Abstract
Background
The goal of this work is to establish a broad-range real-time polymerase chain reaction (PCR) diagnostic system for ocular fungal infection and to measure Candida and Aspergillus DNA in the ocular fluids obtained from unknown uveitis/endophthalmitis patients.
Methods
After obtaining informed consent, intraocular fluids (aqueous humor and vitreous fluid samples) were collected from 54 patients with idiopathic uveitis or endophthalmitis. Samples were assayed for Candida or Aspergillus DNA using broad-range (18S rRNA sequences) quantitative real-time PCR.
Results
Candida or Aspergillus DNA was detected in seven out of 54 patient ocular samples (13%). These PCR-positive samples showed significantly high copy numbers of Candida or Aspergillus DNA. On the other hand, fungal DNA was not detected in any of the other 46 samples collected from these idiopathic uveitis or endophthalmitis patients. In the one PCR-negative case, PCR did not detect any fungal genome in the sample, even though this patient was clinically suspected of having Candida endophthalmitis. Real-time PCR results were negative for fungal DNA in the bacterial endophthalmitis patients and in various uveitis patients. In addition, fungal DNA was also not detected in patients without ocular inflammation (controls).
Conclusions
Analysis of ocular samples by this broad-range real-time PCR method can be utilized for rapid diagnosis of patients suffering from unknown intraocular disorders such as idiopathic uveitis/endophthalmitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fungal endophthalmitis is a sight-threatening disease caused by human pathogenic fungi. Fungal infections are known to cause ocular inflammations such as endophthalmitis, uveitis, and keratitis. However, with the exception of for the Candida-associated ocular infection, the association between the fungus and the observed clinical features has yet to be elucidated. The well-known clinical features for Candida endophthalmitis include a fungal ball in the retina and vitreous opacity [1]. Fungal endophthalmitis can result from hematogenous dissemination or from a direct inoculation following trauma or surgery to the eye. Risk factors for fungal endophthalmitis include intravascular catheters, diabetes, malignancy, chemotherapeutic agents, and steroids. However, the clinical findings can be very diverse in some cases of ocular inflammatory disorders caused by fungal species. Moreover, fungal infections have been widely associated with keratitis, retinitis, uveitis, retinal/choroidal vasculitis, invasive orbital infection, and endophthalmitis. Because of this diversity, infection diagnosis is both difficult and time-consuming [1–4]. In order to be able to perform adequate treatments that can prevent these infectious agents from causing irreversible ocular damage, early examinations that correctly identify the etiology of the infection are necessary.
Conventional methods of diagnosis of fungal endophthalmitis include detection and isolation of the fungi from the intraocular fluids (aqueous humor or vitreous). However, since the sensitivity of conventional fungal cultures is not high, and the culture growth rates are slow, longer times are required before final results can be obtained [5, 6]. Thus, an early diagnosis can be important in ensuring there is prompt management of the endophthalmitis. Previous studies have shown that polymerase chain reaction (PCR) can be successfully and reliably used to make a diagnosis of fungal endophthalmitis [7–10]. However, even conventional PCR has yet to be able to determine quantitative information for the fungal genome in ocular samples.
In this study, we used real-time quantitative PCR for detection of Candida and Aspergillus DNA. We developed a protocol for the rapid detection of fungal DNA in ocular samples that was based on two major species (Candida and Aspergillus) that commonly cause eye disorders. We designed novel panfungal primers and probes that were complementary to the 18S rRNA sequences present in these species. Our broad-range real-time PCR proved to be an accurate method for quantitating fungal copies of both Candida and Aspergillus DNA.
Methods
Sample preparation
From 2006 to 2010, we consecutively enrolled endophthalmitis and uveitis patients in a prospective study that was conducted at our hospital (Table 1). After informed consent was obtained in all patients, we collected aqueous humor and vitreous fluid samples. A 0.1–0.2 ml aliquot of aqueous humor (asepsis) was collected in a syringe with a 30-G needle. We also collected non-diluted vitreous fluid samples (0.5–1.0 ml) during diagnostic pars plana vitrectomy (PPV) procedures that were conducted in patients with clinically suspected fungal endophthalmitis/uveitis. All of the patients displayed active intraocular inflammation at the time of sampling. The samples were transferred into a pre-sterilized microfuge tube and used for PCR. To ensure that no contamination of the PCR preparation occurred, the DNA amplification and the analysis of the amplified products were done in separate laboratories, as per a method reported for one of our previous studies [11].
