Abstract
Background
To determine whether there is a significant correlation between the pulse-wave analysis in the optic nerve head circulation determined by laser speckle flowgraphy (LSFG), and brachial–ankle pulse wave velocity (baPVW), carotid intima–media thickness (IMT), and age.
Methods
Thirty-three patients who visited the Vascular Function Section in our hospital were included. Age was 57.3 ± 12.6 years, with a range from 29 to 80 years. baPVW, carotid IMT, and pulse wave analysis in optic nerve head circulation using LSFG were conducted on subjects, and this parameter is named blowout time (BOT). The following items were analyzed as other systemic parameters: age, blood pressure, pulse pressure, heart rate, body mass index, and mean arterial blood pressure; other ocular parameters were intraocular pressure and ocular perfusion pressure. Pearson’s correlation coefficients were used to determine the relationship between the BOT, baPWV, IMT, age, and other parameters. In addition, multiple regression analysis was used to determine independent factors for age.
Results
BOT was significantly correlated with age (r = −0.85, P <0.0001), pulse pressure (r = −0.36, P = 0.04), baPWV (r = −0.72, P <0.0001), and IMT (r = −0.64, P < 0.0001). The result of multiple regression analysis showed that baPWV (odds ratio = 0.93, 95% confidence interval = 0.03–1.82 P = 0.04) and BOT (−2.26, −3.27 to −1.26, <0.0001) were independent contribution factors to age.
Conclusions
Our results confirmed measurements of BOT in the optic nerve head can be a useful method for determinin g whether early atherosclerotic changes are present in the optic nerve head circulation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Aging is significantly associated with the development of atherosclerosis, and is a major risk factor for cardiovascular diseases [1]. In the eye, aging is a risk factor for retinal vascular diseases, e.g., retinal vein occlusion [2–4] and age-related degeneration [5, 6]. The pulse-wave velocity (PWV) and carotid intima–media thickness (IMT) are important markers of atherosclerosis. A significant correlation has also been reported between the PWV and retinal vein occlusion and age-related macular degeneration [7, 8]. Significant correlations have also been found between IMT of the carotid artery and age-related macular degeneration [9]. PWV is an indicator of arterial stiffness [10, 11], and a simple method has recently developed of measuring the brachial–ankle PWV (baPWV) [12, 13].
It has been reported that the IMT of the carotid artery is useful for determining coronary artery atherosclerosis [14], and the IMT is highly correlated with the presence and extent of coronary artery disease [15, 16]. The values of the baPWV and increasing thickness of IMT are age-related [17, 18]. Therefore, it was suggested that evaluations of the relationships between ocular circulation, IMT, baPWV, and age are important.
Laser speckle flowgraphy (LSFG; Kyushu Institute of Technology, Fukuoka, Japan) is a method of determining ocular blood flow, and it is based on the changes in the speckle pattern of laser light reflected from the eye [19, 20]. LSFG is dependent on the movement of erythrocytes in the retina and choroid [21], and can thus measure the relative velocity of the erythrocytes mean blur rate (MBR). The changing of MBR has a pulse-wave pattern tuned to the cardiac cycle.
The purpose of this study was to determine whether there is a significant correlation between the pulse wave in the optic nerve head circulation determined by LSFG, and the baPWV, carotid IMT, and age. In addition, we examined whether significant associations were presented between pulse-wave analysis of the optic nerve head circulation, the baPWV, carotid IMT, and systemic and ocular parameters.
Materials and method
One hundred and thirty-six consecutive patients who visited the Vascular Function Section of the Department of Cardiovascular Center of Toho University Sakura Medical Center between April 1 2007 and October 1 2010 were studied. The exclusion criteria were patients who had diabetes mellitus, using systemic anti-hypertensive drugs, using anti–hyperlipidemic drugs, history of cardiovascular disease and heart failure, presence of cerebrovascular disease, arrhythmias (atrial fibrillation), glaucoma, and vitreous and retinal diseases. In the end, 33 patients whose mean ± standard deviation (SD) age was 57.3 ± 12.6 years, with a range from 29 to 80 years, met the study criteria. There were 19 men and 14 women, and all subjects were nonsmokers.
The Institutional Review Board of Toho University Sakura Medical Center approved the protocol of this study, and we began the research after all participants received information on the purpose and possible side-effects of the research protocol. All subjects provided a signed informed consent. The procedures used conformed to the tenets of the Declaration of Helsinki.
