Abstract
Background
To evaluate the role of preoperative optical coherence tomography (OCT), multifocal electroretinography (mfERG), and fluorescein angiography (FA) as prognostic factors for vision after pars plana vitrectomy (PPV) in diabetic macular edema (DME).
Methods
Thirty-five eyes of 34 patients who underwent PPV were retrospectively reviewed. Best-corrected visual acuity (VA) was measured at baseline, and at 3, 6, and 9 months after surgery. Patients were categorized into two groups according to the final VA. Group 1 consisted of eyes with 0.2 or more logMAR lines of visual recovery, the rest of the eyes being placed in group 2. Preoperative FA findings, central macular thickness and mfERG responses at the central macula were evaluated to determine their effect on visual outcome.
Results
Eighteen eyes showed improved VA after PPV, and were classified into group 1. Seventeen eyes were placed in group 2. The presence of macular ischemia did not affect the postoperative visual outcome between the groups, although a trend was noted toward macular ischemia with delayed implicit time. P1 implicit time at the central seven hexagons (eccentricity of 0–5°) was the only statistically significant factor predicting unfavorable visual outcome. There was significantly delayed implicit time in group 2 patients compared with those of group 1. MfERG responses at other retinal eccentricities and central macular thickness did not show significant association with visual prognosis.
Conclusions
Preoperative mfERG parameters, especially the implicit time, can be useful indicators for predicting functional visual prognosis after PPV in DME.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Diabetic macular edema (DME) is a main cause of visual impairment in patients with diabetic retinopathy [1, 2]. The condition is characterized by increased vascular permeability and the deposition of hard exudates in the central retina. Recently, many reports have suggested that pars plana vitrectomy (PPV) might be effective in patients refractory to conventional focal or grid laser macular photocoagulation [3–13]. These studies have shown a significant improvement in vision, and reduction of central macular thickness measured by optical coherence tomography (OCT).
Multifocal electroretinography (mfERG) is an objective test which assesses the electrical response in discrete portions of the central 40° of vision. The technique allows simultaneous measurement of multiple retinal responses at different locations, and provides a topographic mapping of retinal function. Previous studies have described changes of mfERG values in eyes with DME, and showed that mfERG could be used as an objective criterion for evaluation of DME [14–16].
In the present study, we obtained preoperative mfERG data, central macular thickness measured by OCT and FA findings of macular ischemia in patients with DME, and investigated the relationship between these parameters and postoperative visual acuity (VA) to verify their prognostic values.
Methods
Thirty-four consecutive patients (35 eyes) with macular edema caused by diabetic retinopathy underwent PPV at the Yonsei University Eye and ENT Hospital Vitreoretinal Service (Seoul, Korea) between June 2005 and January 2008. This study was approved by the Yonsei University Hospital Institutional Review Board responsible for research involving human subjects. Informed consent was obtained from each participant after the nature and possible consequences of the procedure had been explained.
Patients were included in the study if they had: (1) diffuse macular edema with attached posterior hyaloid caused by diabetic retinopathy as documented by slit-lamp biomicroscopy with contact lens, and diffuse fluorescein leakage on angiography, (2) a best-corrected visual acuity (BCVA) on the logMAR scale of ≥0.52 (Snellen equivalent ≤20/70), and (3) a minimum follow-up period of 9 months. Exclusion criteria were: (1) a thickened and taut vitreous membrane or posterior vitreous detachment diagnosed by OCT or the presence of a Weiss ring, (2) cataract surgery or intravitreal triamcinolone injection within 6 months before surgery, (3) laser treatment including panretinal photocoagulation, grid macular photocoagulation, or posterior capsulotomy, within 6 months before surgery, or (4) presence of ocular conditions including vitreous hemorrhage, preretinal hemorrhage, or tractional retinal detachment.
