Abstract
Background
One of the most frequent ocular features of systemic sclerosis (SSc) is dry eye disease (DED), which has been identified to occur in 37–79% of patients. Although several studies have found weak or no correlations between symptoms and signs of dry eye, symptoms are often the motivation for seeking eye care, and are therefore a critical outcome measure when assessing treatment effect. The aim of this study is to evaluate the impact of symptoms of dry eye on vision-related quality of life in patients with systemic sclerosis, and to investigate the relation between clinical tests and symptoms of dry eye in these patients.
Methods
In this cross-sectional study, 45 consecutive patients with SSc were enrolled. For evaluation of the symptoms the “Ocular Surface Disease Index (OSDI)” questionnaire was applied to all patients. After that, all individuals were submitted to a full ophthalmic examination, including the following tests: tear break-up time, Schirmer I, rose bengal staining. Patients were then grouped into dry eye and non-dry eye groups with regard to the diagnosis of dry eye. Mann–Whitney test was used to compare continuous variables, whereas the Fisher exact test was used to compare categorical data between groups. Spearman’s correlation test was used to analyze the correlations between clinical tests and OSDI scores. P values <0.05 were considered significant.
Results
Dry eye disease was diagnosed in 22 patients (48.9%). Other ocular surface abnormalities found were: blepharitis (40% of the patients), pterygium (15.6%), pinguecula (82.2%), and superficial punctate keratitis (26.7%). Among the 45 patients, 29 patients (64.4%) had symptoms of ocular surface disease. The mean OSDI score was 26.8 ± 25.8 (SD). There were no statistically significant differences in OSDI scores between DED and non-DED patients. No substantive correlations were found between OSDI scores and TBUT, Schirmer I, or rose bengal staining score, and none of the observed correlations reached statistical significance.
Conclusion
Symptoms of dry eye have a moderate impact on vision-related quality of life in patients with systemic sclerosis and do not correlate well with clinical findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic sclerosis (SSc) is a rare chronic disease of unknown cause characterized by fibrosis, degenerative changes, and vascular abnormalities in the skin, joints, and internal organs [1, 2]. Impairment of internal organs induces a wide spectrum of functional failures and limitations, affecting general health status and significantly decreasing health-related quality of life [3]. SSc has a worldwide distribution, occurring most commonly in females. The peak incidence appears in individuals between 45 and 64 years old [2].
One of the most frequent ocular features of SSc is dry eye disease (DED), which has been identified to occur in 37–79% of patients and is thought to be derived from fibrosis of the conjunctiva and lacrimal gland, which leads to a tear deficiency state that causes further damage to the ocular surface [4, 5]. Although the probability of dry eye causing blindness or visual impairment is low, it has a significant impact on the daily and social lives of patients [6, 7]. In a considerable number of cases, however, dry eye symptoms do not correlate well with clinical findings of DED [8–12]. Although several studies have found weak or no correlations between symptoms and signs of dry eye [8–12], symptoms are often the motivation for seeking eye care, and are therefore a critical outcome measure when assessing treatment effect [11, 13].
Patient-reported measurements used to evaluate the impact of eye disease on symptoms, functioning, and perceptions are referred to as vision-targeted health-related quality of life instruments [11]. Recently, some studies have developed ways of measuring patient-reported symptoms of dry eye, such as the Dry Eye Questionnaire, the McMonnies Questionnaire, and the Ocular Surface Disease Index (OSDI). The later is notable among other questionnaires for ocular surface disease for having undergone psychometric testing and having been accepted by the U.S. Food and Drug Administration (FDA) for use in clinical trials [14, 15].
Since lack of association between clinical findings and subjective symptoms among patients with dry eye have been reported in some studies, it is valuable to explore possible differences in associations of clinical signs with dry eye symptoms in patient populations with different manifestations or causes of DED [11].
The purpose of this study was to evaluate the impact of symptoms of DED on vision-related quality of life in patients with SSc, using a dry-eye-disease-specific instrument (OSDI questionnaire) and also to investigate the relation between clinical tests and the OSDI scores in these patients.
