Abstract
Purpose
To assess the usefulness of laser flare-cell photometry to quantify intraocular inflammation in patients with Behçet disease.
Methods
The study comprised 47 healthy individuals, 78 Behçet patients without ocular involvement, 54 Behçet patients with a uveitis attack and 53 Behçet patients with uveitis in clinical remission. A single observer assigned clinical scores to anterior chamber cells, vitreous haze, and fundus lesions in the attack group. Laser flare-cell photometry measurements were performed by another observer who was masked to the clinical findings. Fundus fluorescein angiography was performed only in the remission group, and fluorescein leakage was scored by a masked retina specialist. The risk of recurrent uveitis attack was analyzed in eyes with high versus low flare values in the remission group. Main outcome measures were anterior chamber flare in Behçet patients compared to the control group, and correlations of flare with clinical scores of intraocular inflammation and with fluorescein leakage. Mann-Whitney U-test, Spearman’s bivariate correlation test, linear regression method, and Kaplan-Meier method were used for statistical analyses.
Results
Mean flare was not increased in Behçet patients without ocular involvement. It was significantly higher in patients with Behçet uveitis both during attacks and in remission (P < 0.001 for each). A significant correlation was found between anterior chamber flare and anterior chamber cell score (rho = 0.705), vitreous haze score (rho = 0.588), and fundus score (rho = 0.464) in the attack group. In the remission group, there was a significant correlation between flare and fluorescein angiography leakage score, and the risk of recurrent uveitis attack was significantly higher in eyes with flare values >6 photons/msec than in eyes with flare values ≤6 photons/msec (right eyes, P < 0.001; left eyes, P = 0.0184).
Conclusions
Laser flare-cell photometry is a useful objective method in the quantitative assessment of intraocular inflammation in patients with Behçet uveitis. The use of this quantitative technique in clinical trials of Behçet uveitis may provide comparable data, as it gives an objective measure of intraocular inflammation. In clinical practice, it may reduce the need for fluorescein angiography because it seems to be especially useful in monitoring persistent retinal vascular leakage in patients who are clinically in remission.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Behçet disease (BD) is a chronic relapsing inflammatory disorder with multisystemic manifestations [1]. Patients with ocular involvement commonly have bilateral panuveitis and retinal vasculitis that affects all elements of the retinal vasculature [2]. The disease course is characterized by recurrent explosive uveitis attacks followed by a gradual resolution of intraocular inflammation [3]. Anterior or posterior segment of the eye, or more commonly both may be inflamed unilaterally or bilaterally at a given episode of activation. Acute nongranulomatous iridocyclitis, diffuse vitritis, retinitis, retinal edema, inflammatory sheathing of retinal veins, occlusion of retinal vessels, and papillitis are the typical ocular findings seen during uveitis attacks [2, 3]. Hypopyon formation, dense vitreous haze that obscures fundus details, extensive necrotizing retinopathy, and exudative retinal detachment may also be seen in severe attacks [2, 3]. The severity and frequency of uveitis attacks show individual variability and determine the visual prognosis [4]. Rapid resolution of anterior uveitis even in eyes with a hypopyon is a characteristic feature of Behçet uveitis [3]. Acute signs of posterior segment inflammation such as vitreous haze, inflammatory sheathing of retinal vessels, and retinitis also resolve within days to weeks, with or without treatment. Retinal hemorrhages take much longer to resolve, and debris of inflammatory cells remains attached to the vitreous fibers. Gliotic sheathing of retinal vessels, optic disc pallor, and variable atrophy, gliosis, and scarring of the retina are the typical sequelae of recurrent attacks [3]. In severe cases, posterior segment inflammation may not resolve completely between attacks, and the clinical picture during these periods may resemble intermediate uveitis, with slight hyperemia of the disc and diffuse vitreous cells and debris. Serious complications such as cystoid macular edema and neovascularization of the optic disc may develop in eyes with persistent inflammation [3, 5]. Fluorescein angiography (FA) has been traditionally used to monitor posterior segment involvement in patients with BD. Dye leakage from retinal vessels, capillaries and/or from the optic disc may be seen even during clinical remission and is considered as a sign of persistent retinal angiopathy [3, 6].