The baPWV, blood pressure, heart rate, and LSFG were measured after the patients rested for 10 minutes in a quiet and air-conditioned room maintained at 24°C. All subjects abstained from alcohol and caffeine for at least 12 hours prior to the measurements. All evaluations were made between 15:00 to 17:00 hours before a meal.
Measurement of baPWV, blood pressure, and heart rate
Measurements of the baPWV, blood pressure, and heart rate were done with the program embedded in the VaSera (Fukuda Denshi Co.LTD, Tokyo). The precise methods of baPWV were described in the previous report in detail [22]. Briefly, the brachial and ankle pulse waves were determined with inflatable cuffs, with the pressure maintained between 30 to 50 mmHg to ensure a minimal effect of the cuff pressure on the systemic hemodynamics. The blood pressure and heart rate were determined simultaneously [22]. The measurements were made in the supine position, and the right baPWV was used for the statistical analyses.
Measurements of carotid intima–media thickness (IMT)
High-resolution ultrasonographic imaging of the carotid artery with the B-scan mode was performed with the EUB-8500 (Hitachi, Co.LTD, Tokyo), with the probe frequency set to 7.5 MHz. The subjects were measured in the supine position with their head slightly turned from the sonographer. The procedures involved scanning the near and far walls of the carotid artery every 1 cm proximal to the carotid bulb in the longitudinal view. The IMT was defined as the average of the maximum IMT at 1 cm proximal to and 1 cm distal from the carotid bulb [23–25]. The IMT of the right carotid artery was used for the data analyses.
Other systemic parameters
The following systemic parameters were measured : age, systolic blood pressure (SBP, mmHg), diastolic blood pressure (DBP, mmHg), pulse pressure (mmHg), heart rate (beats/min, bpm), and body mass index (BMI, kg/m2). The mean arterial blood pressure (MAP, mmHg) was determined by the formula; MABP = DBP + (SBP-DBP)/3.
Measurement of pulse-wave analysis in optic nerve head circulation using LSFG
The determination of the LSFG from these images has been described in detail [19, 20, 26]. Briefly, the LSFG is obtained from a 21° section centered on the optic disc. This total of observation field is made up of 750 (width) × 360 (height) pixels. LSFG uses the mean blur rate (MBR) as an indicator of the relative velocity of the erythrocytes. The MBR is determined by the formula: MBR = 2 × (normalized blur rate) 2.
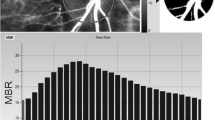
The normalized blur rate is calculated from the speckle pattern generated by reflected lights from the moving erythrocyte illuminated by a 830-nm wavelength diode laser beam [19, 21]. Initially, 118 MBR images (118 frames) were recorded in 4 seconds from the optic nerve head area. Next, a gray-scale map of the still images was made by averaging the MBR images (Fig. 1, upper panel). On the analysis screen, the pulse wave of the changing MBR which corresponded to each cardiac cycle were obtained (Fig. 1, middle panel). Finally, analysis of the screen, which is normalized to one pulse, was displayed (Fig. 1, lower panel), and the analysis of the pulse wave in the optic nerve head circulation was made on this screen.
Method of determining the pulse wave velocity in the optic nerve head circulation by laser speckle flowgraphy (LSFG). Upper panel: a gray-scale map of total measurement area. Circle designates the area that was measured the optic disc area. Middle panel: pulse waves showing changes in the MBR which is tuned to cardiac cycle for 4 seconds. The total number of frames is 118. Lower panel: normalization of one pulse. A = maximum MBR−minimum MBR. B = number of frames spent at one-half the value of A. C = Number of frames spent at normalized one pulse
The maximum MBR−minimum MBR waves is labeled as “A” and is shown in the lower panel of Fig. 1. The number of frames spent at one-half the value of A is designated as “B”, and the number of frames spent for one cardiac cycle is labeled “C”. The time analysis of pulse wave in the optic nerve head circulation was determined by the formula; blowout time = 100 × (B)/(C).
This parameter is named the blowout time (BOT), and we measured the BOT of the optic nerve head area three times and used the average for the statistical analyses. All subjects were measured in seated position, and pupils were dilated with 0.5% tropicamide eye drops. Only the data from the right eye were used for the analysis.
Measurements of other ocular parameters
The following ocular parameters were studied; the intraocular pressure (IOP mmHg) measured by applanation tonometry, and ocular perfusion pressure (OPP mmHg). The OPP was defined as; OPP = (2/3MAP)−IOP.
