Abstract
Background
To evaluate the intraocular lens (IOL) position by analyzing the postoperative axis of internal astigmatism as well as the higher-order aberration (HOA) profile after cataract surgery following the implantation of a diffractive multifocal toric IOL
Methods
Prospective study including 51 eyes with corneal astigmatism of 1.25D or higher of 29 patients with ages ranging between 20 and 61 years old. All cases underwent uneventful cataract surgery with implantation of the AT LISA 909 M toric IOL (Zeiss). Visual, refractive and corneal topograpy changes were evaluated during a 12-month follow-up. In addition, the axis of internal astigmatism as well as ocular, corneal, and internal HOA (5-mm pupil) were evaluated postoperatively by means of an integrated aberrometer (OPD Scan II, Nidek).
Results
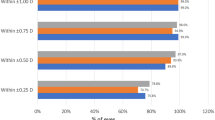
A significant improvement in uncorrected distance and near visual acuities (p < 0.01) was found, which was consistent with a significant correction of manifest astigmatism (p < 0.01). No significant changes were observed in corneal astigmatism (p = 0.32). With regard to IOL alignment, the difference between the axes of postoperative internal and preoperative corneal astigmatisms was close to perpendicularity (12 months, 87.16° ± 7.14), without significant changes during the first 6 months (p ≥ 0.46). Small but significant changes were detected afterwards (p = 0.01). Additionally, this angular difference correlated with the postoperative magnitude of manifest cylinder (r = 0.31, p = 0.03). Minimal contribution of intraocular optics to the global magnitude of HOA was observed.
Conclusions
The diffractive multifocal toric IOL evaluated is able to provide a predictable astigmatic correction with apparent excellent levels of optical quality during the first year after implantation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Toric intraocular lenses (IOLs) have been shown to be very effective for the compensation of the preexisting corneal astigmatim in eyes undergoing cataract surgery [1–9]. However, these IOLs are only able to improve distance visual acuity, with spectacle dependence for near vision. A new model of diffractive multifocal IOL with toric component was introduced to compensate for any degree of corneal astigmatim as well as to allow spectacle independence, the AT LISA toric 909M. This IOL has been shown to provide excellent compensation of astigmatism as well as far and near visual rehabilitation simultaneously [10, 11]. In addition, it can be implanted through small incision, providing better control of postoperative surgically induced astigmatism (SIA) [11] and theoretically of higher-order aberrations (HOAs). However, to this date, there are no reports evaluating the intraocular optical quality and aberrations induced with the implantation of this new modality of toric diffractive IOL.
The achievement of a perfect astigmatic correction with this and other types of toric IOLs requires a precise intraocular alignment and long-term rotational stability and centration. Toric IOL position can be evaluated using either subjective or objective methods [6, 8, 12–19]. Each technique has its own limitations such as head position and cyclotorsion during measurements, or the need for experienced staff to work with sophisticated software and equipment. One of these methods for assessing axis alignment and IOL rotation is the analysis of internal astigmatism by means of an integrated aberrometer combining a corneal and ocular aberrometer [20–22], which is an easy procedure for clinical use. Specifically, it consists of the analysis of the internal aberration map which displays the refractive status of the internal optics of the eye, including the posterior cornea and the IOL optics.
The aim of the current study was to evaluate the intraocular lens (IOL) position by analyzing the postoperative axis of internal astigmatism as well as the higher-order aberration profile after cataract surgery following the implantation of an acrylic plate haptic diffractive multifocal toric IOL using an advanced integrated aberrometer.
Methods
Patients
In this study, 51 eyes of 29 patients with ages ranging between 20 and 61 years old were included. The inclusion criteria of this study were patients with visually significant cataract or presbyopic/pre-presbyopic patients suitable for refractive lens exchange demanding complete spectacle-independence, and with corneal astigmatisms of 1.25D or higher. The exclusion criteria were patients with history of glaucoma or retinal detachment, corneal disease, irregular corneal astigmatism, abnormal iris, macular degeneration or retinopathy, neurophthalmic disease, or history of ocular inflammation. This study was approved by the local ethics committee, and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. Written informed consent was obtained after explaining the nature of the procedure prior to surgery in all cases.