Laser flare-cell photometry (LFCP) is an automated technique that quantifies anterior segment inflammation [7]. It is an objective and noninvasive method that enables rapid and reproducible measurements of protein content and cells in the anterior chamber (AC) [7, 8]. Flare measurement has been shown to be useful in evaluating intraocular inflammation both in patients with anterior and with posterior uveitis [8–11]. A positive correlation has been found between flare values and complications of uveitis [12, 13]. Laser flare photometry studies have also shown an increase in aqueous flare intensity in a variety of noninflammatory posterior segment disorders such as diabetic retinopathy, retinal vein occlusion, and retinitis pigmentosa [14–16].
In the present study, we aimed to investigate the usefulness of LFCP to quantify intraocular inflammation in patients with Behçet uveitis.
Methods
The study was conducted at the Uveitis Service, Department of Ophthalmology, Istanbul Faculty of Medicine, Istanbul University. Approval was obtained from the local ethics committee, and all participants provided written informed consent prior to enrollment in the study.
The study comprised four groups of participants. Because of the influence of age on flare values [7], participants who were between 20 and 40 years of age were included in the study. All patients with BD, with or without ocular involvement, met the International Study Group criteria for the diagnosis of BD [17]. Patients who had previous ocular surgery were excluded. The first group consisted of healthy individuals who did not have any known systemic disease or ocular disorder other than a mild refractive error. The second group consisted of BD patients who did not have ocular involvement and were followed at the Division of Rheumatology, Department of Internal Medicine (non-ocular BD group). The third group consisted of BD patients who presented within 1 week after the onset of a uveitis attack (attack group). Only the eye with more recent attack or—in the case of simultaneous bilateral attacks—the eye with more severe inflammation was included in this group. Patients with a dense cataract or extensive posterior synechiae were not included in the study. The fourth group comprised patients with Behçet uveitis who had been clinically in remission bilaterally for at least 3 months (remission group). Only the eyes that had had a documented uveitis attack involving the posterior segment, and had clear media and adequate pupillary dilation that allowed FA, were included in this group. Patients with any clinical sign of ongoing inflammation were excluded from this group. Our study groups were not sex-matched, because no significant difference was found between genders in previous studies [18–20].
All consecutive study participants underwent a complete ocular examination by a single observer (ITT), who determined the eligibility of the participants for the uveitis and control groups. In the attack group, the same observer assigned clinical scores of intraocular inflammation before LFCP measurement [21, 22]. Anterior chamber cells were scored before pupillary dilation, and a modification was made to the scoring system by adding 5 + for hypopyon formation [21]. Vitreous haze and fundus findings were scored after pupillary dilation with tropicamide 1% and phenylephrine 2.5% [22]. The fundus scoring sheet developed by BenEzra et al. [22] was used for the scoring of fundus findings. In this sheet, the fundus is divided into four pre-equatorial crescent-shaped zones and four post-equatorial pie-shaped zones, by horizontal and vertical lines passing through the optic disc. Active retinal vasculitis, chorioretinal infiltrates, and neovascularizations are recorded as present or absent in each of these eight zones. Macular edema (0,1), neovascularization of the optic disc (0,1), and papillitis (0–3) are scored separately.
Laser flare-cell measurements were performed by another observer (KC), who was masked to the clinical findings and the clinical scores. The KOWA FC-2000 (Kowa Company, Ltd, Tokyo, Japan) was used for recordings. Measurements were performed 1 hour after pupillary dilation. Only the flare mode was used in all eyes in the remission and control groups. Measurements with “Cell”, “S/N”, or “BG” error codes were not stored. Seven readings were obtained, for which the difference between background values was less than 15%. The highest and lowest values were discarded, and the machine automatically calculated the mean and standard deviation of the remaining five readings of flare. The mean flare value, expressed as photon counts per millisecond (photons/msec), was recorded for study purposes. The flare-cell mode was used for the measurement of flare and cells in eyes in the attack group. Seven measurements were performed that counted cells in at least 100 of 128 blocks. Measurements were not stored when the number of blocks counted was less than 100, or when “S/N” or “BG” flare error codes were seen. The number of cells under good measurement conditions was converted automatically by the machine to the number of cells in a fixed volume of 0.5 cubic mm. The highest and lowest counts were deleted, and the mean cell count was obtained in a similar fashion described for flare. When there were three or more “C” error codes on flare display in the flare-cell mode, flare measurements were repeated until at least five measurements were obtained without an error code. When it was not possible to obtain a cell measurement in the attack group, only the flare mode was used, and measurements with a “S/N” and/or “Cell” error code had to be used, because it was not possible to obtain a measurement without an error code in such eyes.