Statistical analyses
Data are presented as the means ± standard deviations (SDs) for the continuous variables. Pearson’s correlation coefficients were used to determine the relationship between the BOT, baPWV, IMT, age, and other systemic and ocular parameters. Multiple regression analysis was used to determine independent factors for age. A P value <0.05 was considered to be statistically significant. The Stat View version 5.0 program (SAS Institute Inc, Cary, NC, USA) was used for the statistical analyses.
Results
The results of the systemic and ocular measurements are shown in Table 1. The mean ± standard deviation (SD) of BOT was 49.2 ± 3.7, baPWV was 18.0 ± 4.3 m/second, and IMT was 0.80 ± 0.15 mm (Table 2). Examples of the analysis of BOT in a young, middle-aged, and elderly subjects are shown in Fig. 2. In a 29-year-old man (Fig. 2a), the BOT was 58.8, in a 52-year-old man (Fig. 2b), BOT was 51.5, and in a 79-year-old woman (Fig. 2c), BOT was 42.7.
Relationship between brachial ankle pulse wave velocity and blowout time. a Representative analysis of the normalization to one pulsation in 29-year-old man showing a blowout time of 58.8. b Analysis in 52-year-old man showing a blowout time of 51.5. c Analysis in 79-year-old woman showing a blowout time of 42.7
The results of Pearson’s correlation analysis between BOT, baPWV, IMT, and age and the ocular parameters are shown in Table 3. BOT was significantly and negatively correlated with age (r = −0.85, t = −9.0, P <0.0001), pulse pressure (r = −0.36, t value = −2.2, P = 0.04), baPWV (r = −0.72, t value = −5.8, P <0.0001), and IMT (r = −0.64, t value = −4.6, P < 0.0001).
The effect of baPWV on the BOT is shown in Fig. 3, that of the IMT on the BOT in Fig. 4, and that of age on the BOT is shown in Fig. 5. The results of Pearson’s correlation analysis between age and all parameters of the subjects are shown in Table 4. Age was significantly and positively correlated with pulse pressure (r = 0.35, t value = 2.1; P = 0.04), baPWV (r = 0.75, t value = 6.3, P < 0.0001), and with IMT (r = 0.56, t value = 3.7, P = 0.0008). Age was also significantly and negatively correlated with the BOT (r = −0.85, t value = −9.0, P < 0.0001).
The results of the multiple regression analyses of the systemic and ocular factors that were significantly associated with the age of the subjects are shown in Table 5. We analyzed the pulse pressure, baPWV, IMT, and BOT which had been shown to be significantly correlated with age. Both baPWV (odds ratio = 0.93, 95% confidence interval = 0.03–1.82, P = 0.04) and BOT (odds ratio = −2.26, 95% confidence interval = −3.27 to −1.26, P < 0.0001) were found to be significantly correlated with age.
Discussion
It has been shown that the IMT was significantly associated with albuminuria, retinal arteriosclerosis, and left ventricular mass index [23]. A significant association of baPWV and albuminuria has also been reported [25]. Thus, it was suggested that the IMT and baPWV may signal early arteriosclerotic changes. Nagaoka et al. determined the correlation between ocular circulation and age and IMT by evaluating the retinal arterioles by pulse wave analysis obtained by laser Doppler velocimetry [27, 28]. However, to the best of our knowledge, evaluation of the degree of atherosclerosis by the laser speckle method has not been reported.
Our results showed that BOT was significantly correlated with age, baPWV, and IMT. The BOT decreased with increasing age and baPWV, but with decreasing IMT. These findings suggested that the changing MBR which reflects the blood-flow velocity in the cardiac circulation become faster as the atherosclerotic changes worsen.
The value of baPWV is related to the stiffness of the large to middle-sized arteries [13, 29]. This would then suggest that the BOT of the optic nerve head circulation reflects not only stiffness of large to middle-sized arteries but also the thickness of the carotid artery. In addition, age was found to be significantly associated with BOT, and baPWV was strongly correlated with BOT.