A complete ophthalmic examination including VA measurement, slit-lamp biomicroscopy using a 90+ diopter noncontact lens, fluorescein angiography, and color fundus photography was performed on every patient at baseline, and 3 months, 6 months, and 9 months after surgery. OCT and mfERG data were recorded before surgery. A standard Snellen VA chart was employed to measure BCVA at each examination. For statistical analysis, BCVA measurements were converted to the logMAR scale.
All mfERG data were recorded using the RETI scan multifocal system (Roland Consult, Brandenburg, Germany). Stimulation and recording of mfERG responses were performed using the m-sequence technique according to ISCEV guidelines [17]. The stimulus, consisting of 103 hexagons covering a visual field of 30°, was presented at a frame rate of 75 Hz on a monitor 24 cm from the patient’s eye. The luminance (97% contrast; mean luminance 61.8 cd/m2) of each hexagon independently alternated between black and white. The amplifier gain was set at 100,000, the lower cutoff frequency was 5 Hz, and the upper frequency 100 Hz. After maximum dilation of the pupil, contact lens ERG-JET electrodes were applied to the topically anesthetized cornea with one ground electrode in the forehead and two temporal reference electrodes. The eyes were optically corrected for near vision in order to see clearly the small fixation spot in the center of the stimulus matrix. For patients with poor vision such as those in this study, a spoke-shaped (filled cross) fixation target was used, and the patients were instructed to fixate at the intersection of the spokes.
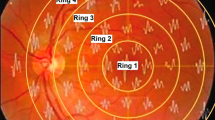
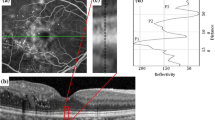
The first-order component of mfERG was analyzed, with reference to the mean response density of P1 amplitude (amplitude per unit of retinal area [nV/deg2]) and the mean implicit time (in milliseconds). The amplitude and implicit time from three different retinal eccentricities (0–5°, 5–10° and 10–15°) were analyzed. The central macular responses at an eccentricity of 0–5° were calculated by averaging individual responses of the central seven hexagons, ring 1 and ring 2. Other mfERG responses at an eccentricity of 5–10° and 10–15° were obtained from the data of ring 3 and 4, respectively.
The degree of macular ischemia was assessed on preoperative FA by an independent masked retinal specialist. In the evaluation of macular perfusion, broken perifoveal capillary rings ≥50% at the borders of the foveal avascular zones were classified as ischemic macula. Patients in the non-ischemic group lacked the sign of macular ischemia described above.
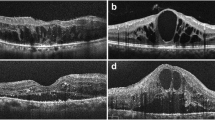
OCT was performed on every patient using a third-generation instrument (OCT3; Stratus Zeiss Humphrey, San Leandro, CA, USA). After dilation of the pupil, the macula was scanned in the horizontal and vertical meridians using the standard, linear crosshair pattern, with a scan length of 6 mm centered through the fovea, as determined by simultaneous evaluation of the red-free image on the computer monitor of the OCT scanner. The central macular thickness was measured manually in all scans, using the caliper tool built into the OCT software.
The surgical technique was standard three-port PPV. All operations were performed by a single surgeon (HJK). In all eyes, the posterior hyaloid membrane was separated from the retinal surface by applying suction from the vitreous cutter. For internal limiting membrane (ILM) peeling, 0.25% (w/v) indocyanine green was initially applied, with 15 seconds of contact time. When the ILM became stained, the ILM was cautiously peeled from the macula using a microvitreoretinal blade and intraocular forceps. An intravitreal injection of 4 mg/0.1 ml triamcinolone acetonide (40 mg/ml; Tamceton®; Hanall Pharmaceutical, Seoul, Korea) was always performed at the end of surgery. In patients with mild cataracts, phacoemulsification of the lens with posterior chamber lens implantation was performed during PPV.