Methods
The study protocol was approved by the Ethics Committee of Hospital Clementino Fraga Filho (HUCFF). Consecutive patients with diagnosed SSc were recruited from the Rheumatology Service of HUCFF from April 2009 to September 2009. The diagnosis of SSc was based on the American College of Rheumatology criteria [16]. Patients with SSc sine scleroderma, scleroderma overlap syndrome, diabetes mellitus, or with severe systemic hypertension were excluded.
Before the clinical examination, a trained interviewer administered the OSDI questionnaire to each patient. Subsequently, a comprehensive ophthalmologic evaluation, including tear function tests and ocular surface status, was performed by another physician.
The OSDI [14] (provided by Allergan, Inc. Irvine, CA, USA) was used to quantify the impact of dry eye symptoms on vision-related quality of life. This disease-specific questionnaire includes 12 questions which are subdivided into three groups: (1) ocular discomfort, which includes symptoms such as painful eyes, (2) functioning, which measures limitation in performance of common activities such as reading and working on a computer, and (3) environmental triggers, which measures the impact of environmental triggers, such as wind or drafts, on dry eye symptoms. The questions are asked with reference to a 1-week recall period. Possible responses refer to the frequency of the disturbance: none of the time, some of the time, half of the time, most of the time, or all of the time. The total OSDI score was calculated on the basis of the following formula: OSDI = [(sum of scores for all questions answered) × 100]/[(total number of questions answered) × 4]. Subscale scores were computed similarly, with only the questions from each subscale used to generate its own score. Thus, the OSDI overall and subscale scores were scored on a scale of 0 to 100, with higher scores representing greater disability. The scoring of the OSDI was performed according to the published guidelines [17].
The OSDI was considered in the study to evaluate the impact of dry eye with the following scores: 0–12 normal, 13–22 mild, 23–32, moderate, and 33–100 severe symptoms [18].
Tear film stability was assessed using tear film breakup time (TBUT). One drop of 2% sodium fluorescein (Fluoresceína®, Allergan, São Paulo-SP, Brazil) was instilled into the inferior fornix, and the patient was instructed to blink several times. Using the cobalt blue filter and slit-lamp biomicroscopy, the duration of time required for the first area of tear film breakup after a complete blink was determined. The mean value of a total of three measurements was recorded.
A 5-minute conventional Schirmer I test without anesthesia was performed to evaluate tear production. A commercially available 5 x 35-mm paper strip (Schirmer strips®, Ophthalmos, São Paulo-SP, Brazil) was placed over the lower lid margin between the junction of the middle and outer third of the lower lid. Patients were instructed to keep their eyelids closed during the Schirmer test.
The assessment of ocular surface damage was performed by touching the inferotemporal bulbar conjunctiva with a rose bengal strip (Rose Glo™, Rose Stone Enterprises, Alta Loma, CA, USA), wetted with one drop of a preservative-free isotonic sodium chloride solution, and the reaction was classified according to the van Bijsterveld scoring system [19], which could range from 0–9, higher scores indicating worse ocular surface damage.
Abnormal values of the tests were as follows: Schirmer test ≤5 mm in 5minutes, TBUT <10 seconds, rose bengal staining score >3. Patients were diagnosed with DED if two or more of these tests (Schirmer,TBUT, or rose bengal) were abnormal. The diagnosis of DED in this study was made by extrapolating the Japanese [20] and Copenhagen criteria [21].
Demographic and clinical characteristics of the patients were analyzed by descriptive statistics. Correlation between clinical tests and dry eye symptoms was assessed using Spearman’s correlation analysis. Patients were grouped into DED and non-DED groups. Mann–Whitney test was used to compare continuous variables, whereas the Fisher exact test was used to compare categorical data between groups. P value of <0.05 was considered as significant.
Results
Forty-five patients were enrolled in this study. Forty (88.9%) patients were female and five (11.1%) were male, and the mean age was 51 years (range, 22–77). According to the criteria adopted in this study, DED was diagnosed in 22 patients (48.9%). Other ocular surface abnormalities found were: blepharitis (40% of the patients), pterygium (15.6%), pinguecula (82.2%), and superficial punctate keratitis (26.7%). Among the 45 patients, 29 patients (64.4%) had symptoms of ocular surface disease such as itching, burning, foreign body sensation, dryness, or redness. Twenty-three patients (51.1%) had a score higher than 22 in the OSDI questionnaire (Table 1).