Preoperative and postoperative protocol
Preoperatively, all patients had a full ophthalmologic examination including the following clinical tests: uncorrected (UDVA) and corrected distance (CDVA) visual acuities (Snellen charts), uncorrected (UNVA) and corrected near (CNVA) visual acuities (Radner charts), manifest refraction, slit-lamp examination, Goldmann applanation tonometry, corneal topography (Atlas 9000, Carl Zeiss Meditec), biometry (IOL Master v.4.3, Carl Zeiss Meditec), and funduscopy. Patients were evaluated postoperatively at 1 day, 1 month, and 3, 6, and 12 months after surgery. At 1 day after surgery, only UDVA, tonometry, and the integrity of the anterior segment was evaluated. The postoperative examination protocol at 1, 3, 6, and 12 months was identical to the preoperative protocol, with the additional measurement of the axis of internal astigmatism and optical aberrations with the OPD Scan II system (Nidek) under pharmacological dilation (tropicamide). The axis alignment of internal astigmatism was read from the 3-mm central zone of the postoperative internal OPD map, and compared with the preoperative axis of corneal astigmatism. Misalignment of the IOL was defined as the mean difference between the axis of the internal astigmatism and the preoperative orientation of the steepest corneal meridian. Root-mean square (RMS) values of total aberrations, higher order (HOAs), tilt, primary coma, trefoil, tetrafoil, primary spherical aberration, and secondary astigmatism were calculated for the corneal, internal and ocular optics (5-mm pupil).
Surgery
All surgeries were performed by the same experienced surgeon (PM) using a standard technique of sutureless micro-coaxial phacoemulsification. In all cases, instillation of topical anaesthesia drops was applied to the patient prior to the surgical procedure. Adequate dilation was obtained with intracameral mydriasis. In all cases, mini-incision surgery was performed (2.2 mm temporal corneal incision), with the incision placed on the steepest corneal meridian determined by corneal topography. Before starting surgery, in supine position, three limbal reference marks at 3, 6 and 9 o’clock positions were done with a sterile marker with the aim of avoiding possible cyclorotations during surgery. After capsulorhexis creation and phacoemulsification (Infinity Vision System, Alcon), the IOL was inserted into the capsular bag using the AT.Smart Cartridge Set (Carl Zeiss Meditec) and the AT.Shooter A2-2000 injector (Carl Zeiss Meditec) through the incision. Postoperative topical therapy included a combination of topical antibiotic and steroid.
Statistical analysis
The statistical analysis was performed using the SPSS statistics software package version 15.0 for Windows (SPSS, Chicago, IL, USA). First of all, normality of all data samples was evaluated by means of the Kolmogorov–Smirnov test. When parametric analysis was possible, the Student's t-test for paired data was performed for all parameter comparisons between preoperative and postoperative examinations, and the 1-way analysis of variance (ANOVA) with Bonferroni post-hoc comparison procedure was used for the comparison between groups. When parametric analysis was not possible, the Wilcoxon rank sum test was applied to assess the significance of differences between preoperative and postoperative data, whereas the Kruskal–Wallis test was used to compare the analyzed parameters between groups. For post-hoc analysis, the Mann–Whitney test with Bonferroni’s adjustment was used in order to avoid the experimental error rate in these cases. For all statistical tests, the same level of significance was used (p < 0.05). Correlation coefficients (Pearson or Spearman depending on whether normality condition could be assumed) were used to assess the correlation between different clinical and optical quality parameters.
Results
Mean age of patients included in this prospective study was 47.5 years (standard deviation, SD: 9.6; range: 20 to 61 years). IOL implantation was performed in a total of 27 right eyes (52.94 %) and 24 left eyes (47.06 %), with only seven cases of unilateral implantation (24.14 %). Regarding the gender distribution, 12 patients were male (41.38 %) and 17 female (58.62 %). Preoperatively, mean axial length was 23.21 mm (SD: 2.14; range: 19.23 to 28.52) and mean anterior chamber depth was 3.25 mm (SD: 0.41; range: 2.52 to 4.26). Mean IOL spherical power implanted was 20.12 D (SD: 8.00; range: 3.50 to 35.5) and mean IOL cylindrical power was 3.01 D (SD: 1.50; range: 1.50 to 8.50).
