Abstract
Purpose
To evaluate the short- and long-term in vivo safety and efficacy of topical bevacizumab (Avastin) application for treatment of corneal neovascularization secondary to a variety of corneal diseases.
Methods
Thirty eyes of 27 patients with progressive corneal neovascularisation (not responding to conventional anti-inflammatory treatment) due to different underlying corneal diseases received topical bevacizumab (Avastin) eye drops (5 mg/ml Bevacizumab) for 0.5–12 months (five times/day on average). At each visit, a routine Snellen visual acuity assessment was performed, followed by ophthalmic examination including fluorescein staining. Changes of corneal neovascularization and vessel diameter were assessed using morphometry of standardized digital corneal photographs.
Results
Five patients (five eyes) developed new corneal epithelial defects during topical bevacizumab treatment. In 22 patients, no new epithelial defects were observed. None of the 27 patients complained about any drug-related ocular or systemic adverse events during follow-up. No allergic reactions were observed.
Corneal photographs of 21 eyes (19 patients) could be assessed. The mean reduction in vascularized area during treatment was 61%. The mean reduction in vessel diameter under topical Avastin therapy was 24%.
Conclusions
Off-label topical bevacizumab therapy against corneal neovascularization secondary to different corneal diseases was generally well-tolerated for up to 12 months. Bevacizumab (Avastin) eye drops inhibit corneal neovascularization, and lead to a reduction of the vessel diameter. Our results suggest that off-label use of Bevacizumab eye drops is a relatively safe and well-tolerated option for the treatment of corneal neovascularization. Care should be taken in patients with epithelial defects and neurotrophic keratopathy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Background
The human cornea is normally avascular, actively maintained by expression of antiangiogenic and antilymphangiogenic factors [1, 2]. In various inflammatory, infectious, degenerative or traumatic disorders, corneal neovascularization may occur. The consequences are decreased visual acuity and bad prognosis for corneal transplantation, by losing the immunologic privilege of the avascular cornea [3].
So far, no specific antiangiogenic treatment against corneal neovascularization has been available. Although steroids are the first choice in clinical practice, they are not always effective, and have serious side-effects. Several studies showed that members of the vascular endothelial growth factor (VEGF) family play a key role in pathologic neovascularization [4, 5]. Bevacizumab (Avastin, Roche Pharma AG) is a humanized monoclonal antibody blocking VEGF-A, which results in inhibition of the outgrowth of new vessels. Bevacizumab is approved for the treatment of metastatic colorectal cancer. It is currently injected “off-label” into the vitreous for the treatment of proliferative and nonproliferative diabetic retinopathy, neovascular age-related macular degeneration, and neovascular glaucoma, with promising results [2].
Recently, cell culture studies showed evidence for the safe use of bevacizumab on cultured human corneal cells [6]. We and others were recently able to demonstrate that bevacizumab eye drops are able to inhibit corneal angiogenesis in vivo in small pilot studies [7, 8, 13]. Based on these initial results, we initiated off-label treatment with Avastin eye drops in a larger group of patients with progressive corneal neovascularization not responding to conventional therapy. Here we report on the short- and long-term in vivo safety profile and efficacy of topical bevacizumab (Avastin) application for treatment of progressive corneal neovascularization due to a variety of corneal diseases in a larger group of patients.
Patients and methods
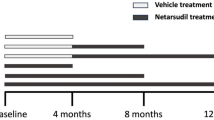
This uncontrolled, non-randomized case series consists of 30 eyes of 27 patients (22 male, five female) between 28–83 years of age (mean age: 51 ± 15 years) with progressive corneal neovascularisation due to limbal stem cell deficiency after chemical burn (n = 11), corneal graft rejection (n = 1), keratoplasty (n = 4), herpetic keratitis (n = 1), measles keratitis (n = 1), ocular pemphigoid (n = 2), Steven-Johnson syndrome (n = 1), KID syndrome (n = 1), graft-versus-host disease (n = 1), recurrent pterygium (n = 2), aniridia (n = 1) and Salzmann nodular corneal degeneration (n = 1). Patients received off-label topical bevacizumab (Avastin) treatment for 0.5–12 months (mean: 3.4 ± 2.9). Dosing varied from one to ten times per day (average five times per day). Bevacizumab eye drops were given in addition to current local and systemic therapy including steroid and immune suppression, which were unable to stop progressive corneal neovascularization alone. The therapy was terminated when corneal neovascularization had at least partly regressed. The institutional review board approved this treatment, and all patients gave a written consent prior to treatment.