In this study, the “group 1: favorable outcome” eyes included those in which VA improved by more than 0.2 logMAR lines, and the “group 2: unfavorable outcome” eyes showed less than 0.2 logMAR lines of improvement or worsened from baseline at the 9-month follow-up visit. Normal distribution was confirmed with histogram, quantile-quantile plot and Kolmogorov–Smirnov method. Baseline demographic and clinical parameters were compared between the two groups.
Statistical analysis was performed by using SPSS® Version 17.0 (SPSS Inc., Chicago, IL, USA) on a Windows platform. Numerical variables were subjected to an independent sample Student’s t-test, and categorical variables were analyzed by chi-square or Fisher’s exact tests to ensure comparability. Univariate and multiple variable logistic regression analysis were used for elucidating the independent influence of each potential factor like age, sex, lens status, diabetic retinopathy status, macular ischemia, preoperative VA, macular thickness, and mfERG responses on unfavorable visual outcome after surgery. Receiver operator characteristics (ROC) curve analysis was performed to find the optimal implicit time which predicts postoperative visual prognosis based on the improvement of 0.2 logMAR lines. Accuracy was determined by the area under the ROC curve (AUC), which was calculated with the 95% confidence intervals. In all tests, P < 0.05 was considered to be significant.
Results
A total of 35 eyes of 34 patients who completed at least 9 months of follow-up after PPV were included in the study. Of the 35 eyes, 18 eyes (51%) were classified into group 1, and 17 eyes were group 2. Baseline characteristics for both groups are listed in Table 1. There were no statistically significant differences in age, gender, retinopathy status, number of previous interventions, macular ischemia, lens status, or VA between the two groups. FA revealed that seven eyes (39%) in group 1 and eight eyes (47%) in group 2 had macular ischemia. The proportion of macular ischemia was not significantly different between the groups. All patients were treated with standard PPV and ILM peeling, without any intraoperative complications. Combined cataract surgery was performed in 22 (63%) of 35 eyes. No serious vision-threatening complications such as vitreous hemorrhage, retinal detachment, sclera perforation, or infectious endophthalmitis were found during the follow-up period.
The baseline logMAR of VA (mean ± SD) was 1.15 ± 0.38 in group 1 and 0.93 ± 0.40 in group 2 (P = 0.10, Student’s t-test). Figure 1 and Table 2 present the changes in logMAR of VA between baseline, 3 months, 6 months, and 9 months after surgery. Within each group, pairwise comparisons revealed a significant improvement in logMAR of VA at six and nine months in group 1 (P < 0.001), whereas group 2 showed a significant VA change between all time-points (P < 0.05). Between-group comparisons showed a significant difference in logMAR of VA change from baseline at only 9 months after treatment (P = 0.015).
Mean preoperative P1 amplitude and implicit time with odds ratio in relation to unfavorable visual outcome are shown in Table 3. The P1 amplitude (mean ± SD) at the central seven hexagons, representing an eccentricity of 0–5°, was 32.29 ± 14.57 nV/deg2 in group 1 and 24.97 ± 17.48 nV/deg2 in group 2. The P1 implicit time (mean ± SD) at an eccentricity of 0–5° was 42.61 ± 3.31 milliseconds in group 1 and 45.32 ± 3.03 milliseconds in group 2. After multivariate analysis, the only statistically significant factor predictive of unfavorable visual outcome was P1 implicit time at an eccentricity of 0–5° (P = 0.023), with borderline association with implicit time at an eccentricity of 5–10° (P = 0.051). Factors that showed no significant association included P1 implicit time at an eccentricity of 10–15° and P1 amplitude. The central macular thickness (mean ± SD) was 474.7 ± 110.9 µm in group 1 and 499.8 ± 100.2 µm in group 2. No significant association between macular thickness and visual outcome was observed (P = 0.391).