Visual and refractive outcomes
Table 1 summarizes the preoperative and postoperative outcomes of the current series. As shown, a statistically significant improvement in UDVA of around 5 LogMAR lines was found on average postoperatively (p < 0.01). This visual change was consistent with a significant postoperative reduction of manifest cylinder in absolute terms (p < 0.01). A significant postoperative improvement was also found in CDVA (p < 0.01) as well as in UNVA (p < 0.01) and CNVA (p < 0.01) (Table 1).
Corneal topographic changes
Small in magnitude but statistically significant changes were detected in the keratometric readings after surgery (p < 0.01), as shown in Table 2. However, the magnitude of corneal astigmatism was not modified significantly with surgery (p = 0.32) (Table 2).
Aberrometric outcomes
No statistically significant differences were found in the magnitude of tilt, higher order, primary coma, and secondary astigmatism RMS between corneal, internal, and ocular measurements (p ≥ 0.17) (Table 3). In contrast, significant differences were found in the magnitude of total, trefoil, and tetrafoil RMS, as well as in the magnitude of primary spherical aberration (p ≤ 0.02). Ocular total RMS was significantly lower than that corresponding to corneal and internal optics (p < 0.01). However, ocular trefoil RMS was significantly higher than corneal (p = 0.02) and internal values (p = 0.02). Regarding corneal primary spherical aberration, it was significantly more positive than the internal (p < 0.01) and ocular (p < 0.01) values. Furthermore, the internal tetrafoil RMS was significantly higher than the ocular RMS associated to this aberration (p = 0.03).
Comparison of axis of internal and corneal astigmatism
Figure 1 shows in a scatterplot the relationship between the 12-month postoperative axis of internal astigmatism (3-mm pupil) and the preoperative axis of corneal astigmatism. As shown, both axes were close to perpendicularity in almost all cases, with a mean absolute angle between them of 87.16° (SD: 7.14; range: 67° to 103°). No significant correlations of this mean absolute angle with any ocular aberrometric parameter were obtained (−0.04≤ r ≤0.26, p ≥ 0.26). No significant correlations of the mean absolute angle between axes of corneal and internal astigmatism with postperative visual and refractive data were found (−0.08≤ r ≤0.26, p ≥ 0.17), except for the postoperative cylinder (r = 0.31, p = 0.03) (Fig. 2). All these same trends were also observed in the remaining postoperative visits (1 month, mean: 88.29°, SD: 7.43°, range: 67° to 102°; 3 months, mean: 88.24°, SD: 6.85°, range: 67° to 101°; 6 months, mean: 88.12°, SD: 6.70°, range: 67° to 101°). No significant differences between consecutive postoperative visits were found in this parameter during the first 6 months of the follow-up (1–3 months, p = 0.93; 3–6 months, p = 0.46). However, a small but significant change was detected at 12 months (6–12 months, p = 0.01). Mean misalignment was 5.98° (SD: 4.65; range: 0° to 23°), 5.33° (SD: 4.60; range: 0° to 23°), 5.25° (SD: 4.51; range: 0° to 23°), and 5.98° (SD: 4.76; range: 0° to 23°). Difference in this parameter between consecutive measurements reached statistical significance at 3 (p = 0.02) and 12 months (p = 0.04).
Discussion
In the current series, a statistically significant improvement in UDVA of approximately 5 logMAR lines was found, which confirms the efficacy of this IOL for the correction of corneal cylinder after cataract extraction in eyes with moderate to high astigmatism. This finding was consistent with the distance visual improvement reported by other authors using other modalities of toric IOLs [1–9, 12] as well as using the same IOL model [10, 11]. As expected, this significant improvement in UDVA was combined with a significant reduction in manifest cylinder. The significant decrease in refractive cylinder found in the current series was consistent with those reported by other authors evaluating other modalities of toric IOLs [1–9, 12]. With regard to near vision, a significant improvement in UNVA was found as well, with a final postoperative visual outcome very similar to that reported in previous series using the same toric multifocal IOL [10, 11]. In addition, mean UNVA was around J1, an excellent outcome comparable to the result obtained with the last generation of multifocal IOLs [23, 24]. As the aberrometric and scattering effect of the cataractous crystalline lens of most of the cases was eliminated, a significant improvement in CDVA and CNVA was also detected.
