Abstract
Background
To determine whether rubella virus is involved in the pathogenesis of Fuchs heterochromic iridocyclitis (FHI).
Methods
Fourteen patients (14 eyes) diagnosed with FHI based on characteristic ocular manifestations and eight control subjects were studied. Aqueous humor (AH) samples from 14 FHI patients and one vitreous sample from a FHI patient were analyzed for intraocular antibody production against rubella virus by calculation of the Goldmann–Witmer coefficient (GWC). Viral detection by nested polymerase chain reaction and isolation by culture in RK-13 cells were conducted in nine FHI patients. In addition to laboratory examinations, medical history of rubella virus vaccination was also obtained.
Results
Ten patients with FHI examined showed intraocular synthesis of rubella virus antibodies (GWC > 3). A high index of rubella virus antibody production was also found in the vitreous sample (GWC = 30.6). GWC in all control subjects were below detectable level. The rubella genome was detected in two of nine patients, and rubella virus was isolated from one of nine patients with FHI. None of the patients with FHI had been vaccinated against rubella.
Conclusions
Our laboratory data strongly suggest a relationship between FHI and rubella virus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fuchs heterochromic iridocyclitis (FHI) is an intraocular inflammatory disease that constitutes approximately 0.5% to 6.2% of all cases of uveitis [1, 2]. FHI usually occurs in only one eye. Common clinical manifestations are: (1) chronic low-grade iridocyclitis including keratic precipitates, (2) iris heterochromia, atrophy or both, (3) absence of synechiae, and (4) early cataract [3, 4]. Complications such as glaucoma and vitreous opacities have been reported in 14.8% of patients with FHI [5]. Patients may remain asymptomatic for years, and diagnosis is often made by a decrease in visual acuity secondary to cataract which was observed in 77.8% at presentation. Therefore, it is difficult to detect FHI at the early stage and to prevent disease progression.
The etiology of FHI remains unknown. Because of the association between FHI and Horner’s syndrome, sympathetic nerve dysfunction was considered to be a cause of FHI [6]. Saari et al. [7] also reported vascular abnormality of the iris in patients with FHI, as demonstrated by fluorescein angiography. In addition to the organic abnormalities in patients, some infectious agents such as Toxoplasma gondii [8], herpes simplex virus (HSV) [9] and cytomegalovirus (CMV) [10], as well as auto-antigens [11, 12] have been proposed as possible causes of FHI. Recently, several studies have implicated rubella virus infection as a possible etiological agent of FHI [13–16]. However, it is suggested that intraocular presence of rubella virus is not necessary for the development of FHI [13, 16].
The objectives of the present study were to verify the relationship between rubella virus infection and FHI by examining intraocular antibody production and detecting viral RNA by polymerase chain reaction (PCR), and to attempt to isolate rubella virus from aqueous humor of FHI patients to confirm the intraocular presence of the virus.
Material and methods
Fourteen Japanese patients (14 eyes) with FHI who attended the uveitis clinic of Tokyo Medical University Hospital between 2006 and 2009 were enrolled in this retrospective review. The study was approved by the institutional review board.
Diagnosis of FHI was based on characteristic ocular manifestations including chronic anterior intraocular inflammation, keratic precipitate, absence of posterior synechiae, heterochromia or anterior stromal iris atrophy, and secondary cataract. The demographics and clinical background of the patients with FHI are shown in Table 1.
As controls, eight Japanese patients with other types of uveitis comprising sarcoidosis (one), Posner–Schlossman syndrome (one), herpetic iritis (one), Behçet disease (one) and unclassified intraocular inflammation (four) were selected. The diseases of the control patients were clearly differentiated from FHI by clinical manifestations and laboratory studies. Demographics of FHI patients and controls are listed in Table 2.
Aqueous humor (AH) samples were obtained from all FHI patients during surgery for secondary cataract or secondary glaucoma. All patients with FHI had no or low-grade ocular inflammatory activity at the time of sample collection. One vitreous humor (VH) sample was also obtained during vitrectomy for vitreous opacity. Rubella antibody titers in intraocular fluid (AH and VH) and serum samples from 14 FHI patients were determined by fluorescent antibody (FA) and enzyme immunoassay (EIA) techniques. Paired intraocular fluid and serum samples from each patient were tested at the same time. The Goldmann–Witmer coefficient (GWC) was calculated as follows: quantity of rubella virus-specific IgG/total IgG in intraocular fluid divided by rubella virus-specific IgG/total IgG in serum. A GWC value exceeding 3 was considered to indicate local antibody production, as described previously [14].