For cultures of fungi, the Bacteria Work Station of the Tokyo Medical and Dental University Hospital processed all specimens (aqueous humor and vitreous fluids) within 1 h after the sample collection, with standard methods followed for the isolation and identification of fungal cultures [11].
In addition to the patient groups, we also analyzed samples from a control group. A total of 40 samples (20 aqueous humor and 20 vitreous fluids) were collected from patients who did not have any type of ocular inflammation (age-related cataract, macular edema, retinal detachment, idiopathic macular hole, or idiopathic epiretinal membrane).
The research followed the tenets of the Declaration of Helsinki and all study protocols were approved by the Institutional Ethics Committee of Tokyo Medical and Dental University. This clinical trial was registered, with registration information available at www.umin.ac.jp/ctr/index/htm. The study number attached to this registration is R000002708. The study was begun in April of 2006 and ended in April of 2010.
Polymerase chain reaction
To detect the Candida and Aspergillus DNA, we designed primers and probes for the broad-range PCR of the 18S rRNA sequences, which we have described in a previous report [10]. Kami et al. [12] developed primers and a probe for real-time PCR and demonstrated that the procedure was highly specific for the Aspergillus infection. In this study, we also designed a probe for use in the Candida species DNA amplifications (Fig. 1).
DNA was extracted from the samples using a DNA Mini Kit (Qiagen, Valencia, CA) installed on a robotic workstation that was set for automated purification of nucleic acids (BioRobot E21, Qiagen). The real-time PCR was performed using the Amplitaq Gold and the Real-Time PCR 7300 system (Applied Biosystems, Foster City, CA) or Light Cycler 480 II (Roche, Switzerland). The paired primers and TaqMan probes used for Candida and Aspergillus are shown in Fig. 1. Products were subjected to 50 cycles of PCR amplification, with cycling conditions set at 95°C for 10 min, followed by 50 cycles at 95°C for 15 s and 60°C for 1 min. For PCR assay sensitivity, PCR fragments were amplified from the DNA of C. albicans (Strain: ATCC 60193). Amplification of the human β-globulin gene served as an internal positive extraction and amplification control. Copy number values of more than ten copies/ml in the sample were considered to be significant.
Results
Specificity of Candida and Aspergillus species in broad-range real-time PCR
To evaluate the specificity of the Candida and Aspergillus species using broad-range real-time PCR of the 18S rRNA sequences, total nucleic acids of six Candida species and five Aspergillus species were extracted and assayed for 18S rDNA. As seen in Fig. 1, the broad-range real-time PCR detected six Candida species, i.e., C. albicans, C. parapsilosis, C. tropicalis, C. guilliermondii, C. glabrata, and C. krusei, along with five Aspergillus species, i.e., A. fumigatus, A. flavus, A. nidulans, A. niger, and A. terreus. By using several different primers and probes, we were able to separately detect each of these fungal species (Fig. 1).
Sensitivity of the real-time PCR assay
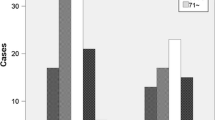
To confirm the broad-range real-time PCR assay sensitivity, PCR fragments were amplified from the DNA of C. albicans. The detection limit and standard range of the TaqMan real-time PCR were determined by using serial tenfold dilutions of linearized plasmid. The PCR results for the prepared samples showed that the best sensitivity for detecting C. albicans DNA was at a concentration of 101 per PCR (Fig. 2). There was no detection of the DNA in the negative control (nuclease-free water).
Detection of Candida and Aspergillus 18S rRNA gene in unknown uveitis/endophthalmitis patients
PCR results indicated a total of seven ocular fluid samples from the idiopathic uveitis or endophthalmitis patients (7/54, 13% positive, Table 1) were positive for Candida or Aspergillus DNA. These positive patients had high copy numbers of either Candida or Aspergillus DNA, with values ranging from 3.4 × 102 to 9.2 × 105 copies/ml. These results indicate the presence of a fungal infection. A representative PCR result is shown in Fig. 3. Conversely, conventional fungal cultures only found two out of the seven PCR-positive samples (both C. albicans) to be positive, while the other five samples were negative.