In the current study, mini-incision surgery (2.2 mm) was performed for the implantation of the toric multifocal IOL selected. This allowed the surgeon to reduce the surgical trauma and to minimize the surgically induced astigmatism, as in a previous series [11]. Indeed, no statistically significant changes after surgery were detected in corneal astigmatism in the current series. This is a factor that contributed clearly to the predictable astigmatic correction obtained with the evaluated IOL. A significant change was only observed in keratometric readings, but small in magnitude, not clinically relevant, and unable to induce significant changes in corneal toricity. It should be considered that both micro (sub-1.8 mm) and mini-incision phacoemulsification have been shown not to degrade the optical quality of the cornea [25].
With regard to the analysis of aberrations, no significant differences were found in the magnitude of tilt, higher order, primary coma, and secondary astigmatism RMS between corneal, internal and ocular measurements. Specifically, a minimal contribution of the intraocular optics to the global magnitude of these types of higher-order aberrations was observed. Furthermore, the magnitude of internal spherical aberration was very close to zero, and significantly lower than that for the corneal and total ocular optics. Two factors may have accounted for such a finding: the use of an aspheric curve for both IOL surfaces minimizing the induction of this type of aberration, and a potential IOL neutralization effect of the minimal spherical aberration arising from the posterior corneal surface [26]. The internal optics were also found to contribute to the induction of ocular trefoil and to the reduction of ocular tetrafoil. This might be in relation with specific optical properties of the evaluated IOL. More studies evaluating in detail the optical performance of the evaluated multifocal toric IOL should be performed in the future. In any case, the internal aberrometric analysis shown in the current study should be considered with caution, because the accuracy of wavefront aberration measurements have been demonstrated to be limited in some eyes implanted with diffractive bifocal and multifocal IOLs [27]. Indeed, a more significant aberrometric component may be expected with the evaluated IOL due to its diffractive component. However, we have found lower amounts of primary spherical aberration than those reported for eyes implanted with monofocal IOLs [24]. Possibly, the Hartmann–Shack aberrometer of the OPD-Scan II system is unable to detect the highest order aberrations induced by the diffractive components of the toric multifocal IOL. On the other hand, it should be also considered that the aberrometer used did not provide a quantification of the forward scattering, whose magnitude may be relevant with a diffractive multifocal IOL. One potential drawback of the current study is the absence of preoperative aberrometric measurements and therefore the absence of a comparative statistical analysis of the significance of the change between preoperative and postoperative visits. In any case, it should be considered that a large variability in the preoperative levels of higher order aberrations would have been observed because patients with visually significant cataract and therefore potentially large levels of higher-order aberrations, as well as presbyopic/pre-presbyopic patients suitable for refractive lens exchange with potentially no significantly altered aberrometric pattern, were included.
The axis of internal astigmatism was found to be perpendicular or almost perpendicular to the axis of corneal cylinder in the great majority of cases and during all follow-up. This condition of orthogonality of both axes is indispensable for an efficacious astigmatic correction. Therefore, the analysis of internal astigmatism axis in the analyzed sample is consistent with an appropriately implanted and positioned toric IOL. Only a minimal but statistically significant loss of the orthoganility between internal and corneal astigmatic axes is observed at the end of the follow-up, possibly due to capsular bag changes affecting IOL position. A significant although limited correlation was found between the postoperative cylinder and the difference in degrees between corneal and internal axes. Specifically, the closer this difference to 90°, the lower was the magnitude of the postoperative cylinder, as could be expected. Therefore, misalignments of the astigmatic correction were able to induce a non-efficacious correction of the pre-existing corneal astigmatism in some specific cases. Viestenz et al. [14]. estimated that 11.5° of toric IOL rotation would lead to residual astigmatism, that is 40 % of the initial astigmatic power and 3°, 10 % of the initial power. In terms of misalignment, we found in the current series a mean value at the end of follow-up of 5.98°. This value was consistent with the mean absolute angle of error (AE) calculated using the Alpins vector analysis and reported in a previous study on the same toric multifocal IOL (mean: 5.76°, SD: 10.09; range, 0° to 76°). Likewise, our misalignment was similar to that reported for other toric IOLs using the same device and procedure to estimate it, the analysis of the axis of the internal astigmatism with the OPD-Scan II [22].