Table 4 presents mfERG responses for ischemic and non-ischemic macula. FA showed that 15 eyes had macular ischemia and 20 eyes had non-ischemic macula. The P1 implicit time was 45.47 ± 3.55 milliseconds in the ischemic group and 42.77 ± 2.88 milliseconds in the non-ischemic group. The implicit time was significantly delayed in the ischemic group (P = 0.023). There was a tendency toward decreased amplitude in ischemic macula, but no significant difference of amplitude was noted (P = 0.071).
A correlation between preoperative VA and baseline central macular thickness was observed. There was a significant correlation with a coefficient of determination (r2) of 0.16. The slope of the best fit line was approximately 0.1 logMAR of improved VA for every 100 µm decrease in central macular thickness. However, there was no significant correlation between preoperative central macular thickness and mfERG responses. Youden index and ROC curve analysis were performed to investigate the specific implicit time for prediction of visual prognosis. Figure 2 demonstrates an AUC of 0.820 and implicit time of 43.40 milliseconds as the cut-off value which best discriminates the unfavorable visual outcome group with a sensitivity of 94% and specificity of 71%.
Discussion
Among various interventions for DME that is unresponsive to laser treatment, PPV has shown promising results in recent studies [3–13]. Our previous work on DME patients showed that PPV with ILM peeling was of greater benefit than intravitreal triamcinolone injection [13]. In the cited study, improvement in VA and macular thickness was sustained to 6 months after surgery. However, in some patients, a significant reduction of macular thickness as measured by OCT did not consistently correlate with improvement of VA [18, 19]. Kumar and colleagues reported that visual improvement after PPV in DME patients was limited, despite a reduction in macular thickness [18].
mfERG is a technique assessing the local ERG from different regions of the posterior retina. Many authors have reported postoperative changes after PPV on DME patients in the morphology and function of the macula, using OCT and mfERG [14–16]. Yamamoto and co-workers also showed that mfERG provided additional evidence of improved physiological function of the macula, and of the safety of PPV [16].
In the present study, we sought to identify factors affecting visual prognosis after PPV, using mfERG parameters between favorable and unfavorable VA groups. This result would provide appropriate indications of PPV by detecting patients on whom surgery should not be performed because any benefit was unlikely. Patients were categorized by change in VA at the 9-month follow-up, in comparison with baseline values, and preoperative mfERG data at three different retinal eccentricities were analyzed to determine whether they could be used as a prognostic factor. We also investigated mfERG responses in correlation with macular ischemia or non-ischemia defined by FA.
Our most important finding was that delayed P1 implicit time at the central fovea was found to be the only factor strongly predictive of unfavorable visual outcome. According to the multiple logistic regression analysis, the patients with DME who showed relatively delayed implicit time preoperatively tended to have poor visual outcome after surgery (OR: 2.87; 95% CI: 1.16–7.15). However, central macular thickness and mfERG responses at an eccentricity of 5–15° did not show significant associations with postoperative visual outcome. The implicit time at an eccentricity of 5–10° had a weak predictive value, but it was not statistically significant. This suggests that preoperative implicit time at the central macula could be used to predict postoperative visual outcome, and may be a very sensitive method for measuring macular function. This is consistent with data of a previous report which demonstrated that delayed implicit timing changes were observed in a large area of the retina in DME patients, whereas amplitude changes were not [20].
Bearse and colleagues considered that this might be attributable to the lower intersubject variability found for local implicit times. This provides smaller confidence intervals than for those obtained for local mfERG amplitudes, which thus require a larger relative deviation from normal to reach statistical significance [21]. A few studies on the relationship between implicit time and amplitude in early-stage diabetic retinopathy (DR) patients have appeared [22, 23]. It is known that the primary generators of mfERG signal, the outer plexiform layer and the bipolar cells, are the first to be damaged, but are not completely silenced in early-stage DR. Previous histopathologic study has shown that macular edema usually develops at the inner retinal layer (from the outer plexiform layer to the nerve fiber layer) and causes pathologic change such as necrosis in Müller cells [24]. We would thus expect that local retinal responses yielding mfERG signals might be significantly delayed, also in DME patients, but without definite abnormalities of amplitude.