Rubella virus detection and isolation were conducted using AH samples from the nine most recent FHI patients (cases 6 to 14). For rubella virus isolation, RK-13 cells were inoculated with AH and incubated, and the cell cultures were serially passaged. The RK-13 cells were lysed by rapid freezing and thawing, and the lysate obtained was used for reverse transcription-polymerase chain reaction (RT-PCR). For rubella virus detection from ocular samples, total RNA was extracted from the samples using the High Pure Viral RNA kit (Roche Diagnostics, UK). For detecting rubella viral RNA, two nested RT-PCR were conducted for two parts of the E1 gene, designated as E1-2 region (466 bp) and E1-3 region (423 bp). The primer designs used for RT-PCR were listed in Table 3. The first round RT-PCR was performed as follows: 50°C for 30 min, followed by 95°C for 5 min, then 40 cycles of 90°C for 30 s, 61°C for 30 sand 72°C for 1 min., and 72°C for 5 min. For the nested PCR, 25 cycles of 98°C for 10 s, 59°C for 30 s (E1-2 region) or 66°C for 30 s (E1-3 region) and 72°C for 45 s were conducted. The PCR products were confirmed by electrophoresis in 1.5% agarose gel.
In addition to laboratory examinations, medical history related to exposure to rubella (vaccination or infection) was also obtained.
Results
Antibody titer and GWC for rubella virus
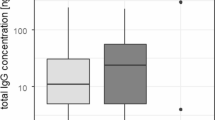
We attempted to measure rubella antibody titers and determine GWC using paired AH and serum samples collected from 14 patients with clinically definite FHI. Ten FHI patients demonstrated intraocular synthesis of rubella virus antibodies (GWC > 3) with median GWC of 45.1 (total range 5.7–186.1) (Fig. 1). In the remaining four patients with FHI (cases 11 to 14), total IgG in AH could not be measured because of inadequate AH samples, and therefore GWC could not be determined, although rubella antibody was positive in their AH samples (case 11: 32.5 IU, case 12: 130 IU, case 13: 20 IU, case 14: 28.5 IU). None of the control subjects had antibodies against rubella in AH samples and GWC values were below detectable level. The rates of intraocular antibody synthesis were significantly different (P < 0.01; Fisher’s exact test) between patients with FHI (ten of ten) and control patients (none of eight) (Table 2).
Evaluation of the rubella virus Goldmann–Witmer coefficient (GWC) values of ten patients with FHI and eight control patients. The median value of FHI patients is indicated by a horizontal black line. The threshold GWC value 3 is indicated by the dashed line. The GWC value is presented in a logarithmic scale
The vitreous sample from one FHI patient (case 6) was also examined. The rubella antibody titer in the VH sample was ×160, and total IgG was 14.9 mg/dl. The GWC of VH was high (GWC = 30.6).
Rubella virus gene detection from AH and lens anterior capsule
Using RT-PCR, the rubella genome was detected in two of nine AH samples from FHI patients (cases 6 and 7). Virus detection was confirmed by two primer sets targeting the E1 gene of rubella virus. The representative data of RT-PCR are shown in Fig. 2.
Representative results of the detection of rubella virus gene from ocular samples of case 6 using two nested RT-PCR. Lanes 1 and 2 indicate the PCR products of E1-2 and E1-3 regions, respectively. Lane M shows the 100 bp DNA ladder markers. Cap; lens anterior capsule, AH; aqueous humor. Note that the PCR products from AH are positive for rubella virus
Rubella virus isolation from AH
Rubella virus isolation was attempted in nine patients with FHI (Cases 6 to 14). Rubella virus was isolated from one patient with FHI (case 7). The results of RT-PCR obtained from lysates of various passages of RK-13 cells are shown in Fig. 3.