Bevacizumab eye drops were prepared in the hospital pharmacy from the standard solution diluted in 0.9% saline to a concentration of 5 mg/ml. Avastin was portioned into 1 ml syringes for daily use. The eye drops were stored at -20°C; after opening they were used within 14 days, and kept at 4°C during that time. The costs of the Avastin eye drops is approximately 20 €/5 mg Avastin. In our case, by applying on average eye drops five times per day, the monthly cost would be around 150 €.
At each visit, a routine Snellen visual acuity assessment was performed, followed by an ophthalmic examination including fluorescein staining and tonometry. Changes in corneal neovascularization and vessel diameter were determined by repeatedly performed standardized digital slit-lamp pictures, which were then analyzed morphometrically using image analysis software based on grey filter sampling (Cell^F: Olympus, Hamburg, Germany) as described previously [7, 18]. The area of vascularization was measured in terms of pixels. Its ratio to the entire corneal area resulted in the percentage of corneal neovascularization. The vessel diameters before and during topical Avastin treatment were also measured in terms of pixels.
Statistical analysis was done by Microsoft Excel 2000 and InStat 3 Version 3.06 (GraphPad Software Inc., San Diego, CA, USA). Graphs were drawn using Prism4, Version 4.03 (GraphPad Software Inc.). Statistical significance was defined as P < 0.05.
Results
-
a.
Safety data
The mean duration of follow-up was 8.4 ± 5.1 months, and the median follow-up time was 7 months. The mean treatment duration was 3.4 ± 2.9 months. Table 1 summarizes the patients´ baseline data and therapy duration, and gives an overview of the outcomes after topical bevacizumab treatment.
In total, 14 eyes showed improvement in visual acuity, 15 eyes showed stable visual acuity and one eye showed vision worsening.
Generally, Avastin eye drops did not cause new epithelial defects. Out of 30 eyes, only five eyes (five patients) showed new corneal epithelial defects during topical bevacizumab treatment, but four patients already had preexisting epithelial defects prior to treatment. The remaining eye had a persistent epithelial defect immediately after pannectomy and limbal stem cell transplantation (after which Avastin eye drops were initiated). One patient with a pre-existing corneal ulcer developed a spontaneous corneal perforation 5 months after start of additional bevacizumab treatment.
Eleven eyes (ten patients) with preexisting recurrent epithelial defects showed no new epithelial defects under the topical Avastin therapy. No new epithelial defects were observed in the remaining 14 eyes. Corneal sensitivity was difficult to assess in most patients due to multiple previous corneal operations. Ten eyes (eight patients) showed punctate epithelial keratopathy. All of them already had punctate epithelial keratopathy prior to topical bevacizumab treatment.
None of the 27 patients complained about pain or discomfort throughout follow-up, nor about any drug-related ocular or systemic adverse events. No allergic reactions were observed. No IOP elevation was observed.
-
b.
Antiangiogenic efficacy: Avastin eye drops inhibit corneal neovascularization
Corneal photographs of 21 eyes (19 patients) were available for morphometrical assessment using image analysis. The mean reduction in vascularized area during treatment was 61% until visit 4 (Fig. 1). Visit 1 (n = 21 eyes) is defined as the first visit, prior to topical bevacizumab treatment. Visits 2, 3 and 4 are the follow-up visits. At visit 3, we only had photographs of 16 patients. At visit 4, there were only four patients remaining. Sixteen patients had a significant reduction of neovascularization at visit 3 (28%, p = 0.01) and four patients had a reduction of 61% at visit 4 (p = 0.0182).