On the other hand, fungal DNA was not detected in any of the other 46 samples collected from these idiopathic uveitis or endophthalmitis patients. In the one PCR-negative case, PCR did not detect any fungal genome in the aqueous humor (<10 copies, case 8 in Table 1), even though this patient was clinically suspected of having Candida endophthalmitis. Real-time PCR results were negative for the Candida and Aspergillus DNA in the bacterial endophthalmitis patients (n = 7) and in the various uveitis patients (n = 24) who had been diagnosed with sarcoidosis, Vogt-Koyanagi-Harada disease, toxocariasis, toxoplasmosis, acute retinal necrosis, cytomegalovirus retinitis, or herpetic anterior iridocyclitis. In addition, fungal DNA was not detected in any of the 40 control samples that were collected from the patients without ocular inflammation.
Of the seven patients who were PCR positive, further examinations led to fungal endophthalmitis diagnoses as follows: five patients had endogenous endophthalmitis (four Candida and one Aspergillus), one had late postoperative endophthalmitis (Aspergillus, case 3), and one had post-traumatic keratitis-associated endophthalmitis (Candida, case 4) (Table 1).
Case reports
Case 1
A 65-year-old man with type II diabetes mellitus was treated for unknown uveitis over a period of a few weeks during 2009. He complained of blurred vision, decreased visual acuity, and pain in his right eye (RE). Ophthalmologic examination demonstrated the presence of characteristics of uveitis, bacterial endophthalmitis and fungal endophthalmitis. Vitreous opacity, including the presence of a fungal ball and yellowish retinal exudates, was seen in the fundus of his RE (Fig. 4a). After vitrectomy of his RE, real-time PCR of the vitreous sample obtained during the procedure indicated there were high copy numbers of Candida DNA (9.2 × 105 copies/ml, Fig. 4b). Based on these results, the patient was given systemic fluconazole (Table 1). Aspergillus DNA was not detected in this sample. A few days later, fungal culture of his vitreous specimen was also found to be positive for C. albicans. After being treated, he had complete resolution of his symptoms.
PCR results for case 1. a Fundus photograph of the right eye with a Candida infection. Dense vitreous opacity and retinal exudates are seen. b This is a graph of the PCR results. We calculated the copy number of fungal genomic DNA in the sample. After we measured both the tested ocular sample and the control DNA (105, 104, and 103 copies/ml) using real-time PCR, we then established the standard curve based on the results of the control DNA. Based on this standard curve, the sample Ct value was used to determine the DNA concentration of the sample. Final copy numbers of genomic DNA in the sample (copies/ml) were calculated based on the obtained sample volume and final dilution volume. High copy numbers of Candida DNA (9.2 × 105 copies/ml) were detected by PCR. Aspergillus DNA was not detected in the sample
Case 3
A 73-year-old man was referred to the Uveitis Clinic at our hospital in July 2008 because of keratic precipitates (KPs), cells in the anterior chamber, and anterior vitreous opacity in his RE that was associated with recurrent anterior uveitis. In his RE, diffuse pigmented KPs were seen (Fig. 5a). After considering both the clinical features and whole body inspections, we diagnosed this case as idiopathic uveitis. Although he was treated with topical corticosteroid and an antibiotic for 2 months, the KPs expanded (Fig. 5b). During the treatment, diffuse pigmented KPs continued to expand and then united. In addition, we also observed cells in the anterior chamber with hypopyon and dense anterior vitreous opacity. After informed consent was obtained, pars plana vitrectomy was performed in order to obtain a vitreous sample. Although fungi were not detected in a culture test, real-time PCR detected 1.8 × 103 copies/ml of the Aspergillus 18S rRNA gene (Table 1). Microbiological investigations performed using both culture and Gram’s staining of the vitreous sample proved to be negative. A blood test for β-D-glucan and fungal antigens including Aspergillus were also negative. We diagnosed the patient as having Aspergillus-associated late postoperative endophthalmitis that was related to his 2007 cataract surgery. The patient was subsequently treated using systemic fluconazole. The medication proved to be effective in treating the infectious endophthalmitis, with the inflammation in the anterior segment of his RE completely disappearing (Fig. 5c). After treatment, Aspergillus DNA in his sample was below the PCR detection level.