The region of measurement was set for the entire optic nerve head area. This area was selected because it had the highest correlation with all of the systemic and ocular parameters in preliminary investigations. However, it has been suggested that BOT of the optic nerve head reflects not only artery blood flow but also venous and choroidal blood flow. In any case, measurements of BOT in the optic nerve head area using LSFG may be a useful method for evaluating atherosclerosis, because of the good correlation between BOT of optic nerve head area and age, baPWV, and IMT. However, both genders were evaluated by the same method because there was a small number of subjects. It will be necessary to reexamine a larger number of subjects, and determine whether there are differences between men and women. There is also a possibility that the uneven distribution of gender may be due to a bias in the gender of the subjects who visit the Vascular Function section in our hospital. An investigation based on health survey will be necessary in the future to evaluate a larger number of healthy subjects. In addition, a prospective study is needed to evaluate whether the BOT may detect changes with increased age.
In conclusion, our results confirmed that measurements of BOT in the optic nerve head by LSFG can be a useful method for determining whether early atherosclerotic changes are present in the optic nerve head circulation. Further studies will be needed to investigate the association of BOT to serious arteriosclerosis-related diseases such as cardiovascular diseases or cerebrovascular diseases.
References
Pinto E (2007) Blood pressure and ageing. Postgrad Med J 83:109–114
Mitchell P, Smith W, Chang A (1996) Prevalence and associations of retinal vein occlusion in Australia. The Blue Mountains Eye Study. Arch Ophthalmol 114:1243–1247
Yasuda M, Kiyohara Y, Arakawa S, Hata Y, Yonemoto K, Doi Y, Iida M, Ishibashi T (2010) Prevalence and systemic risk factors for retinal vein occlusion in a general Japanese population: the Hisayama study. Invest Ophthalmol Vis Sci 51:3205–3209
Hayreh SS, Zimmerman MB, Podhajsky P (1994) Incidence of various types of retinal vein occlusion and their recurrence and demographic characteristics. Am J Ophthalmol 117:429–441
Miyazaki M, Nakamura H, Kubo M, Kiyohara Y, Oshima Y, Ishibashi T, Nose Y (2003) Risk factors for age related maculopathy in a Japanese population: the Hisayama study. Br J Ophthalmol 87:469–472
Miyazaki M, Kiyohara Y, Yoshida A, Iida M, Nose Y, Ishibashi T (2005) The 5-year incidence and risk factors for age-related maculopathy in a general Japanese population: the Hisayama study. Invest Ophthalmol Vis Sci 46:1907–1910
Kaderli AA, Kaderli B, Gullulu S, Avci R (2010) Impaired aortic stiffness and pulse wave velocity in patients with branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol 248:369–374
Sato E, Feke GT, Appelbaum EY, Menke MN, Trempe CL, McMeel JW (2006) Association between systemic arterial stiffness and age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 244:963–971
Klein R, Klein BE, Knudtson MD, Cotch MF, Wong TY, Liu K, Burke GL, Saad MF, Jacobs DR Jr, Sharrett AR (2007) Subclinical atherosclerotic cardiovascular disease and early age-related macular degeneration in a multiracial cohort: the Multiethnic Study of Atherosclerosis. Arch Ophthalmol 125:534–543
Lehmann ED (1999) Clinical value of aortic pulse-wave velocity measurement. Lancet 354:528–529
Asmar R, Benetos A, Topouchian J, Laurent P, Pannier B, Brisac AM, Target R, Levy BI (1995) Assessment of arterial distensibility by automatic pulse wave velocity measurement. Validation and clinical application studies. Hypertension 26:485–490
Suzuki E, Kashiwagi A, Nishio Y, Egawa K, Shimizu S, Maegawa H, Haneda M, Yasuda H, Morikawa S, Inubushi T, Kikkawa R (2001) Increased arterial wall stiffness limits flow volume in the lower extremities in type 2 diabetic patients. Diabetes Care 24:2107–2114
Yamashina A, Tomiyama H, Takeda K, Tsuda H, Arai T, Hirose K, Koji Y, Hori S, Yamamoto Y (2002) Validity, reproducibility, and clinical significance of noninvasive brachial–ankle pulse wave velocity measurement. Hypertens Res 25:359–364
Matsushima Y, Kawano H, Koide Y, Baba T, Toda G, Seto S, Yano K (2004) Relationship of carotid intima–media thickness, pulse wave velocity, and ankle brachial index to the severity of coronary artery atherosclerosis. Clin Cardiol 27:629–634