Decrease of corneal neovascularization in 19 patients over four visits (paired t-test). Visit 1: n = 21 eyes, visit 2: n = 21 eyes, visit 3: n = 16 eyes, visit 4: n = 4 eyes. Green line: two follow-ups, blue line: three follow-ups, red line: four follow-ups. * p = 0.0182, ** p = 0.01, n.s. = statistically not significant
By considering the two major patient subgroups (chemical burns n = 6, post keratoplasty/graft rejection n = 3) a reduction of corneal neovascularization in both groups could also be detected (Fig. 2). Figure 3 demonstrates this effect for a patient suffering graft rejection.
Avastin eye drops potently inhibit corneal neovascularization in graft rejection (patient 16). Aggressive corneal neovascularization and persistent corneal epithel defects due to graft rejection prior to (a) and 4 weeks after initiation of additional treatment with bevacizumab eye drops (c). The corneal defects closed under the additional anti-VEGF therapy. No new corneal defects were observed. Pictures b and d are images of morphometrical analysis of pictures a and c respectively
Furthermore, we compared patients after transplantation of cultured limbal stem cells (fibrin gels), who received additional topical bevacizumab eye drops (n = 5) with patients who did not receive the bevacizumab therapy (n = 4). Patients with topical bevacizumab eye drops showed 5 months after limbal stem cell transplantation significantly less corneal neovascularization (p = 0.023, Figs. 4, 5). Due to the small number of patients who underwent this precedure at our clinic, the p-value should be regarded with caution.
Bevacizumab eye drops inhibit corneal neovascularization after limbal stem cell transplantation. Immediately after limbal stem cell transplantation, both patients showed almost no corneal neovascularization (a and c). Five months after surgery, the patient who received additional topical bevacizumab treatment (d) showed less new vessels than the patient who did not receive Avastin eye drops (b)
Avastin eye drops diminish the vessel diameter
We previously observed that Avastin eye drops seem to be able to reduce the perfusion of established vessels [7]. Therefore, we examined the vessel thickness before and during topical Avastin treatment. The mean reduction in vessel diameter under topical Avastin therapy was 24% within all 19 patients (Fig. 6). The strongest reduction in vessel diameter was seen in the keratoplasty group. The reduction rate was statistically significant within all patients (p = 0.01) and in the keratoplasty group (p = 0.005). Figure 7 shows a significant reduction for a patient from the chemical burn group.
Time course of blood vessel diameter reduction during antiangiogenic therapy
The strongest regression of corneal vessel thickness appeared to happen within the first 3 months of anti-VEGF treatment (Fig. 8). After that, the vessels seemed to reach a condition of equilibrium.
Discussion
Various inflammatory, infectious, degenerative, or traumatic disorders are associated with corneal neovascularization. This sight-threatening complication occurs when the balance between angiogenic and anti-angiogenic factors is tilted towards angiogenic molecules. The vascular endothelial growth factor (VEGF) has been shown to be up-regulated in inflamed and vascularized corneas in humans and in animal models [9, 10]. VEGF promotes several steps of angiogenesis and lymphangiogenesis, including proteolytic activities, endothelial cell proliferation, migration and capillary tube formation [11–13]. Bevacizumab is a humanized monoclonal antibody to VEGF, approved for intravenous administration for the treatment of colorectal cancer. A low incidence of significant adverse effects has been observed in systemic treatment, such as mild to moderate hypertension, increased rate of thrombosis and impaired wound healing [14]. In vitro studies have shown no significant side-effects in cells of the anterior segment of the eye [6]. Bevacizumab also showed no significant side-effects when injected intravitreally in the treatment of choroidal and retinal neovascularization [15].
Our results show that topical bevacizumab therapy for corneal neovascularization due to different corneal diseases was generally well-tolerated for up to 12 months treatment duration.