PCR results for case 3. a Slit photograph of the right eye with an Aspergillus infection. Diffuse pigmented keratic precipitates (KPs) are seen. b The pigmented KPs are expanded and united. Like the previous case, the Aspergillus DNA gene (1.8 × 103 copies/ml) but not the Candida DNA was detected in the sample. c After treatment, the inflammation completely disappeared
Discussion
PCR is well suited for the detection of fungal moieties due to its specificity and applicability for use with small samples such as ocular specimens. Moreover, real-time quantitative PCR can be used to determine whether or not the fungus is related to endophthalmitis. By utilizing our broad-range real-time PCR for the 18S rRNA sequence, we were able to rapidly diagnose Candida or Aspergillus endophthalmitis in a few patients that exhibited clinical evidence of a fungal infection. While our methodology showed both positive and negative results, it was generally more helpful than waiting for culture results, as the culture tests used to detect Candida or Aspergillus are both difficult to perform and require longer amounts of time due to the slow growth rates for these species [5, 6, 13]. In addition, the specificity of our PCR examination is good enough so that even a negative test is of benefit, as it helps to prevent making an incorrect diagnosis and administering a treatment for an infectious agent that is not present. Thus, this broad-range and real-time PCR system for ocular samples can provide a rapid diagnosis for those patients suffering from an unknown intraocular disorder such as idiopathic uveitis or endophthalmitis.
Fungal endophthalmitis is a sight-threatening disease that is most commonly caused by the Candida species. This disease usually accounts for a few percent of all of the cases of culture-proven endophthalmitis. The disease is normally acquired from an endogenous source that is spread by hematogenous dissemination. However, its occurrence may also be secondary to trauma, intraocular surgery, or corneal ulceration.
As confirmation of this suspected clinical disease is often difficult, there is frequently a delay in starting treatments. In the present patients, it was difficult to ascertain whether Candida or Aspergillus species were the causative agent in the intraocular inflammation. Since, in general, all of the patients were elderly and were immunocompetent, there was no focus area for the fungal infection systemically. As seen in Table 1, however, there were three exceptions. These included one case with a history of trauma (case 4), one case with a history of ocular surgery (case 3), and one case involving a normal infant (case 7), and for whom the case report details have been previously published [14].
In cases of fungal endophthalmitis in immunocompetent patients, specific additional antimycotic therapy has been shown to be effective in controlling the inflammation in the eye. In fact, all of the patients who were rapidly diagnosed by this PCR method were well controlled by the antimycotic treatment. Moreover, our PCR system was not only able to detect the conserved sequence of the fungal 18S rRNA gene, but it was also able to provide quantitative information from the ocular samples.
In recent years, PCR technology has been demonstrated to have a great potential in the detection and identification of low copy numbers of a microorganism’s DNA in clinical samples [7–12, 15, 16]. It also holds great promise for being able to identify small numbers of organisms in small sample volumes, a situation that is commonly seen when trying to examine intraocular samples from patients with infectious endophthalmitis. We evaluated these PCR techniques in order to determine a reliable and effective protocol for detecting Candida or Aspergillus species DNA in ocular samples. Our specific aims were to try and significantly increase the number of intraocular samples from which a confirmed diagnosis could be made and to reduce the time it took to make a mycologic diagnosis. In many previous reports, DNAs of Candida and Aspergillus species were detected in patients with clinically suspected fungal endophthalmitis [7–10, 15–20]. For example, Candida species such as C. albicans, C. parapsilosis, C. tropicalis, C. guilliermondii, C. glabrata, and C. krusei have been increasingly recognized as being capable of causing fungal endophthalmitis. However, C. albicans has been shown to be the causative agent in the majority of cases of culture-proven endophthalmitis. Moreover, Aspergillus such as A. fumigatus, A. flavus, A. nidulans, A. niger, and A. terreus have also been reported to be the causative species in an unknown ocular infection [17–20]. To detect these fungal species, our present PCR system used paired primers and specific probes that were based upon the 18S rRNA genes of Candida and Aspergillus (see Fig. 1).
