition, an ORA measurement of both eyes was conducted. The ORA determines corneal biomechanical properties using an applied force-displacement relationship. Details have been described previously [15–21]. In brief, the difference between the inward and outward motion applanation pressures is the CH and is an indication of viscous damping in the cornea. CRF is a measure of the cumulative effects of both the viscous and elastic overall resistance of the cornea. Biomechanical and pressure values recorded included CH, CRF, the corneal compensated pressure (IOPCC) and the Goldmann-equivalent pressure (IOPG). Calculations of IOP-corrected and CRF-corrected CH and CRF was conducted according to Spörl et al. [22] with references of IOP = 18 mmHg and CCT = 540 μm, taking into account that biomechanical properties of the eye are pressure-dependent [23].
Statistics
Statistical analysis was performed with the SPSS statistical software (Version 19.0, SPSS Science, Chicago, IL). Descriptive statistical analyses were performed to characterize the patients’ clinical and functional data. Visual acuity mean values were calculated after transforming the mean angle of resolution values to -logMAR (negative mean angle of resolution) values. For correlation analysis, the Spearman’s r correlation coefficient was calculated. Data were also fitted to multiple linear regression analyses to assess the predictive value of clinical and biomechanical parameters on the IOP lowering effect of SLT using absolute values of IOP reduction; t-based 95 % confidence intervals (CIs) for the regression coefficients were used. For all tests, p < 0.05 was considered to be statistically significant.
Results
A total of 68 eyes with medically uncontrolled OAG from 68 patients were included. Mean best-corrected visual acuity for the treated eye was -logMAR 0.30 +/− 0.40. The mean number of glaucoma medication was 2.38 +/− 1.10. The distribution of glaucoma diagnosis for the eyes was as follows: primary open angle glaucoma (POAG) n = 45 (66 %), normal tension glaucoma (NTG) n = 4 (6 %), pigment dispersion glaucoma (PDG), n = 4 (6 %) and pseudoexfoliative glaucoma (PEX) n = 15 (22 %). The mean number of laser applications per eye was 104 +/− 17 with a mean power of 1.28 +/− 0.32 mJ. There were no serious adverse events after the SLT procedure, e.g. IOP spikes in the immediate post-laser period. Corneal biomechanical properties measured with the ORA were obtained from all 68 eyes. All relevant data of the patients’ characteristics and clinical data are displayed in Table 1. A documentation of the angle according to the Spaeth classification was performed, angle characteristics are displayed in Table 2.
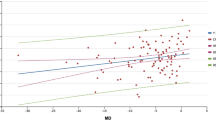
Six months after SLT the overall IOP reduction was 3.8 ± 4.4 mmHg (20.1 %, from baseline 18.1 ± 5.2 mmHg). For the subgroups, IOP reduction was 3.5 ± 4.6 mmHg (19.7 %, from baseline 17.8 ± 4.6 mmHg), 1.0 ± 4.0 mmHg (8.5 %, from baseline 11.8 ± 2.3 mmHg), −0.1 ± 5.0 mmHg (−0.6 %, from baseline 17.4 ± 4.2 mmHg), 3.1 ± 5.8 mmHg (15.5 %, from baseline 20.0 ± 5.1 mmHg) in the groups of POAG, NTG, PDG and PEX, respectively. After 12 months, the IOP lowering effect was stable in each group with an overall reduction of 4.2 ± 5.7 mmHg (23.2 %) from baseline. The difference of IOP reduction 6 and 12 months after SLT was not significant on student testing (p = 0.25). The relative IOP lowering effect in the subgroups after twelve was 24.2 %, 8.5 %, −1.7 % and 15.5 % in the POAG, NTG, PDG and PEX subgroup, respectively. In correlation analysis, the preoperative IOP correlated significantly with relative and absolute IOP reduction after 6 and 12 months (Spearman’s correlation coefficients r = −0.68 and r = −0.75, p < 0.001, respectively). The correlation of CHcorr and CRFcorr with IOP reduction after 12 months was r = −0.17 (p = 0.14) and r = −0.19 (p = 0.19). There were no significant correlations between angle characteristics or other clinical parameters and IOP reduction.