Detection of rubella virus gene using RT-PCR from different passages of RK-13 cells inoculated with aqueous humor sample collected from case 7. Lanes 1-5 show the PCR results of E1-2 region, and lanes 6-10 show the PCR results of E1-3 region. Lanes 1-3 and 6-8 are the results from passages 1 to 3, respectively, of RK-13 cells inoculated with AH. Lanes 4 and 9 indicate negative control and lanes 5 and 10 indicate positive control. Lane Ms are 100 bp DNA ladder markers. Note that the PCR products from the 3rd passages of RK-13 cell are positive for rubella virus
Medical history of rubella vaccination and infection
Fourteen patients with FHI were questioned for a medical history of rubella vaccination and infection (Table 1). None of the patients with FHI had been vaccinated against rubella, although one patient was uncertain. A previous medical history of rubella infection was confirmed in 11 cases.
Discussion
Many previous reports have speculated the etiology of FHI, but recent reports of the relationship between rubella virus and FHI have renewed the interest. Quentin et al. [13] demonstrated the existence of rubella virus in AH by GWC determination and PCR assay, and de Groot-Mijnes et al. [14] confirmed the presence of rubella infection by calculating GWC. In this study, we also demonstrated rubella infection in AH and VH by GWC determination and PCR assay. The epidemiologic observation revealed reduced incidence of FHI following the introduction of vaccination against rubella virus [15]. None of our patients with FHI had received vaccination against rubella virus. Together with previous reports, these results confirmed the relationship between FHI and rubella virus.
With regard to the diagnosis of FHI, Ruokonen et al. [16] reported the usefulness of determining intraocular antibody production rather than detecting the virus gene by RT-PCR. In their report, intraocular antibody production against rubella virus was found in all cases, whereas only two of 20 cases had positive results for PCR. In our study, the rate of rubella antibody proportion was 10/10 and that of virus gene detection by PCR was 2/9, and these findings agree with Ruokonen’s report.
On the other hand, rubella virus was isolated from the AH of one FHI patient in this study. Except with the congenital rubella syndrome, rubella virus is transmitted by the respiratory route, and replicates in the nasopharynx and lymph nodes and then spreads throughout the body causing fever and rash [17]. The general perception is that there is no carrier state and the reservoir exists only in active human cases. Therefore, it is unclear whether the virus detected and isolated from aqueous humor in the FHI patient was from acute infection, re-infection or re-activation of latent virus. In the case of congenital rubella syndrome, rubella virus may persist in the lens for many years [18]. We also tried to detect rubella virus from the lens anterior capsule in case 6 using RT-PCR, but the result was negative.
Since rubella virus has not been hitherto isolated from intraocular fluid of FHI patients, the genetic characters of rubella virus associated with FHI are unknown. In Japan, no nationwide epidemics of rubella have been documented since 1992 [19], but small outbreaks in local areas have been observed, and the virus genotypes isolated in various outbreaks were different [20]. By studying the genealogical background of rubella virus strains isolated from patients with FHI, it may be possible to determine the time of infection and the strain(s) with a predilection to induce FHI. Moreover, antigen-specific immune reaction has been suspected to play a role in the pathogenesis of FHI, based on the results of restriction of infiltrated T cells [21] and polymorphisms of cytotoxic T cell antigen 4 [22]. Analysis of the specific genetic modification of the rubella virus may clarify the characteristics and the tropisms of the virus. Efforts to isolate and characterize the virus from intraocular sites will elucidate the pathomechanism of FHI. Further investigations are warranted.
In summary, isolation of rubella virus from intraocular specimens of FHI patients is difficult. To the best of our knowledge, this is the first report of isolation of rubella virus from the aqueous humor of a patient with FHI. Intraocular existence of rubella virus in an FHI patient is a very interesting finding when considering the mechanism of FHI development. Although the number of samples examined in this study was small, the results confirm a relationship between rubella virus and FHI. Further investigations, especially in the isolation and characterization of rubella virus strains associated with FHI, are warranted.