There was a significant correlation between delayed implicit time and macular ischemia. This finding reconfirmed that implicit time is more sensitive than amplitude to vascular ischemia as well as DME. Similarly, Hvarfner and colleagues showed that macular ischemia correlated well with the prolonged implicit time of mfERG in retinal vein occlusion [25]. When we categorized patients to groups 1 and 2 by improvement of VA and evaluated the effect of macular ischemia, the presence of macular ischemia did not have significant influence on postoperative visual outcome. The number of macular ischemia cases was almost the same, seven eyes (39%) in group 1 and eight eyes in group 2 (47%). Also, this angiographic finding was not a significant prognostic factor for predicting the unfavorable outcome after multiple logistic regression analysis. Therefore, we can consider that mfERG responses probably predict postoperative visual prognosis better than macular ischemia documented by FA.
In our study, PPV led to visual improvement of 2 or more lines in 51% (18/35) of DME patients. This is similar to the results of other larger studies, that showed a functional benefit in approximately 50% of patients [3, 8, 11, 12]. Group 2 patients had a somewhat worse VA at baseline than did those of group 1, but the difference was not significant. Preoperative central macular thickness at an eccentricity of 0–5° did not show any significant between-group difference, although the macula was slightly thicker in patients of group 2. Preoperative macular thickness measured by OCT was of no prognostic value in prediction of visual outcome after surgery. This suggests that macular thickness is just one of several variables that can be used to evaluate the complex macular function.
The correlation of macular thickness measured by OCT with VA before the surgery was significant but modest (r = 0.40), showing that retinal thickness accounts for only 16% of the variability in concurrently measured VA. This is similar to those of previous reported studies which indicate that OCT cannot be a good surrogate for VA assessment in DME patients [26, 27]. Browning et al. analyzed data from the Diabetic Retinopathy Clinical Research Network (DRCR network) randomized trial and showed that OCT-based assessment of DME did not explain additional variation in baseline VA [28]. No correlation was found between macular thickness and mfERG responses at an eccentricity of 0–5°. One possible explanation might be that the central macular thickness measured by OCT could not reflect the ischemic component of macula accurately in DME. Recently developed spectral domain OCT would be useful to evaluate more detailed structures of DME by identifying the individual retinal layer. The critical cut-off value of implicit time for predicting postoperative unfavorable visual outcome was 43.40 milliseconds. This result means that the visual outcome after surgery would be relatively poor when preoperative implicit time is delayed more than 43.40 milliseconds. It is noteworthy that an attempt was made to identify a specific value of implicit time. This might be another useful surgical indication to the retinal specialists whether to perform the surgical treatment in DME patients. However, it is true that to quantify and establish a specific implicit time can be limited by the small sample size and lack of the control data in our current study.
Combined cataract surgeries were performed on 11 eyes (61% and 65%) in each group, and the lens status or number of cataract surgery was not significantly different at baseline. Patients with severe cataracts were not included in this study. After all, the influence of concomitant cataract surgery on the visual outcome will be minimal. There could be another problem about the possibility of cataract progression after surgery in the case of phakic eyes. However, Hutton and co-workers showed that 37% of patients developed significant cataract progression over 16–108 months after surgery, and Smiddy and associates reported a relatively lower rate of cataract formation [29, 30]. Thus, progression of cataract during the 9-month follow-up period would not affect postoperative visual outcome.
The most important limitation of this study may be the retrospective design with no normal control mfERG values. It is well-known that using relative values of mfERG to the normal control data is more appropriate because uncontrolled confounding factors may influence the mfERG values, and measurement of mfERG has a characteristic of inter-individual variation to some degree. Also, there could be a flaw about using the Snellen chart, due to inaccuracy in measuring low vision range and its property of no geometric progression of letters, although we converted Snellen VA to the logMAR scale. Therefore, further investigations in a larger group with normal control group will be necessary to apply these results in practice.