In multiple linear regression analysis, relevant clinical parameters (age, number of glaucoma medications, presence of diabetes, spherical equivalent, angle pigmentation, CCT and lens status) and biomechanical parameters (CHcorr, CRFcorr) were tested for their predictive value on the absolute IOP lowering effect of SLT. Table 3 displays the coefficients for potential predictive parameters included for prediction of IOP lowering effect 12 months after surgery with R2 = 0.61 for all included variables (model 1), which allows better modelling than the initial IOP alone (R2 = 0.56). Using a backward model to reduce the number of included parameters, beside the initial IOP the corneal biomechanical parameters and CCT remain in the model with further improvement of the predictive potency (model 2, R2 = 0.65). However, as the significance level was set at 0.05, only the baseline IOP is a significant predictor. In the model 2, for CHcorr and CRFcorr the standardized regression coefficients are still larger than 1/smaller than −1, a sign of multicollinearity indicating that the biomechanical parameters are (highly) correlated. We therefore entered the baseline IOP together with CHcorr or CRFcorr in a linear regression model. The R2 for the baseline IOP alone is 0.56 (p < 0.001). Adding CHcorr or CRFcorr to the model, the R2 increases to 0.64 with p < 0.001 for CHcorr and CRFcorr, respectively, enhancing the predictive power of baseline IOP alone for IOP lowering effect of SLT (model 3 with values for CHcorr, Table 3). CCT failed to increase the predictive power of baseline IOP (p = 0.67).
Discussion
Since its initial description by Latina and Park in 1995, SLT has proven to be safe and effective in lowering IOP in different types of OAG. When applied to previously untreated eyes, SLT may achieve a reduction of IOP of approximately 30 %, being comparable with the IOP lowering effect of prostaglandin F2α analoga [24, 25]. Even if its principle of action is yet not fully understood, SLT seems to have an enhanced safety profile compared to ALT and therefore appears to be a feasible alternative or adjunct to pharmacotherapy as primary treatment of eyes with OAG. It could be shown in previous studies, that a higher baseline IOP is predictive of a greater IOP decrease [9, 26]. In addition it has been demonstrated that the type of glaucoma has no significant influence on SLT success [27]. A recent study revealed that thinner CCT was correlated with a better IOP control [28]. Although the starting IOP was found to be predictive, one could argue that the magnitude of the potential IOP drops as the IOP becomes lower.
Our results are in consistence with these earlier findings, as well as that angle characteristics (width and pigmentation) have no predictive value [29]. The distribution of the different types of glaucoma as well as the pressure lowering effect of SLT in medically uncontrolled glaucoma is comparable to previous studies [27, 30]. However, in the four included eyes of patients with PDG, there was no IOP lowering effect of SLT.
Alterations of the biomechanical properties of the eye have been discussed as predictive factors for development and progression of OAG [12, 13]. The viscous component of the eye is supposed to play an important role in the pathogenesis of OAG as the viscosity mediates damping properties and reduces pressure peaks. The human cornea combines elastic and viscous properties and the viscosity of the cornea is in good correlation with the viscosity of the sclera. Therefore, corneal hysteresis (CH), as measured by ORA, may be related to the distensibility of the optic nerve complex [31]. However, there is only very limited knowledge on how these biomechanical parameters are affected by laser treatment of the trabecular meshwork, such as SLT. In our study, biomechanical properties revealed good modelling for the IOP lowering effect of SLT in linear regression in addition to baseline IOP. It can be suggested that the obtained predictive parameters are to some extend pressure related or influence the measurement of IOP. However, using IOP-corrected biomechanical parameters as recommended [22, 23] minimizes that potential source of error.
In accordance with a previous study, other clinical parameters like lens status or presence of diabetes could not predict the IOP lowering effect of SLT [29]. We did not observe a significant predictive value of the CCT as reported previously, but in the model 2 the CCT remained in the model with a p-value of 0.09. Therefore, a mild influence of CCT can also be suggested by our data. The predictive value of biomechanical properties of the eye leads to the suggestion, that corneal (and scleral) biomechanical properties as measured with the ORA are also reflected in the TM. An association between the biomechanical characteristics of the eye shell and intraocular tissue of the anterior segment is therefore very likely. As the targeted tissue in SLT is the TM, and there is a positive prediction of biomechanical properties on the IOP lowering effect of SLT, the biomechanical properties of the eye shell are to some extend correlated with characteristics of the TM. Corneal stroma, sclera and the major amount of the iris are originally derived from mesenchymal tissue in embryogenesis, which might be an explanation for the predictive impact. First results of direct measurements of biomechanical properties of the TM using atomic force microscopy reveal a significant difference in the elastic modulus of glaucomatous eyes [32].