Kim et al. recently observed epitheliopathies and descemetocele in six of ten eyes under topical bevacizumab treatment. In our series, two of 30 eyes suffered from epitheliopathy. One eye showed a persistent epithelial defect immediately after pannectomy and limbal stem cell transplantation. One patient with a pre-existing corneal ulcer developed a spontaneous corneal perforation 5 months after start of additional Bevacizumab treatment. But 11 eyes (ten patients) with preexisting recurrent epithelial defects closed their epithelial defects under the topical Avastin therapy. None of the remaining patients suffered from new or increased epitheliopathy. The reason for the low incidence of these possible side effects may be that the Avastin eye drops Kim et al. used were more than twice as concentrated as the ones we used in our study (12.5 mg/ml versus 5 mg/ml, respectively 1.25% versus 0.5%). It is known that VEGF inhibitors may impair wound healing processes. This could happen in a dose-dependent manner. The exact mechanisms remain the subject of further studies. In addition, VEGF neutralization at the ocular surface might cause a neurotrophic keratopathy since VEGF is known to have neuroprotective effects [16]. Therefore, care should be taken in patients with epithelial defects and neurotrophic keratopathy. In our study, patients received Avastin eye drops from 1-ml syringes. In any case, injuries by the syringes should also be considered. Whether Avastin eye drops have other side-effects (such as reduced corneal sensitivity, altered corneal thickness, loss of endothelial cell etc.), not studied here, remains open to future studies.
Our results also suggest that topical application of bevacizumab (Avastin) can lead to reduction of the vessel thickness and inhibit corneal neovascularization. The effect of the eye drops was very variable. There are several possible explanations for these variations. First, we had a non-homogeneous study group composed of different underlying etiologies for corneal neovascularization. Second, the treatment regimen differed between the patients groups. Third, cytokines other than VEGF (such as fibroblast growth factor and transforming growth factor-α) which can induce corneal vascularization were not antagonized by bevacizumab [10, 17]. Fourth, bevacizumab is most efficient against actively growing corneal neovascularization (established corneal vessels do not depend on VEGF any more) [19]. The intensity of angiogenic stimulus was different even between patients with similar corneal diseases. Bevacizumab inhibited neovascularization significantly if administered early. Regression of established vessels occurred to a different degree in each patient. The reason, therefore, could be that in inflamed and vascularized corneas there is increased penetration of eye drops into and though the cornea [20]. Established vessels produce fewer inflammatory factors, and respond less well to the Avastin treatment. Nonetheless, we were able to show that almost all patients not responding to conventional anti-inflammatory treatment could benefit from the additional topical Avastin treatment. Despite the small number of patients who had undergone limbal autograft transplantation at our clinic, the comparison of with and without additional bevacizumab therapy clearly showed the benefit of the anti-VEGF therapy. In addition, patients with corneal neovascularization after low- and high-risk keratoplasty were able to benefit from Avastin treatment. It has recently been shown that antiangiogenic therapy both after low- and high-risk keratoplasty may progress graft survival [21, 22].
In summary, our preliminary results suggest that topical bevacizumab treatment seems to be a relatively safe and well-tolerated option for the treatment of progressive corneal neovascularization. Topical Avastin therapy may be used in cases of progressive corneal neovascularization not responding to conventional therapy. Future controlled prospective randomized trials are necessary to learn more about the long-term safety, tolerability and efficacy of Avastin eye drops.