In one patient who was clinically suspected of having Candida endophthalmitis, our new PCR method did not detect any fungal genome in the ocular sample (case 8 in Table 1). However, it should be noted that this sample was aqueous humor and not vitreous fluid. Perhaps if a vitreous sample had been obtained, we might have detected Candida DNA, as Candida endophthalmitis often results from hematogenous dissemination. In fact, this particular patient received intravascular catheters after his initial surgery. Thus, in order to be able to make an accurate diagnosis, the type of sample that is collected may be very important.
Although there are many advantages for using our PCR assay, there is one disadvantage when attempting to diagnose fungal ocular infection. While our PCR examination was able to detect all species of Candida and Aspergillus DNA, it could not detect other fungi DNA. Recently, Vollmer et al. reported on a novel broad-range real-time PCR assay for the rapid detection of human pathogenic fungi [21]. Their assay targeted a part of the 28S large subunit rRNA (rDNA) gene. Since this PCR assay can examine Candida species, Aspergillus species, Cryptococcus species, among others, we are currently trying to develop a new PCR examination that uses these primers and probes for the diagnosis of fungal ocular infections, including fungal endophthalmitis.
In conclusion, utilization of the PCR assay to examine ocular samples in patients with suspected fungal endophthalmitis and idiopathic uveitis or endophthalmitis appears to be clinically useful for detecting Candida and Aspergillus DNA. Thus, broad-range PCR for the 18S rRNA sequence is a reliable tool for the diagnosis of fungal endophthalmitis and in screening for fungal infections. Moreover, because real-time PCR is an accurate method of quantitating fungal copies, real-time quantitative PCR can be used to determine whether the fungus is related to the endophthalmitis. Since the sensitivity of conventional culture techniques is not high and these cultures tend to take a long time due to their slow growth, the use of a broad-range and real-time PCR system to analyze ocular samples may be a better way to obtain a rapid diagnosis in patients suffering from unknown intraocular infectious disorders. As early treatments are also essential for infectious endophthalmitis, this method may help to ensure that patients receive timely and optimal treatments. However, this is currently a limited research tool and not widely available for clinical labs at the present time. As a next step, we will need to work on making these tests widely available to clinical labs as oppose to only having them in research labs. In the near future, it is assumed that a comprehensive PCR system for examining fungi, bacteria, parasites, and viruses will become available, and be able to be used in the diagnosis of ocular infectious disorders.
References
Edwards JE Jr, Foos RY, Montgomerie JZ, Guze LB (1974) Ocular manifestations of Candida septicemia: review of seventy-six cases of hematogenous Candida endophthalmitis. Medicine 53:47–75
Rao NA, Hidayat AA (2001) Endogenous mycotic endophthalmitis: variations in clinical and histopathologic changes in candidiasis compared with aspergillosis. Am J Ophthalmol 132:244–251
Klotz SA, Penn CC, Negvesky GJ, Butrus SI (2000) Fungal and parasitic infection of the eye. Clin Microbiol Rev 13:662–685
Walsh TJ, Anaissie EJ, Denning DW, Herbrecht R, Kontoyiannis DP, Marr KA, Morrison VA, Segal BH, Steinbach WJ, Stevens DA, van Burik JA, Wingard JR, Patterson TF, Infectious Diseases Society of America (2008) Treatment of aspergillosis; clinical practice guidelines of the Infectious Disease Society of America. Clin Infect Dis 46:327–360
Kunimoto DY, Das T, Sharma S, Jalali S, Majji AB, Gopinathan U, Athmanathan S, Rao TN (1999) Microbiologic spectrum and susceptibility of isolates: part I. Postoperative endophthalmitis. Endophthalmitis Research Group. Am J Ophthalmol 128:240–242