A limitation of our study is that SLT was performed in medically uncontrolled glaucoma, as the study was performed at a tertiary university-affiliated glaucoma clinic. Therefore, a transfer of our results to use biomechanical parameters to predict success in treatment naive or medically controlled glaucoma patients, in whom SLT could substitute the local therapy, might not be applicable. Another limitation is that in this investigation we did not test on absolute success of SLT in uncontrolled OAG by defining a success criterion (e.g., minimum IOP reduction of 20 % and absolute IOP lower than 21 mmHg). However, we believe that success has to be defined individually for every single patient, and therefore we decided to test on absolute IOP reduction.
To date, the ORA is the only FDA approved instrument to display biomechanical properties of the eye in vivo, and a relatively high variability of repeated measurement is well-known [22]. With new technologies more precise and reliable measurements will better display the biomechanical characteristics in vivo and allow to better understand the pathophysiological processes of glaucoma. An instrument that generates in vivo measurements of the elastic tissue properties like Young's modulus would be eligible [33].
However, our finding that biomechanical properties, beside the initial IOP, are predictive for the outcome of SLT in medically uncontrolled OAG may provide an additional criterion helping better to decide for the individual patient: is the attempt of laser treatment with SLT is justified, should pharmacotherapy be intensified, or should the patient preferably undergo glaucoma surgery.
References
Quigley HA, Broman AT (2006) The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 90:262–267
Krasnov M (1972) Laser puncture of the anterior chamber angle in glaucoma (a preliminary report) [in Russian]. Vestn Oftalmol 3:27–31.
Latina MA, Park C (1995) Selective targeting of trabecular meshwork cells: in vitro studies of pulsed and CW laser interactions. Exp Eye Res 60:359–371
Bovell AM, Damji KF, Hodge WG, Rock WJ, Buhrmann RR, Pan YI (2011) Long term effects on the lowering of intraocular pressure: selective laser or argon laser trabeculoplasty? Can J Ophthalmol 46:408–413
Liu Y, Birt CM (2012) Argon versus selective laser trabeculoplasty in younger patients: 2-year results. J Glaucoma 21:112–115
Kramer TR, Noecker RJ (2001) Comparison of the morphologic changes after selective laser trabeculoplasty and argon laser trabeculoplasty in human eye bank eyes. Ophthalmology 10:773–779
Samples JR, Singh K, Lin SC, Francis BA, Hodapp E, Jampel HD, Smith SD (2011) Laser trabeculoplasty for open-angle Glaucoma A report by the american academy of ophthalmology. Ophthalmology 118:2296–2302
Katz LJ, Steinmann WC, Kabir A, Molineaux J, Wizov SS, Marcellino G (2012) Selective laser trabeculoplasty versus medical therapy as initial treatment of glaucoma: a prospective, randomized trial. J Glaucoma 21:460–468
Ayala M, Chen E (2011) Predictive factors of success in selective laser trabeculoplasty (SLT) treatment. Clin Ophthalmol 5:573–576
Tzimis V, Tze L, Ganesh J, Muhsen S, Kiss A, Kranemann C, Birt CM (2011) Laser trabeculoplasty: an investigation into factors that might influence outcomes. Can J Ophthalmol 46:305–309
Bruen R, Lesk MR, Harasymowycz P (2012) Baseline factors predictive of SLT response: a prospective study. J Ophthalmol 2012:642869
De Moraes CV, Hill V, Tello C, Liebmann JM, Ritch R (2012) Lower corneal hysteresis is associated with more rapid glaucomatous visual field progression. J Glaucoma 21:209–213
Abitbol O, Bouden J, Doan S, Hoang-Xuan T, Gatinel D (2010) Corneal hysteresis measured with the Ocular Response Analyzer in normal and glaucomatous eyes. Acta Ophthalmol 88:116–119
Spaeth GL (1971) The normal development of the human anterior chamber angle: a new system of descriptive grading. Trans Ophthalmol Soc U K 91:709–739
Luce DA (2005) Determining in vivo biomechanical properties of the cornea with an ocular response analyzer. J Cataract Refract Surg 31:156–162