Table 2 presents the characteristics of the patients, divided into DED and non-DED groups, by age, sex, and clinical examination findings. There were no significant differences between groups in terms of age (p = 0.2) or sex (p = 0.67). Furthermore, the two study groups were comparable for ocular surface abnormalities (p > 0.13). With respect to DED evaluation for all patients, the following results were obtained: Schirmer I, 11.7 ± 10.9 mm (range, 0–35); TBUT, 4.4 ± 3.1 s (range, 1–12); rose bengal staining, 0.98 ± 1.4 (range, 0–5).
The OSDI overall and subscale scores of the patients are shown in Table 3. There were no statistically significant differences in OSDI overall score or in any of the subscale scores between DED and non-DED patients.
Correlation analyses between OSDI (overall and subscale scores), TBUT, Schirmer I test and rose bengal staining scores are described in Table 4. No substantive correlations were found and none of the observed correlations reached statistical significance.
Discussion
DED is a multifactorial disease of the tears and ocular surface that results in symptoms of discomfort, visual disturbance, and tear film instability, with potential damage to the ocular surface and adverse impact on vision-related quality of life [7, 22]. SSc is a systemic autoimmune disease associated with high prevalence of DED [4, 5]. We sought to evaluate the impact of symptoms of DED on vision-related quality of life and its correlation with clinical findings in patients with SSc. Although a few studies have assessed DED in patients with SSc, assessments of symptoms have been very limited [23–25]. Furthermore, this study is the first to evaluate the impact of DED symptoms in vision-related quality of life in SSc patients.
The prevalence of DED in this study (48.9% of the patients) correlates well with previous studies that showed a prevalence ranging from 37–79% of patients [4, 26, 27]. In this study, symptoms usually related to dry eye, such as itching, burning, foreign body sensation, dryness, redness, were reported by 29 patients (64.4%). Other studies showed that 34.6–72% of patients with SSc have ocular symptoms related to DES [23–25].
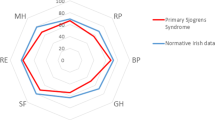
The Ocular Surface Disease Index (OSDI) is a 12-item questionnaire designed to provide a rapid assessment of the symptoms of ocular irritation consistent with DED and their impact on vision-related functioning [14]. Systemic disease factors could have their own additional impact on vision-targeted health-related quality of life. Since OSDI is a dry-eye-disease-specific instrument, it is expected to be less influenced by additional factors [10]. We found that patients with SSc had OSDI scores (mean 26.8) similar to those previously published for moderate dry eye patients [14], and lower than the ones reported for patients with Sjögren’s syndrome. In previous studies, patients with Sjögren’s syndrome were found to have a mean OSDI score ranging from 30 to 58.6 [11, 12].
The pathophysiology of DED associated with SSc is thought to be due to fibrosis of the conjunctiva and lacrimal gland [4, 5]. On histology, there is fibrosis of the conjunctiva associated with degranulating mast cell. There have been parallels drawn between primary Sjögren’s syndrome and DED from SSc, since both have primary ductal involvement that suggests similar mechanisms. However, lymphoid infiltrates are sparser in SSc. Conjunctival biopsy is valuable for differentiating between SSc and primary Sjögren’s syndrome [28]. The presence of fibrosis on histology suggests SSc, whereas lymphocytic infiltration is present in primary Sjögren’s syndrome [28].
In this study, the correlations of ocular surface parameters with OSDI overall and subscale scores tended to be weak or nonexistent, consistent with several other studies demonstrating poor correlation between signs and symptoms of dry eye [8–10].