In conclusion, this study showed that 18 (51%) of 35 eyes of patients with DME experienced visual improvement after surgery. Between-group comparisons showed that preoperative mfERG parameter, especially P1 implicit time at the central fovea, was more useful than amplitude for predicting unfavorable visual outcome after PPV. However, central macular thickness measured by OCT did not differ significantly between the two groups. Thus, these findings would provide a proper indication of PPV for patients with DME who are likely to benefit from surgery.
References
Pelzek C, Lim JI (2002) Diabetic macular edema: review and update. Ophthalmol Clin North Am 15:555–563
Klein R, Klein BE, Moss SE, Cruickshanks KJ (1996) The Wisconsin Epidemiologic Study of Diabetic Retinopathy XVII: the 14-year incidence and progression of diabetic retinopathy and associated risk factors in type 1 diabetes. Ophthalmology 105:1801–1815
Kumagai K, Furukawa M, Ogino N, Larson E, Iwaki M, Tachi N (2009) Long-term follow-up of vitrectomy for diffuse nontractional diabetic macular edema. Retina 29:464–472
Yanyali A, Nohutcu AF, Horozoglu F, Celik E (2005) Modified grid laser photocoagulation versus pars plana vitrectomy with internal limiting membrane removal in diabetic macular edema. Am J Ophthalmol 139:795–801
Stolba U, Binder S, Gruber D, Krebs I, Aggermann T, Neumaier B (2005) Vitrectomy for persistent diffuse diabetic macular edema. Am J Ophthalmol 140:295–301
Bahadır M, Ertan A, Mertoğlu O (2005) Visual acuity comparison of vitrectomy with and without internal limiting membrane removal in the treatment of diabetic macular edema. Int Ophthalmol 26:3–8
Yanyali A, Horozoglu F, Celik E, Nohutcu AF (2007) Long-term outcomes of pars plana vitrectomy with internal limiting membrane removal in diabetic macular edema. Retina 27:557–566
La Heij EC, Hendrikse F, Kessels AG, Derhaag PJ (2001) Vitrectomy results in diabetic macular oedema without evident vitreomacular traction. Graefes Arch Clin Exp Ophthalmol 239:264–270
Yanyali A, Horozoglu F, Celik E, Ercalik Y, Nohutcu AF (2006) Pars plana vitrectomy and removal of the internal limiting membrane in diabetic macular edema unresponsive to grid laser photocoagulation. Eur J Ophthalmol 16:573–581
Yang CM (2000) Surgical treatment for severe diabetic macular edema with massive hard exudates. Retina 20:121–125
Kralinger MT, Pedri M, Kralinger F, Troger J, Kieselbach GF (2006) Long-term outcome after vitrectomy for diabetic macular edema. Ophthalmologica 220:147–152
Pendergast SD, Hassan TS, Williams GA, Cox MS, Margherio RR, Ferrone PJ, Garretson BR, Trese MT (2000) Vitrectomy for diffuse diabetic macular edema associated with a taut premacular posterior hyaloid. Am J Ophthalmol 130:178–186
Kim YM, Chung EJ, Byeon SH, Lee SC, Kwon OW, Koh HJ (2009) Pars plana vitrectomy with internal limiting membrane peeling compared with intravitreal triamcinolone injection in the treatment of diabetic macular edema. Ophthalmologica 223:17–23
Yamamoto S, Yamamoto T, Hayashi M, Takeuchi S (2001) Morphological and functional analyses of diabetic macular edema by optical coherence tomography and multifocal electroretinograms. Graefes Arch Clin Exp Ophthalmol 239:96–101
Ma J, Yao K, Jiang J, Wu D, Gao R, Yin J, Fang X (2004) Assessment of macular function by multifocal electroretinogram in diabetic macular edema before and after vitrectomy. Doc Ophthalmol 109:131–137