Wofford JL, Kahl FR, Howard GR, McKinney WM, Toole JF, Crouse JR 3rd (1991) Relation of extent of extracranial carotid artery atherosclerosis as measured by B-mode ultrasound to the extent of coronary atherosclerosis. Arterioscler Thromb 11:1786–1794
Craven TE, Ryu JE, Espeland MA, Kahl FR, McKinney WM, Toole JF, McMahan MR, Thompson CJ, Heiss G, Crouse JR 3rd (1990) Evaluation of the associations between carotid artery atherosclerosis and coronary artery stenosis. A case-control study. Circulation 82:1230–1242
Tomiyama H, Yamashina A, Arai T, Hirose K, Koji Y, Chikamori T, Hori S, Yamamoto Y, Doba N, Hinohara S (2003) Influences of age and gender on results of noninvasive brachial–ankle pulse wave velocity measurement—a survey of 12517 subjects. Atherosclerosis 166:303–309
Sun Y, Lin CH, Lu CJ, Yip PK, Chen RC (2002) Carotid atherosclerosis, intima media thickness and risk factors—an analysis of 1781 asymptomatic subjects in Taiwan. Atherosclerosis 164:89–94
Tamaki Y, Araie M, Kawamoto E, Eguchi S, Fujii H (1995) Non-contact, two-dimensional measurement of tissue circulation in choroid and optic nerve head using laser speckle phenomenon. Exp Eye Res 60:373–383
Isono H, Kishi S, Kimura Y, Hagiwara N, Konishi N, Fujii H (2003) Observation of choroidal circulation using index of erythrocytic velocity. Arch Ophthalmol 121:225–231
Fujii H (1994) Visualisation of retinal blood flow by laser speckle flowgraphy. Med Biol Eng Comput 32:302–304
Shirai K, Utino J, Otsuka K, Takata M (2006) A novel blood pressure-independent arterial wall stiffness parameter; cardio–ankle vascular index (CAVI). J Atheroscler Thromb 13:101–107
Takiuchi S, Kamide K, Miwa Y, Tomiyama M, Yoshii M, Matayoshi T, Horio T, Kawano Y (2004) Diagnostic value of carotid intima–media thickness and plaque score for predicting target organ damage in patients with essential hypertension. J Hum Hypertens 18:17–23
O’Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK Jr (1999) Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med 340:14–22
Ishikawa T, Hashimoto J, Morito RH, Hanazawa T, Aikawa T, Hara A, Shintani Y, Metoki H, Inoue R, Asayama K, Kikuya M, Ohkubo T, Totsune K, Hoshi H, Satoh H, Imai Y (2008) Association of microalbuminuria with brachial–ankle pulse wave velocity: the Ohasama study. Am J Hypertens 21:413–418
Sugiyama T, Araie M, Riva CE, Schmetterer L, Orgul S (2010) Use of laser speckle flowgraphy in ocular blood flow research. Acta Ophthalmol 88:723–729
Nagaoka T, Sato E, Takahashi A, Sogawa K, Yokota H, Yoshida A (2009) Effect of aging on retinal circulation in normotensive healthy subjects. Exp Eye Res 89:887–891
Nagaoka T, Ishii Y, Takeuchi T, Takahashi A, Sato E, Yoshida A (2005) Relationship between the parameters of retinal circulation measured by laser Doppler velocimetry and a marker of early systemic atherosclerosis. Invest Ophthalmol Vis Sci 46:720–725
Yambe M, Tomiyama H, Hirayama Y, Gulniza Z, Takata Y, Koji Y, Motobe K, Yamashina A (2004) Arterial stiffening as a possible risk factor for both atherosclerosis and diastolic heart failure. Hypertens Res 27:625–631
Acknowledgments
There was no sponsorship or other support for this study. The authors have no financial conflicts of interest. Involved in design and conduct of this study (T.S., M.T.); involved in collection, management, analysis, and interpretation of the data (T.S., M.T); involved in preparation, review, or approval of the manuscript (T.S., M.T., Y.H., T.M ). The institutional review board of Toho University Sakura Medical Center approved the study, and we began research after obtaining informed consent from all participants in accordance with the Declaration of Helsinki. We had no statistical consultation or assistance.
Conflict of interest
The authors have no proprietary or financial interest in any aspect of this report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shiba, T., Takahashi, M., Hori, Y. et al. Pulse-wave analysis of optic nerve head circulation is significantly correlated with brachial–ankle pulse-wave velocity, carotid intima–media thickness, and age. Graefes Arch Clin Exp Ophthalmol 250, 1275–1281 (2012). https://doi.org/10.1007/s00417-012-1952-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-012-1952-5