Ozcura et al. have reported a significant inverse correlation between the OSDI and TBUT test scores, but no correlation between the Schirmer I test scores and OSDI [29]. In their study, Schirmer I test was performed with opened eyes. Reflex epiphora developed during the Schirmer I test was suggested by the authors as the underlying cause of the absence of any correlation between OSDI and Schirmer I scores. In support of this, Singh Bhinder et al. reported that the Schirmer I results change according to reflex epiphora when performed with opened eyes [30]. Indeed, closing the eyes while the test is performed has been recently found to increase its reliability, successfully minimizing the influence of such factors [31].
Schiffman et al. have found poor correlation between OSDI overall and subscale scores and traditional objective clinical measures of dry eye (Schirmer I, TBUT, fluorescein staining and lissamine green staining) when the results from all patients were analyzed together. However, when the analysis focused on only patients with Schirmer I scores less than 10 mm, low to moderate statistically significant correlations were detected for all subscales except vision-related function. The authors concluded that among a heterogeneous group of patients with DED, these measures lack sufficient sensitivity to capture the full range of ocular surface and tear abnormalities that produce typical dry eye symptoms. However, in certain subsets of patients (such as patients with tear deficiency), these clinical measures may correlate more closely with patient perception of disease severity [14].
Since the type of dry eye in Sjögren’s syndrome is more likely to be severe, and Sjögren-related dry eye is the prototype of tear-deficient dry eye, one should expect stronger associations between signs and symptoms of DED in patients with Sjögren’s syndrome. However, some studies have reported poor correlation between OSDI scores and clinical measures of dry eye in patients with Sjögren’s syndrome [11, 12]
Wangkaew et al. have found weak or no correlation between subjective symptoms of dry eye and the results of Schirmer I test in patients with SSc and in patients with rheumatoid arthritis. However, they found moderate statistically significant correlation in patients with systemic lupus erythematosus [32].
Decreased corneal sensation is a feature of severe dry eye which might alter patient’s perception of symptoms of ocular irritation, and might explain the lack of correlation in populations with high prevalence of severe DED [11, 12]. Reduced corneal sensation could provide inadequate feedback through ophthalmic nerve to the central nervous system, resulting in less efferent stimulation to lacrimal gland, with reduced tear production and promotion of a vicious cycle [11]. In addition, blepharitis and other ocular surfaces disorders commonly associated with DED may also influence patient’s perception of symptoms [33–35].
In this study, there were no statistically significant differences between DED and non-DED patients with regard to the presence of blepharitis, punctate keratitis, pterygium, or pinguecula. However, despite the significant difference in objective findings of all clinical diagnostic tests performed, we found no statistically significant differences in OSDI scores between DED and non-DED patients.
We believe that decreased corneal sensation is a possible explanation for the lack of correlation between signs and symptoms of DED in patients with SSc. Future studies should be carried out to evaluate corneal sensation in SSc. Given the fact that SSc is associated with peripheral neuropathy [36, 37], decreased corneal sensation may be a manifestation of the systemic disease itself, regardless of the severity of dry eye.
It is noteworthy that the diagnosis and assessment of DED are complicated by the considerable variation in the disease’s symptoms and signs, and the lack of definitive diagnostic tests. In this study, DED diagnosis was based on TBUT, Schirmer I test, and rose bengal staining. These are among the most common tests used in the clinical setting [38]. However, in light of the evidence concerning the lack of a relationship between symptoms and these dry eye clinical tests, more studies are needed to confirm the relationship between symptoms and other more objective diagnostic tools, such as tear film osmolarity test [39] and the double-pass scattering test [40]. In conclusion, symptoms of DED have a moderate impact on vision–related quality of life in patients with SSc, and do not correlate well with clinical findings.
