Abstract
Purpose
To compare the visual outcome of primary versus secondary traumatic cataract extraction and primary versus secondary intraocular lens (IOL) implantation.
Methods
The medical charts of consecutive patients who developed cataract following open and closed-globe injuries and were referred to our institute were reviewed. The best-corrected visual acuity of the patients who underwent primary and secondary cataract extraction and those with primary and secondary IOL implantation was assessed at presentation and at the end of the follow-up.
Participants
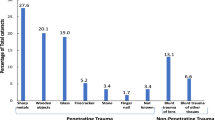
Sixty-nine eyes of 69 patients developed cataract after being involved in ocular trauma. Forty-five eyes had open-globe injury and 24 had closed-globe injury. The right eye was involved in 26 injuries and the left in 43.
Results
Best-corrected visual acuity (BCVA) of 20/40 or better was not statistically associated with the type of cataract extraction (extracapsular versus phacoemulsification) (in open-globe injury p = 0.181 and in all p = 0.662) and placement of anterior or posterior IOL (in open-globe injury p = 0.196 and in all p = 0.114). The timing of surgery (as immediate surgery or later as a second surgery) and the timing of intraocular lens implantation (during the extraction of the cataract or later in a secondary procedure) were not statistically associated with BCVA of 20/40 or better (in open-globe injury p = 0.322 and 0.381 in all p = 0.460 and 0.450, respectively). Irreversible amblyopia in children was a statistically significant factor for this visual acuity both in patients with open-globe injury (p = 0.036) and in all patients (p < 0.001).
Conclusions
In traumatic cataract, the visual outcome did not differ between primary and secondary cataract extraction and between primary and secondary IOL implantation in adults. In the amblyogenic age, primary surgery with IOL implantation should be preferred.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
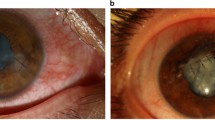
Open- and closed-globe injuries may result in various ocular injuries including cataract. Traumatic cataract has been encountered in 27–65% of the ocular trauma cases [1–3]. We have found it to occur in 3.45 per 100,000 per year or 4.6 per 10,000 outpatient visits (manuscript in publication). The literature addressed traumatic cataract extraction in children. Visual acuity of 20/40 or better was achieved in 45–70% of the children after traumatic cataract extraction [4–6]. The cataract may be localized, and when eccentric and small, may not require surgery. In most cases, however, an extensive opacity is encountered, requiring cataract extraction. This surgery may be performed in the initial setting of wound closure in cases of open-globe injuries or immediately at presentation in closed-globe injuries (primary procedure) or as a later procedure (secondary procedure).
Primary procedure is advantageous in avoiding second surgery and shortening the time of rehabilitation. It was initially employed in poor surgical candidates and is essential if the capsule is torn to avoid lens particle induced glaucoma. Secondary procedure allows planning of the surgery when the eye is quiet and after disclosing all the associated injuries.
During cataract surgery, an intraocular lens (IOL), preferably a posterior chamber one may be placed (primary implantation) or it may be inserted later in another surgery (secondary implantation). Primary implantation has the advantage of avoiding additional surgery, additional use of anesthetics, time and cost, and difficulties in IOL insertion if posterior synechiae present, which if released may cause posterior capsule rupture and vitreous loss. Assessment of the best IOL positioning for long-term stability may also be easier and visual rehabilitation faster. Secondary IOL implantation may on the other hand allow planning of the second intervention in a quiet eye, knowing the potential for visual rehabilitation after the assessment and treatment of the associated ocular injuries. It may allow better IOL calculation after the removal of corneal sutures when the refraction is more stable, which might be beneficial especially for toric IOL and also allow better visualization of the peripheral retina if pars plana vitrectomy is required. However, the posterior chamber IOL can usually be placed in the sulcus because of the adherence of the capsule leaves and may require posterior synechiolysis, which may increase postoperative inflammation.
To date, it is unknown whether the visual outcome is influenced by the timing of cataract extraction and IOL implantation in traumatic cataract; the issue is controversial due to the absence of comparable studies. This study was undertaken to compare primary with secondary cataract extraction and primary versus secondary IOL implantation in a consecutive series of patients with traumatic cataract. The cutting point for best-corrected visual acuity (BCVA) evaluation was 20/40 to allow comparison with pervious studies concerned with traumatic cataract [4–6].