In summary, the AT LISA 909M toric IOL provides a restoration of visual acuity at far and near distances in the eyes with corneal astigmatism and undergoing cataract surgery during the first year after implantation. This is achieved by means a predictable astigmatic correction with apparent excellent levels of optical quality. The analysis of the internal astigmatism by means of an integrated aberrometer (corneal + ocular aberrometry) confirms the ability of this IOL to provide a predictable astigmatic correction and the stability of this implant into the capsular bag, with a limited misalignment. This positional stability is a key factor leading to a complete correction of astigmatim with this type of implant. More studies evaluating the intraocular optics in eyes implanted with this modality of toric multifocal IOL with other optical methodologies should be conducted to confirm our outcomes. An integrated aberrometer seems to be a useful and recommendable tool for evaluating the outcomes obtained with a toric IOL and understanding the cause of a non-efficacious astigmatic correction. Furthermore, this type of devices can be useful to guide the surgeon for a proper replacement of a toric IOL in case of a previous unsuccessful outcome.
References
Holland E, Lane S, Horn JD, Ernest P, Arleo R, Miller KM (2010) The AcrySof toric intraocular lens in subjects with cataracts and corneal astigmatism; a randomized, subject-masked, parallel-group, 1-year study. Ophthalmology 117:2104–2111
Alió JL, Agdeppa MCC, Pongo VC, El Kady B (2010) Microincision cataract surgery with toric intraocular lens implantation for correcting moderate and high astigmatism: pilot study. J Cataract Refract Surg 36:44–52
Mendicute J, Irigoyen C, Ruiz M, Illarramendi I, Ferrer-Blasco T, Montés-Micó R (2009) Toric intraocular lens versus opposite clear corneal incisions to correct astigmatism in eyes having cataract surgery. J Cataract Refract Surg 35:451–458
Bauer NJC, de Vries NE, Webers CAB, Hendrikse F, Nuijts RMMA (2008) Astigmatism management in cataract surgery with the AcrySof toric intraocular lens. J Cataract Refract Surg 34:1483–1488
Mendicute J, Irigoyen C, Aramberri J, Ondarra A, Montés-Micó R (2008) Foldable toric intraocular lens for astigmatism correction in cataract patients. J Cataract Refract Surg 34:601–607
De Silva DJ, Ramkissoon YD, Bloom PA (2006) Evaluation of a toric intraocular lens with a Z-haptic. J Cataract Refract Surg 32:1492–1498
Till JS, Yoder PR, Wilcox TK, Spielman JL (2002) Toric intraocular lens implantation: 100 consecutive cases. J Cataract Refract Surg 28:295–301
Ruhswurm I, Scholz U, Zehetmayer M, Hanselmayer G, Vass C, Skorpik C (2000) Astigmatism correction with a foldable toric intraocular lens in cataract patients. J Cataract Refract Surg 26:1022–1027
Alió JL, Piñero DP, Tomás J, Alesón A (2011) Vector analysis of astigmatic changes after cataract surgery with toric intraocular lens implantation. J Cataract Refract Surg 37:1038–1049
Alió JL, Piñero DP, Tomás J, Plaza-Puche AB (2011) Vector analysis of astigmatic changes after cataract surgery with implantation of a new toric multifocal intraocular lens. J Cataract Refract Surg 37:1217–1229
Mojzis P, Piñero DP, Studeny P, Tomás J, Korda V, Plaza-Puche AB, Alió JL (2011) Comparative analysis of clinical outcomes obtained with a new diffractive multifocal toric intraocular lens implanted through two types of corneal incisions. J Refract Surg 27:648–657
Chang FD (2008) Comparative rotational stability of single-piece open-loop acrylic and plate-haptic silicone toric intraocular lenses. J Cataract Refract Surg 34:1842–1847