Yamamoto S, Yamamoto T, Ogata K, Hoshino A, Sato E, Mizunoya S (2004) Morphological and functional changes of the macula after vitrectomy and creation of posterior vitreous detachment in eyes with diabetic macular edema. Doc Ophthalmol 109:249–253
Marmor MF, Hood DC, Keating D, Kondo M, Seeliger MW, Miyake Y (2003) Guidelines for basic multifocal electroretinography (mfERG). Doc Ophthalmol 106:105–115
Kumar A, Sinha S, Azad R, Sharma YR, Vohra R (2007) Comparative evaluation of vitrectomy and dye enhanced ILM peel with grid laser in diffuse diabetic macular edema. Graefes Arch Clin Exp Ophthalmol 245:360–368
Patel J, Hykin P, Schadt M, Luong V, Fitzke F, Gregor ZJ (2006) Pars plana vitrectomy with and without peeling of the inner limiting membrane for diabetic macular edema. Retina 26:5–13
Greenstein VC, Holopigian K, Hood DC, Seiple W, Carr RE (2000) The nature and extent of retinal dysfunction associated with diabetic macular edema. Invest Ophthalmol Vis Sci 41:3643–3654
Bearse MA Jr, Adams AJ, Han Y, Schneck ME, Ng J, Bronson-Castain K, Barez S (2006) A multifocal electroretinogram model predicting the development of diabetic retinopathy. Prog Retin Eye Res 25:425–448
Fortune B, Adams AJ, Schneck ME (1999) Ophthalmoscopic and angiographic features of diabetic retinopathy are associated with local ERG response delays [ARVO Abstract]. Invest Ophthalmol Vis Sci 40:S714
Fortune B, Schneck ME, Adams AJ (1999) Multifocal electroretinogram delays reveal local retinal dysfunction in early diabetic retinopathy. Invest Ophthalmol Vis Sci 40:2638–2651
Fine BS, Brucker AJ (1981) Macular edema and cystoids macular edema. Am J Ophthalmol 92(4):466–481
Hvarfner C, Andreasson S, Larsson J (2006) Multifocal electroretinography and fluorescein angiography in retinal vein occlusion. Retina 26:292–296
Martidis A, Duker JS, Greenberg PB, Rogers AH, Puliafito CA, Reichel E, Baumal C (2002) Intravitreal triamcinolone for refractory diabetic macular edema. Ophthalmology 109:920–927
Massin P, Duguid G, Erginay A, Haouchine B, Gaudric A (2003) Optical coherence tomography for evaluating diabetic macular edema before and after vitrectomy. Am J Ophthalmol 135:169–177
Browning DJ, Apte RS, Bressler SB, Chalam KV, Danis RP, Davis MD, Kollman C, Qin H, Sadda S, Scott IU, Diabetic Retinopathy Clinical Research Network (2009) Association of the extent of diabetic macular edema as assessed by optical coherence tomography with visual acuity and retinal outcome variables. Retina 29:300–305
Hutton WL, Pesicka GA, Fuller DG (1987) Cataract extraction in the diabetic eye after vitrectomy. Am J Ophthalmol 104:1–4
Smiddy WE, Feuer W (2004) Incidence of cataract extraction after diabetic vitrectomy. Retina 24:574–581
Acknowledgment
This study was supported by a faculty research grant of Yonsei University College of Medicine.(6-2008-0260).
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no proprietary or financial interest in any of the products used in this study.
Rights and permissions
About this article
Cite this article
Kim, Y.M., Lee, S.Y. & Koh, H.J. Prediction of postoperative visual outcome after pars plana vitrectomy based on preoperative multifocal electroretinography in eyes with diabetic macular edema. Graefes Arch Clin Exp Ophthalmol 248, 1387–1393 (2010). https://doi.org/10.1007/s00417-010-1398-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-010-1398-6