Patients and methods
Sixty-nine consecutive eyes of 69 patients during a period of 10 years who developed cataract following ocular trauma were retrospectively reviewed. Forty-five eyes (65%) had open-globe injury and 24 (35%) had closed-globe injury. The male:female ratio was 3.3:1. The patients’ age at presentation ranged between 4 and 84 years (average 25.4 years). Twenty patients (29%) were younger than 10 years and were assessed separately. All the patients in this group developed a post-traumatic decrease in visual acuity that was attributed to amblyopia and not to other pathologies.
The amblyogenic age was considered to be the age in which amblyopia may develop (<10 years), while anti-amblyogenic treatment was employed up to the age of 17. The right eye was involved in 26 injuries and the left in 43. Calculation of the IOL power was determined according to the fellow, uninvolved eye in cases where the IOL power could not be determined in the affected eye. Patients were arbitrarily assigned for phacoemulsification or extracapsular cataract extraction and for primary or secondary procedure and IOL implantation. Phacoemulsification was performed in 14 eyes (20%) and by extracapsular cataract extraction in 28 eyes (41%). Intracapsular cataract extraction was performed in subluxated cataracts (three eyes, 4%). No pars plana lensectomy was performed in this series, a procedure that would be the procedure of choice in case of traumatic cataract extraction combined with retinal detachment (or other posterior segment surgeries). All children underwent lens aspiration (20 eyes, 29%). Four (6%) eyes did not undergo surgery at our facility and were not included in the analysis. Anti-amblyopic treatment by occlusion of the fellow eyes was initiated immediately after the diagnosis of cataract. Posterior chamber three-piece poly(methyl methacrylate) IOL or Foldable acrylic was inserted when capsular support existed. Primary procedures were performed within 24 h from the trauma. Secondary procedures were performed 1 week after the trauma or later. Eyes with closed-globe injuries, which presented with cataract and underwent surgery within 24 h, were included in the primary procedure group. Eyes with closed-globe injuries, which presented with cataract and underwent surgery 1 week after trauma or later and eyes, which developed traumatic cataract later were included in the secondary procedure group. Primary IOL implantation was done during the first cataract removal procedure, while secondary IOL implantation was performed as an additional surgery 1–2 months after the initial surgery. Patients were arbitrarily selected for each procedure. All patients with open-globe injury received prophylactic intravenous gentamicin sulphate 80 mg twice a day and cefamezine 1 g three times a day. Following surgery, topical antibiotics and corticosteroids were prescribed and tapered gradually. Mydriatics were given if the anterior chamber reaction was more than +2.
On follow-up examination, visual acuity was evaluated with Snellen charts under constant illumination. The intraocular pressure was measured and the anterior was evaluated with slit lamp. The posterior chamber was examined with indirect ophthalmoscope after pupil dilation. The follow-up period after the cataract extraction ranged between 1 and 62 months (average 14.7 months), 1–2 months in uncomplicated cases (cataract without other ocular injuries) and longer for complicated ones (cataract with other ocular injuries). All surgeries were performed by one surgeon (UR). The evaluation was performed by another surgeon (SR).
Each of the categorical covariates was individually assessed with Chi-square test. Fisher’s exact test was employed for samples with expectancy of less than 5. Two-tailed p < 0.05 was considered statistically significant. No IRB/institutional approval was required for this study.
Results
BCVA of 20/40 or better was achieved in 53% of all the patients with traumatic cataract and in 61% with open-globe injury. Thirty-two patients (46%) had ocular trauma that resulted in isolated traumatic cataract. All these patients had a final BCVA of 20/40 or better after cataract surgery (p < 0.001).