Sullivan-Mee M, Billingsley SC, Patel AD, Halverson KD, Alldredge BR, Qualls C (2008) Ocular Response Analyzer in subjects with and without glaucoma. Optom Vis Sci 85:463–470
Kirwan C, O’Malley D, O’Keefe M (2008) Corneal hysteresis and corneal resistance factor in keratoectasia: findings using the Reichert ocular response analyzer. Ophthalmologica 222:334–337
Carbonaro F, Andrew T, Mackey DA, Spector TD, Hammond CJ (2008) The heritability of corneal hysteresis and ocular pulse amplitude: a twin study. Ophthalmology 115:1545–1549
Shah S, Laiquzzaman M, Bhojwani R, Mantry S, Cunliffe I (2007) Assessment of the biomechanical properties of the cornea with the ocular response analyzer in normal and keratoconic eyes. Invest Ophthalmol Vis Sci 48:3026–3031
Ortiz D, Pinero D, Shabayek MH, Arnalich-Montiel F, Alio JL (2007) Corneal biomechanical properties in normal, post-laser in situ keratomileusis, and keratoconic eyes. J Cataract Refract Surg 33:1371–1375
Kirwan C, O’Keefe M, Lanigan B (2006) Corneal hysteresis and intraocular pressure measurement in children using the reichert ocular response analyzer. Am J Ophthalmol 142:990–992
Sporl E, Terai N, Haustein M, Bohm AG, Raiskup-Wolf F, Pillunat LE (2009) Biomechanical condition of the cornea as a new indicator for pathological and structural changes. Ophthalmologe 106:512–520
Hirneiss C, Neubauer AS, Yu A, Kampik A, Kernt M (2011) Corneal biomechanics measured with the ocular response analyser in patients with unilateral open-angle glaucoma. Acta Ophthalmol 2011(89):e189–e192
Prasad N, Murthy S, Dagianis JJ, Latina MA (2009) A comparison of the intervisit intraocular pressure fluctuation after 180 and 360 degrees of selective laser trabeculoplasty (SLT) as a primary therapy in primary open angle glaucoma and ocular hypertension. J Glaucoma 18:157–160
Nagar M, Luhishi E, Shah N (2009) Intraocular pressure control and fluctuation: the effect of treatment with selective laser trabeculoplasty. Br J Ophthalmol 93:497–501
Hodge WG, Damji KF, Rock W, Buhrmann R, Bovell AM, Pan Y (2005) Baseline IOP predicts selective laser trabeculoplasty success at 1 year post-treatment: results from a randomised clinical trial. Br J Ophthalmol 89:1157–1160
Koucheki B, Hashemi H (2012) Selective laser trabeculoplasty in the treatment of open-angle glaucoma. J Glaucoma 21:65–70
Shazly TA, Latina MA, Dagianis JJ, Chitturi S (2012) Effect of central corneal thickness on the long-term outcome of selective laser trabeculoplasty as primary treatment for ocular hypertension. Cornea 31:883–886
Martow E, Hutnik CM, Mao A (2011) SLT and adjunctive medical therapy: a prediction rule analysis. J Glaucoma 20:266–270
Hirn C, Zweifel SA, Toteberg-Harms M, Funk J (2012) Effectiveness of selective laser trabeculoplasty in patients with insufficient control of intraocular pressure despite maximum tolerated medical therapy. Ophthalmologe 109:683–690
Wells AP, Garway-Heath DF, Poostchi A, Wong T, Chan KC, Sachdev N (2008) Corneal hysteresis but not corneal thickness correlates with optic nerve surface compliance in glaucoma patients. Invest Ophthalmol Vis Sci 49:3262–3268
Last JA, Pan T, Ding Y, Reilly CM, Keller K, Acott TS, Fautsch MP, Murphy CJ, Russell P (2011) Elastic modulus determination of normal and glaucomatous human trabecular meshwork. Invest Ophthalmol Vis Sci 52:2147–2152
Liu J, Roberts CJ (2005) Influence of corneal biomechanical properties on intraocular pressure measurement: quantitative analysis. J Cataract Refract Surg 31:146–155
Conflict of interest
No authors have any conflict of interest related to this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hirneiß, C., Sekura, K., Brandlhuber, U. et al. Corneal biomechanics predict the outcome of selective laser trabeculoplasty in medically uncontrolled glaucoma. Graefes Arch Clin Exp Ophthalmol 251, 2383–2388 (2013). https://doi.org/10.1007/s00417-013-2416-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-013-2416-2