Prinz A, Neumayer T, Bueh W, Vock L, Menapace R, Findl O, Georgopoulos M (2011) Rotational stability and posterior capsule opacification of a plate-haptic and an open-loop-haptic intraocular lens. J Cataract Refract Surg 37:251–257
Viestenz A, Seitz B, Langenbucher A (2005) Evaluating the eye's rotational stability during standard photography; effect on determining the axial orientation of toric intraocular lenses. J Cataract Refract Surg 31:557–561
Chang DF (2003) Early rotational stability of the longer Staar toric intraocular lens; fifty consecutive cases. J Cataract Refract Surg 29:935–940
Nguyen TM, Miller KM (2000) Digital overlay technique for documenting toric intraocular lens axis orientation. J Cataract Refract Surg 26:1496–1504
Weinand F, Jung A, Stein A, Pfützner A, Becker R, Pavlovic S (2007) Rotational stability of a single-piece hydrophobic acrylic intraocular lens: new method for high-precision rotation control. J Cataract Refract Surg 33:800–803
Shah GD, Praveen MR, Vasavada AR, Rampal NV, Vasavada VA, Asnani PK, Pandita D (2009) Software-based assessment of postoperative rotation of toric intraocular lens. J Cataract Refract Surg 35:413–418
Wolffsohn JS, Buckhurst PJ (2010) Objective analysis of toric intraocular lens rotation and centration. J Cataract Refract Surg 36:778–782
Gualdi L, Cappello V, Giordano C (2009) The use of Nidek OPD Scan II wavefront aberrometry in toric intraocular lens implantation. J Refract Surg 25(suppl 1):S110–S115
Ligabue EA, Giordano C (2009) Assessing visual quality with the point spread function using the Nidek OPD Scan II. J Refract Surg 25(suppl 1):S104–S109
Carey PJ, Leccisotti A, McGilligan VE, Goodall EA, Moore CB (2010) Assessment of toric intraocular lens alignment by a refractive power/corneal analyzer system and slitlamp observation. J Cataract Refract Surg 36:222–229
Ramón ML, Piñero DP, Pérez-Cambrodí RJ (2012) Correlation between visual performance, quality of life and intraocular aberrometric profile in patients implanted with rotationally asymmetric multifocal intraocular lenses. J Refract Surg 28:93–99
Alió JL, Piñero DP, Plaza-Puche AB, Amparo F, Jiménez R, Rodríguez-Prats JL, Javaloy J (2011) Visual and optical performance with two different diffractive multifocal intraocular lenses compared to a monofocal lens. J Refract Surg 27:570–581
Alió JL, Elkady B, Ortiz D (2010) Corneal optical quality following sub 1.8 mm micro-incision cataract surgery vs 2.2 mm mini-incision coaxial phacoemulsification. Middle East Afr J Ophthalmol 17:94–99
Sicam VA, Dubbelman M, Van de Heijde RG (2006) Spherical aberration of the anterior and posterior surfaces of the human cornea. J Opt Soc Am A Opt Image Sci Vis 23:544–549
Charman WN, Montés-Micó R, Radhakrishnan H (2008) Problems in the measurement of wavefront aberration for eyes implanted with diffractive bifocal and multifocal intraocular lenses. J Refract Surg 24:280–286
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no financial or proprietary interest in any product, method, or material described herein.
All the authors have full control of all primary data, and they agree to allow Graefe’s Archive for Clinical and Experimental Ophthalmology to review the data of the current study if requested.
Rights and permissions
About this article
Cite this article
Mojzis, P., Piñero, D.P., Ctvrteckova, V. et al. Analysis of internal astigmatism and higher order aberrations in eyes implanted with a new diffractive multifocal toric intraocular lens. Graefes Arch Clin Exp Ophthalmol 251, 341–348 (2013). https://doi.org/10.1007/s00417-012-2061-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-012-2061-1