In the open-globe injury group, 14 (61%) out of the 23 eyes that underwent ECCE and nine (40%) out of the 22 eyes that underwent phacoemulsification gained BCVA of 20/40 or better (p = 0.181, Chi-square test) (Table 1). Of all the patients, 16 (57%) out of 28 eyes undergoing ECCE and eight (57%) out of 14 eyes undergoing phacoemulsification gained BCVA of 20/40 or better (p = 0.662, Chi-square test) (Table 2). In the open-globe injury patients, BCVA of 20/40 or better was achieved in eight (47%) out of the 17 primary procedures and in 15 (54%) out of the 28 secondary procedures (p = 0.322, Chi-square test). In all patients, BCVA of 20/40 or better was achieved in 11 (76%) out of the 19 primary procedures and in 22 (48%) out of the 46 secondary procedures (p = 0.460, Chi-square test). In the open-globe injury group, BCVA of 20/40 or better was achieved in 20 (59%) of the 34 primary IOL implantation procedures and in two (33%) of the six secondary IOL implantation procedures (p = 0.381, Fisher’s exact test). In all patients, BCVA of 20/40 or better was achieved in 30 (59%) of the 51 primary IOL implantation procedures and in three (43%) of the seven secondary IOL implantation procedures (p = 0.450, Fisher’s exact test). Seven eyes remained aphakic and had BCVA less than 20/40 with correction (p = 0.004, Fisher’s exact test). In patients with open-globe injury, 22 (58%) out of 38 eyes that had posterior chamber IOL had BCVA of 20/40 or better, while none (0%) out of two eyes that had anterior chamber IOL had BCVA of 20/40 or better (p = 0.196, Fisher’s exact test). Thirty-two (63%) out of 51 eyes that had posterior chamber IOL had BCVA of 20/40 or better. Only two (29%) out of seven eyes with anterior chamber IOL had BCVA of 20/40 or better (p = 0.114, Fisher’s exact test).
Of the five eyes with open-globe injury that were left aphakic, only one had final visual acuity better than 20/40. Of the four that had visual acuity of less than 20/40, three had traumatic retinal detachment and one had intraretinal foreign body. The six eyes with closed-globe injury, which were left aphakic, had also retinal detachment and their final visual acuity was less than 20/40. Those eyes that remained aphakic had poorer visual prognosis than those that had IOL implantation (p = 0.003, Chi-square test).
In patients with open-globe injury that were in the amblyogenic age (<10 years), secondary procedures or IOL implantation in all six eyes resulted in irreversible amblyopia with BCVA of <20/40 despite anti-amblyopic treatment, while it was 20/40 or better in the two children that had primary procedure and primary IOL implantation (p = 0.036, Fisher’s exact test). In the amblyogenic age (<10 years), secondary procedures or IOL implantation in six (86%) out of seven eyes resulted in irreversible amblyopia with BCVA of <20/40 despite anti-amblyopic treatment. All the 11 eyes that underwent primary procedures or IOL implantation had BCVA of 20/40 or better (p < 0.001, Fisher’s exact test). Two of the children (two eyes) that were already amblyopic at time of the injury and remained amblyopic after surgery and anti-amblyopic (occlusion) therapy were excluded from the calculation.
Of the 69 eyes, 12 (17%) had one or more posterior segment injuries. Ten (14.5%) eyes had retinal tear, eight (11.6%) had retinal detachment, two (2.9%) had intraretinal foreign body, six (8.7%) had vitreous hemorrhage, four (5.8%) had intravitreal foreign body, one (1.4%) had posterior vitreous detachment, and one (1.4%) had expulsive suprachoroidal hemorrhage. Of these posterior segment injuries, only retinal detachment was statistically associated with final BCVA of <20/40 (in all eight patients, p = 0.006, Chi-square test). The type of trauma (either open or closed) statistically had no effect on the visual outcome.
Discussion
In terms of BCVA of 20/40 or better, the outcomes of primary and secondary procedures, and primary and secondary IOL implantation were similar both in the open-globe injuries and in all the patients as well. However, synechiae may develop after traumatic cataract extraction in contrast to non-traumatized eyes and secondary IOL implantation may require synechiolysis that may increase postoperative inflammation and risk of developing cystoid macular edema. This may also limit the placement of PC-IOL to the ciliary sulcus, since in many cases, the anterior capsular rim may adhere to the posterior capsule over time. In another study, we found that only central corneal perforation and retinal detachment were statistically associated with BCVA of less than 20/40 (p = 0.002 and p = 0.006, respectively) (manuscript in publication).
The only statistically significant difference in visual acuity 20/40 or better was found between aphakic and phakic eyes. The reason for this difference is that eyes with poor visual prognosis, e.g., traumatic retinal detachment or intraretinal foreign body were left aphakic for later pars plana vitrectomy to allow better visualization. In those cases, injury included the retina and resulted in retinal scarring or proliferative vitreoretinopathy, limiting the visual prognosis. It is advisable, that in these cases, pars plana lensectomy and vitrectomy be employed as the primary procedure to decrease the risk of proliferative vitreoretinopathy and that the procedure will be performed by a posterior rather than anterior segment surgeon.