References
Goto H, Mochizuki M, Yamaki K, Kotake S, Usui M, Ohno S (2007) Epidemiological survey of intraocular inflammation in Japan. Jpn J Ophthalmol 51:41–44
Tran VT, Auer C, Guex-Crosier Y, Pittet N, Herbort CP (1994) Epidemiological characteristics of uveitis in Switzerland. Int Ophthalmol 18:293–298
Franceschetti A (1955) Heterochromic cyclitis; Fuchs’ syndrome. Am J Ophthalmol 39:50–58
Mohamed Q, Zamir E (2005) Update on Fuchs’ uveitis syndrome. Curr Opin Ophthalmol 16:356–363
Velilla S, Dios E, Herreras JM, Calonge M (2001) Fuchs’ heterochromic iridocyclitis: a review of 26 cases. Ocul Immunol Inflamm 9:169–175
Regenbogen LS, Naveh-Floman N (1987) Glaucoma in Fuchs’ heterochromic cyclitis associated with congenital Horner’s syndrome. Br J Ophthalmol 71:844–849
Saari M, Vuorre I, Nieminen H (1978) Fuchs’s heterochromic cyclitis: a simultaneous bilateral fluorescein angiographic study of the iris. Br J Ophthalmol 62:715–721
Toledo de Abreu M, Belfort R Jr, Hirata PS (1982) Fuchs’ heterochromic cyclitis and ocular toxoplasmosis. Am J Ophthalmol 93:739–744
Barequet IS, Li Q, Wang Y, O’Brien TP, Hooks JJ, Stark WJ (2000) Herpes simplex virus DNA identification from aqueous fluid in Fuchs heterochromic iridocyclitis. Am J Ophthalmol 129:672–673
Chee SP, Jap A (2008) Presumed Fuchs heterochromic iridocyclitis and Posner–Schlossman syndrome: comparison of cytomegalovirus-positive and negative eyes. Am J Ophthalmol 146:883–889
Hammer H, Olah M (1975) Hypersensitivity towards alpha-crystalline in the heterochromia syndrome. Albrecht Von Graefes Arch Klin Exp Ophthalmol 197:61–66
van der Gaag R, Broersma L, Rothova A, Baarsma S, Kijlstra A (1989) Immunity to a corneal antigen in Fuchs’ heterochromic cyclitis patients. Invest Ophthalmol Vis Sci 30:443–448
Quentin CD, Reiber H (2004) Fuchs heterochromic cyclitis: rubella virus antibodies and genome in aqueous humor. Am J Ophthalmol 138:46–54
de Groot-Mijnes JD, de Visser L, Rothova A, Schuller M, van Loon AM, Weersink AJ (2006) Rubella virus is associated with Fuchs heterochromic iridocyclitis. Am J Ophthalmol 141:212–214
Birnbaum AD, Tessler HH, Schultz KL, Farber MD, Gao W, Lin P, Oh F, Goldstein DA (2007) Epidemiologic relationship between Fuchs heterochromic iridocyclitis and the United States rubella vaccination program. Am J Ophthalmol 144:424–428
Ruokonen PC, Metzner S, Ucer A, Torun N, Hofmann J, Pleyer U (2010) Intraocular antibody synthesis against rubella virus and other microorganisms in Fuchs’ heterochromic cyclitis. Graefes Arch Clin Exp Ophthalmol 248:565–571
Kimberlin DW (2002) Rubella virus. In: Richman DD, Whitley RJ, Hayden FG (eds) Clinical virology. ASM Press, Washington, DC, pp 1211–1225
Mets MB, Chhabra MS (2008) Eye manifestations of intrauterine infections and their impact on childhood blindness. Surv Ophthalmol 53:95–111
Katow S (2004) Surveillance of congenital rubella syndrome in Japan, 1978-2002: effect of revision of the immunization law. Vaccine 22:4048–4091
Nakayama T (2009) Laboratory diagnosis of measles and rubella infection. Vaccine 27:3228–3229
Labalette P, Caillau D, Grutzmacher C, Dessaint JP, Labalette M (2002) Highly focused clonal composition of CD8(+) CD28(neg) T cells in aqueous humor of fuchs heterochromic cyclitis. Exp Eye Res 75:317–325
Spriewald BM, Lefter C, Huber I, Lauer B, Wenkel H (2007) A suggestive association of fuchs heterochromic cyclitis with cytotoxic T cell antigen 4 gene polymorphism. Ophthalmic Res 39:116–120
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Suzuki, J., Goto, H., Komase, K. et al. Rubella virus as a possible etiological agent of Fuchs heterochromic iridocyclitis. Graefes Arch Clin Exp Ophthalmol 248, 1487–1491 (2010). https://doi.org/10.1007/s00417-010-1434-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-010-1434-6