Puliafito CA, Baker AS, Haaf J, Foster CS (1982) Infectious endophthalmitis. Review of 36 cases. Ophthalmology 89:921–929
Lohmann CP, Linde HJ, Reischl U (2000) Improved detection of microorganisms by polymerase chain reaction in delayed endophthalmitis after cataract surgery. Ophthalmology 107:1047–1051
Ferrer C, Colom F, Frasés S, Mulet E, Abad JL, Alió JL (2001) Detection and identification of fungal pathogens by PCR and by ITS2 and 5.8S ribosomal DNA typing in ocular infections. J Clin Microbiol 39:2873–2879
Anand AR, Madhavan HN, Sudha NV, Therese KL (2001) Polymerase chain reaction in the diagnosis of Aspergillus endophthalmitis. Indian J Med Res 114:133–140
Jaeger EE, Carroll NM, Choudhury S, Dunlop AA, Towler HM, Matheson MM, Adamson P, Okhravi N, Lightman S (2000) Rapid detection and identification of Candida, Aspergillus, and Fusarium species in ocular samples using nested PCR. J Clin Microbiol 38:2902–2908
Sugita S, Shimizu N, Watanabe K, Katayama M, Horie S, Ogawa M, Takase H, Sugamoto Y, Mochizuki M (2011) Diagnosis of bacterial endophthalmitis by broad-range quantitative polymerase chain reaction. Br J Ophthalmol 95:345–349
Kami M, Fukui T, Ogawa S, Kazuyama Y, Machida U, Tanaka Y, Kanda Y, Kashima T, Yamazaki Y, Hamaki T, Mori S, Akiyama H, Mutou Y, Sakamaki H, Osumi K, Kimura S, Hirai H (2001) Use of real-time PCR on blood samples for diagnosis of invasive aspergillosis. Clin Infect Dis 33:1504–1512
Akler ME, Vellend H, McNeely DM, Walmsley SL, Gold WL (1995) Use of fluconazole in the treatment of Candida endophthalmitis. Clin Infect Dis 20:657–664
Ito M, Yokoi T, Sugita S, Shinohara N, Nishina S, Azuma N (2010) Endogenous Candida chorioretinitis in a healthy infant. Jpn J Ophthalmol 54:629–631
Tarai B, Gupta A, Ray P, Shivaprakash MR, Chakrabarti A (2006) Polymerase chain reaction for early diagnosis of post-operative fungal endophthalmitis. Indian J Med Res 123:671–678
Hidalgo JA, Alangaden GJ, Eliott D, Akins RA, Puklin J, Abrams G, Vazquez JA (2000) Fungal endophthalmitis diagnosis by detection of Candida albicans DNA in intraocular fluid by use of a species-specific polymerase chain reaction assay. J Infect Dis 181:1198–1201
Shen X, Xu G (2009) Vitrectomy for endogenous fungal endophthalmitis. Ocul Immunol Inflamm 17:148–152
Moinfar N, Smiddy WE, Miller D, Miller D, Herschel K (2007) Posttraumatic Aspergillus terreus endophthalmitis masquerading as dispersed lens fragments. J Cataract Refract Surg 33:739–740
Kramer M, Kramer MR, Blau H, Bishara J, Axer-Siegel R, Weinberger D (2006) Intravitreal voriconazole for the treatment of endogenous Aspergillus endophthalmitis. Ophthalmology 113:1184–1186
Kalina PH, Campbell RJ (1991) Aspergillus terreus endophthalmitis in a patient with chronic lymphocytic leukemia. Arch Ophthalmol 109:102–103
Vollmer T, Störmer M, Kleesiek K, Dreier J (2008) Evaluation of novel broad-range real-time PCR assay for rapid detection of human pathogenic fungi in various clinical specimens. J Clin Microbiol 46:1919–1926
Acknowledgements
We thank Ms. Miki Katayama and Shizu Inoue for their technical assistance. We would like to also thank Drs. Hiroshi Takase and Yoshiharu Sugamoto for obtaining the samples used in this study. This work was supported by a Comprehensive Research on Disability, Health and Welfare grant, along with a Health and Labour Sciences Research Grant from the Ministry of Health, Labour and Welfare, Japan.
No financial relationships exist in the publishing of this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sugita, S., Kamoi, K., Ogawa, M. et al. Detection of Candida and Aspergillus species DNA using broad-range real-time PCR for fungal endophthalmitis. Graefes Arch Clin Exp Ophthalmol 250, 391–398 (2012). https://doi.org/10.1007/s00417-011-1819-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-011-1819-1