In one situation, primary cataract extraction with primary IOL implantation may be preferred over a secondary procedure and/or secondary IOL implantation. This situation is in toddlers and children up to 10 years old, when immediate visual rehabilitation is required to prevent amblyopia even if anti-amblyopic treatment is applied and contact lens or spectacles correction is given in the immediate postoperative period. A sequence of surgeries that includes closure of penetrating wound in the first procedure, secondary cataract extraction in the second procedure and secondary IOL implantation in the second or third procedure creates intervals in which irreversible amblyopia could be developed. If only one surgery that includes primary closure of the penetrating wound, cataract extraction and IOL implantation is performed, the period of visual rehabilitation is reduced and anti-amblyopic treatment may resume in the immediate postoperative period. The same is probably true if other interventions such as IOFB removal and retinal detachment surgery are required. Surgery delay in children may result in a poor visual outcome, despite a good anatomical outcome.
In children, even minimal opacity of the crystalline lens may require immediate intervention if it is centrally located. The recommendation for surgery of congenital cataract may also apply here and any cataract with opacity that involves the visual axis with a diameter of 3 mm or more should be surgically removed [7].
In cases of traumatic cataract, the anti-amblyopic treatment should be initiated in all the children and should be vigorous. Monitoring should be close. A cooperation of the family and the child is essential for the success of such treatment. Such recommendations have also been advocated by others [8].
Since the visual outcome may not be influenced by the type of surgery, its timing, and the timing of IOL placement in adults, the surgical choice may be dictated by the physician’s own preferences and experience and by the patients’ need to visual rehabilitation. In older patients, poor surgical candidates when the involved eye is the only functional eye, the best option would be one combined procedure. Patients with a history of recurrent uveitis may be approached with multi-step procedures and in patients with glaucoma, with injury to the anterior chamber angle or compromised cornea, it is better to avoid placement of anterior chamber IOL. IOL power calculation is difficult in cases of open-globe injuries and may be partially overcome by measuring the power of the fellow uninvolved eye, which only gives the approximated power. If miscalculation occurs, management by spectacle or contact lens may improve vision. In the setting of additional injury to the posterior segment, early pars plana lensectomy and vitrectomy by a posterior segment specialist is warranted.
Our results cannot be compared to the literature, because according to a literature search, a study comparing surgical parameters has never been reported. The caveat of our study is the limited number of the enrolled patients; however, traumatic cataract is fortunately not a frequent event. Nevertheless, our results clearly demonstrate the lack of statistically significant differences in surgical parameters for the treatment of traumatic cataract in adults, in contrast to children.
References
Dannenberg AL, Praver LM, Brechner RJ, Khoo L (1992) Penetrating eye injuries in the workplace. The National Eye Trauma System Registry. Arch Ophthalmol 110:843–848
Slusher MM, Greven CM, Yu DD (1992) Posterior chamber intraocular lens implantation combined with lensectomy-vitrectomy and intraretinal foreign-body removal. Arch Ophthalmol 110:127–129
Pieramici DJ, Sternberg P Jr, Aaberg TM Sr et al (1997) A system for classifying mechanical injuries of the eye (globe). The Ocular Trauma Classification Group. Am J Ophthalmol 123:820–831
Churchill AJ, Noble BA, Etchells DE, George NJ (1995) Factors affecting visual outcome in children following uniocular traumatic cataract. Eye 9:285–291
Gupta AK, Grover AK, Gurha N (1992) Traumatic cataract surgery with intraocular lens implantation in children. J Pediatr Ophthalmol Strabismus 29:73–78
Brady KM, Atkinson CS, Kilty LA, Hiles DA (1995) Cataract surgery and intraocular lens implantation in children. Am J Ophthalmol 120:1–9
Sheppard RW, Crawford JS (1973) The treatment of congenital cataracts. Surv Ophthalmol 17:340–347
Eriksen JR, Bronsard A, Mosha M et al (2006) Predictors of poor follow-up in children that had cataract surgery. Ophthalmic Epidemiol 13:237–243
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no proprietary or financial interests in this study.
Presented in part at the 12th American Academy of Ophthalmology Annual Meeting, Atlanta, GA, November 2008
Rights and permissions
About this article
Cite this article
Rumelt, S., Rehany, U. The influence of surgery and intraocular lens implantation timing on visual outcome in traumatic cataract. Graefes Arch Clin Exp Ophthalmol 248, 1293–1297 (2010). https://doi.org/10.1007/s00417-010-1378-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-010-1378-x