References
Black CM, Stephens C (1993) Systemic sclerosis (scleroderma) and related disorders. In: Maddison PJ, Isenberg DA, Woo P, Glass DN (eds) Textbook of rheumatology. Oxford University Press, Oxford
Coral-Alvarado P, Pardo AL, Castaño-Rodriguez N, Rojas-Villarraga A, Anaya JM (2009) Systemic sclerosis: a worldwide global analysis. Clin Rheumatol 28:757–765
Hudson M, Thombs BD, Steele R, Panopalis P, Newton E, Baron M, Canadian Scleroderma Research Group (2009) Health-related quality of life in systemic sclerosis: a systematic review. Arthritis Rheum 61:1112–1120
Tailor R, Gupta A, Herrick A, Kwartz J (2009) Ocular manifestations of scleroderma. Surv Ophthalmol 54:292–304
Gomes BAF, Santhiago MR, Magalhães P, Kara-Junior N, Azevedo MNL, Moraes HV Jr (2011) Ocular findings in patients with systemic sclerosis. Clinics 66:379–385
Limburg H, Barria von-Bischhoffshausen F, Gomez P, Silva JC, Foster A (2008) Review of recent surveys on blindness and visual impairment in Latin America. Br J Ophthalmol 92:315–319
Miljanović B, Dana R, Sullivan DA, Schaumberg DA (2007) Impact of dry eye syndrome on vision-related quality of life. Am J Ophthalmol 143:409–415
Hay EM, Thomas E, Pal B, Hajeer A, Chambers H, Silman AJ (2008) Weak association between subjective symptoms or and objective testing for dry eyes and dry mouth: results from a population based study. Ann Rheum Dis 57:20–24
Nichols KK, Nichols JJ, Mitchell GL (2004) The lack of association between signs and symptoms in patients with dry eye disease. Cornea 23:762–770
Schein OD, Tielsch JM, Munõz B, Bandeen-Roche K, West S (1997) Relation between signs and symptoms of dry eye in the elderly. A population-based perspective. Ophthalmology 104:1395–1401
Vitale S, Goodman LA, Reed GF, Smith JA (2004) Comparison of the NEI-VFQ and OSDI questionnaires in patients with Sjögren’s syndrome-related dry eye. Health Qual Life Outcomes 1(2):44
Barboza MN, Barboza GN, de Melo GM, Sato E, Dantas MC, Dantas PE, Felberg S (2008) Correlation between signals and symptoms of dry eye in Sjögren’s syndrome patients. Arq Bras Oftalmol 71:547–552
Wilson SE, Stulting RD (2007) Agreement of physician treatment practices with the international task force guidelines for diagnosis and treatment of dry eye disease. Cornea 26:284–289
Shiffman RM, Christianson MD, Jacobsen G, Hirsch JD, Reis BL (2000) Reliability and validity of the ocular surface disease index. Arch Ophthalmol 118:615–621
Johnson ME, Murphy PJ (2007) Measurement of ocular surface irritation on a linear interval scale with the ocular comfort index. Invest Ophthalmol Vis Sci 48:4451–4458
Subcommittee for scleroderma criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee (1980) Preliminary criteria for the classification of systemic sclerosis (scleroderma). Arthritis Rheum 23:581–590
Walt J (2004) Ocular Surface Disease Index (OSDI) administration and scoring manual. Allergan, Inc., Irvine, CA
Miller KL, Walt JG, Mink DR, Satram-Hoang S, Wilson SE, Perry HD, Asbell PA, Pflugfelder SC (2010) Minimal clinically important difference for the ocular surface disease index. Arch Ophthalmol 128:94–101
Van Bijsterveld OP (1969) Diagnostic tests in the Sicca syndrome. Arch Ophthalmol 82:10–14
Homma M, Tojo T, Akizuki M, Yamagata H (1986) Criteria for Syogren’s syndrome in Japan. Scand J Rheumatol 18:26–27
Manthrope R, Oxholm P, Prause JU, Schiødt M (1986) The Copenhagen criteria for Syogren’s syndrome. Scand J Rheumatol 18:19–21
Report of the International Dry Eye Workshop (DEWS) (2007) Ocul Surf 5:65–204
Rasker JJ, Jayson MI, Jones DE, Matthews R, Burton JL, Rhys Davies E, Burton PA (1990) Sjögren’s syndrome in systemic sclerosis. A clinical study of 26 patients. Scand J Rheumatol 19:57–65