References
Chang JH, Gabison EE, Kato T, Azar DT (2001) Corneal neovascularization. Curr Opin Ophthalmol 12:242–249, doi:10.1097/00055735-200108000-00002
Bock F, Koenig Y, Dietrich T, Zimmermann P, Baier M, Cursiefen C (2007) Inhibition of angiogenesis in the anterior chamber of the eye. Ophthalmologe 104:336–344, doi:10.1007/s00347-007-1512-2
Cursiefen C, Chen L, Saint-Geniez M et al (2006) Nonvascular VEGF receptor 3 expression by corneal epithelium maintains avascularity and vision. Proc Natl Acad Sci U S A 103:11405–11410, doi:10.1073/pnas.0506112103
Carmeliet P, Jain RK (2000) Angiogenesis in cancer and other diseases. Nature 407:249–257, doi:10.1038/35025220
Aiello LP, Avery RL, Arrigg PG et al (1994) Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med 331:1480–1487, doi:10.1056/NEJM199412013312203
Yoeruek E, Spitzer MS, Tatar O et al (2007) Safety profile of Bevacizumab on cultured human corneal cells. Cornea 26:977–982, doi:10.1097/ICO.0b013e3180de1d0a
Bock F, Koenig Y, Kruse F, Baier M, Cursiefen C (2008) Bevacizumab (Avastin) eye drops inhibit corneal neovascularization. Graefes Arch Clin Exp Ophthalmol 246:281–284, doi:10.1007/s00417-007-0684-4
Kim SW, Ha BJ, Kim EK, Tchah H, Kim TI (2008) The effect of topical Bevacizumab on corneal neovascularization. Ophthalmology 115:e33–e38, doi:10.1016/j.ophtha.2008.02.013
Philipp W, Speicher L, Humpel C (2000) Expression of vascular endothelial growth factor and its receptors in inflamed and vascularized human corneas. Invest Ophthalmol Vis Sci 41:2514–2522
Cursiefen C, Rummelt C, Küchle M (2000) Immunohistochemical localization of vascular endothelial growth factor, transforming growth factor alpha, and transforming growth factor beta1 in human corneas with neovascularization. Cornea 19:526–533. doi:10.1097/00003226-200007000-00025
Irigoyen JP, Moñoz-Cánoves P, Montero L et al (1999) The plasminogen activator system: biology and regulation. Cell Mol Life Sci 56:104–132, doi:10.1007/PL00000615
Blasi F (1999) Proteolysis, cell adhesion, chemotaxis, and invasiveness are regulated by the u-PA-u-PAR-PAI-1 system. Thromb Haemost 82:298–304
Bock F, Onderka J, Dietrich T et al (2007) Bevacizumab as a potent inhibitor of inflammatory corneal angiogenesis and lymphangiogenesis. Invest Ophthalmol Vis Sci 48:2545–2552, doi:10.1167/iovs.06-0570
Fernando NH, Hurwitz HI (2004) Targeted therapy of colorectal cancer: clinical experience with bevacizumab. Oncologist 9:11–18, doi:10.1634/theoncologist.9-suppl_1-11
Avery RL, Pieramici DJ, Rabena MD et al (2006) Intravitreal bevacizumab (Avastin) for neovascular age-related macular degeneration. Ophthalmology 113:363–372, doi:10.1016/j.ophtha.2005.11.019
Krum JM, Rosenstein JM (2004) New roles for VEGF in nervous tissue: beyond blood vessels. Exp Neurol 187:246–253, doi:10.1016/j.expneurol.2004.01.022
Soubrane G, Jerdan J, Karpouzas I et al (1990) Binding of basic fibroblast growth factor to normal and neovascularized rabbit cornea. Invest Ophthalmol Vis Sci 31:323–333
Bock F, Onderka J, Hos D, Horn F, Martus P, Cursiefen C (2008) Improved semiautomatic method for morphometry of angiogenesis and lymphangiogenesis in corneal flatmounts. Exp Eye Res 87:462–470, doi:10.1016/j.exer.2008.08.007
Cursiefen C, Rummelt C, Küchle M, Schlötzer-Schrehardt U (2003) Pericyte recruitment in human corneal angiogenesis. Br J Ophthalmol 87:101–106, doi:10.1136/bjo.87.1.101
Sadrai Z, Dastjerdi MH, Saban DR, Dana R (2008) Corneal penetration of topical bevacizumab (Avastin). ARVO poster, 2008.
Cursiefen C, Cao J, Chen L et al (2004) Inhibition of hemangiogenesis and lymphangiogenesis after normal-risk corneal transplantation by neutralizing VEGF promotes graft survival. Invest Ophthalmol Vis Sci 45(8):2666–2673, doi:10.1167/iovs.03-1380
Bachmann BO, Bock F, Wiegand SJ et al (2008) Promotion of graft survival by vascular endothelial growth factor a neutralization after high-risk corneal transplantation. Arch Ophthalmol 126(1):71–77, doi:10.1001/archopht.126.1.71
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koenig, Y., Bock, F., Horn, F. et al. Short- and long-term safety profile and efficacy of topical bevacizumab (Avastin®) eye drops against corneal neovascularization. Graefes Arch Clin Exp Ophthalmol 247, 1375–1382 (2009). https://doi.org/10.1007/s00417-009-1099-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-009-1099-1