Alarcón-Segovia D, Ibánez G, Hernández-Ortíz J, Velázquez-Forero F, González-Jiménez Y (1974) Sjögren’s syndrome in progressive systemic sclerosis (scleroderma). Am J Med 57:78–85
Avouac J, Sordet C, Depinay C, Ardizonne M, Vacher-Lavenu MC, Sibilia J, Kahan A, Allanore Y (2006) Systemic sclerosis-associated Sjögren’s syndrome and relationship to the limited cutaneous subtype: results of a prospective study of sicca syndrome in 133 consecutive patients. Arthritis Rheum 54:2243–2249
West RH, Barnett AJ (1979) Ocular involvement in scleroderma. Br J Ophthalmol 63:845–847
Horan EC (1969) Ophthalmic manifestations of progressive systemic sclerosis. Br J Ophthalmol 53:388–392
Mancel E, Janin A, Gosset D, Hatron PY, Gosselin B (1993) Conjunctival biopsy in scleroderma and primary Sjögren’s syndrome. Am J Ophthalmol 115:792–799
Ozcura F, Aydin S, Helvaci MR (2007) Ocular surface disease index for the diagnosis of dry eye syndrome. Ocul Immunol Inflamm 15:389–393
Singh Bhinder G, Singh Bhinder H (2005) Reflex epiphora in patients with dry eye symptoms: role of variable time Schirmer-1 test. Eur J Ophthalmol 15:429–433
Serin D, Karsloğlu S, Kyan A, Alagöz G (2007) A simple approach to the repeatability of the schirmer test without anesthesia: eyes open or closed? Cornea 26:903–906
Wangkaew S, Kasitanon N, Sivasomboon C, Wichainun R, Sukitawut W, Louthrenoo W (2006) Sicca symptoms in Thai patients with rheumatoid arthritis, systemic lupus erythematosus and scleroderma: a comparison with age-matched controls and correlation with disease variables. Asian Pac J Allergy Immunol 24:213–221
Pflugfelder SC, Tseng SC, Sanabria O, Kell H, Garcia CG, Felix C, Feuer W, Reis B (1998) Evaluation of subjective assessments and objective diagnostic tests for diagnosing tear-film disorders known to cause ocular irritation. Cornea 17:38–56
Bekibele CO, Baiyeroju AM, Ajaiyeoba A, Akang EE, Ajayi BG (2010) Case control study of dry eye and related ocular surface abnormalities in Ibadan, Nigeria. Int Ophthalmol 30:7–13
Viso E, Gude F, Rodríguez-Ares MT (2011) The association of meibomian gland dysfunction and other common ocular diseases with dry eye: a population-based study in Spain. Cornea 30:1–6
Ribeiro RT, Fialho LM, de Souza LT, Barsottini OG (2009) Trigeminal sensory neuropathy associated with systemic sclerosis: report of three Brazilian cases. Arq Neuropsiquiatr 67:494–495
Poncelet AN, Connolly MK (2003) Peripheral neuropathy in scleroderma. Muscle Nerve 28:330–335
Korb DR (2000) Survey of preferred tests for diagnosis of the tear film and dry eye. Cornea 19:483–486
Jacobi C, Jacobi A, Kruse FE, Cursiefen C (2011) Tear film osmolarity measurements in dryeye disease using electricalimpedance technology. Cornea 30:1289–1292
Benito A, Pérez GM, Mirabet S, Vilaseca M, Pujol J, Marín JM, Artal P (2011) Objective optical assessment of tear-film quality dynamics in normal and mildly symptomatic dry eyes. J Cataract Refract Surg 37:1481–1487
Acknowledgment
Financial support: The authors would like to acknowledge FAPERJ (process # E-26/100.779/2009) for financial support of this work.
Author information
Authors and Affiliations
Corresponding author
Additional information
The funding organization had no role in the design or conduct of this research.
There are no conflicts of interest. The authors have no financial or proprietary interest in a product, method, or material mentioned herein.
Rights and permissions
About this article
Cite this article
de A. F. Gomes, B., Santhiago, M.R., de Azevedo, M.N.L. et al. Evaluation of dry eye signs and symptoms in patients with systemic sclerosis. Graefes Arch Clin Exp Ophthalmol 250, 1051–1056 (2012). https://doi.org/10.1007/s00417-012-1938-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-012-1938-3