After LFCP, FA was performed on the same day in all patients in the remission group. Superior, inferior, nasal, and temporal periphery, as well as the macula and optic disc, were swept through the late phase of angiography. The angiograms were evaluated later by a retina specialist (NK) who was masked to the flare values. The retina between the superior temporal and superior nasal major retinal veins was defined as the superior periphery, the retina between the inferior temporal and inferior nasal retinal veins was defined as the inferior periphery, the retina between the superior and inferior nasal veins was defined as the nasal periphery, and the retina peripheral to the macula between the superior and inferior temporal major retinal veins was defined as the temporal periphery. Presence or absence of vascular and/or capillary leakage in late frames of the angiogram was graded as 0 = absent and 1+ = present (Fig. 1). Leakage at the optic disc, at the macula, and at superior, inferior, temporal, and nasal periphery was recorded, giving a maximum score of 6+ if leakage was found in all. Hyperfluorescence due to window defects or hypofluorescence due to blocking or nonperfusion were not taken into account.
Primary outcome measures were AC flare in BD patients compared to the control group, correlation of AC flare and cell counts with clinical scores of intraocular inflammation during uveitis attacks, and correlation between AC flare and FA leakage during clinical remission. Data was analyzed using SPSS 11.5 for Windows (SPSS Inc., Chicago, IL, USA). Only the left eyes of the patients in the healthy control group, non-ocular BD group, and remission group were used for statistical comparison of flare values. The non-parametric Mann-Whitney U-test was used for comparison of patients’ age and flare values. Spearman’s bivariate correlation test was used to calculate correlation coefficients (rho). Positive correlation values were also tested using linear regression method.
The study was not primarily designed to analyze the longitudinal follow-up of the patients. However, at the time of data analysis we retrospectively reviewed the charts of BD patients and analyzed two additional data: flare values at 3 months in the attack group, and recurrence of uveitis attacks in the remission group. The Kaplan-Meier method was used in order to estimate the risk of a recurrent uveitis attack in the remission group. The log-rank test was used to perform comparison of survival curves between eyes with high (>6 photons/msec) and low (≤6 photons/msec) flare readings. P value <0.05 was considered significant.
Results
Between November 2005 and December 2007, 232 participants were enrolled in the study. There were 47 individuals (15 men and 32 women) in the healthy control group, 78 patients (32 men and 46 women) in the non-ocular BD group, 54 patients (40 men and 14 women) in the attack group, and 53 patients (37 men and 16 women) in the remission group. The mean age was 27.3 ± 5.3 years in healthy controls, 31.3 ± 5.6 years in the non-ocular BD group, 27.7 ± 4.9 years in the attack group, and 29.4 ± 5.7 years in the remission group. Patients in the non-ocular BD group were significantly older than patients in the attack group (P < 0.001) and healthy individuals (P < 0.001). Comparison between the remaining groups did not reveal significant difference in the mean age. There were 54 eyes (30 right and 24 left eyes) in the attack group and 99 eyes (49 right and 50 left eyes) in the remission group that met the inclusion criteria.
Visual acuity, clinical scores of intraocular inflammation, and anterior chamber flare and cell count measured by LFCP in the attack group are shown in Table 1. The presence of focal posterior synechiae (two eyes) or focal mild posterior sub-capsular lens opacity (seven eyes) did not prevent the assessment of vitreous haze or fundus lesions in this group. However, three eyes had ≥ 4+ vitreous haze and fundus scoring could not be done. Reliable cell measurements could not be obtained in six eyes in this group, including three eyes with a hypopyon, two eyes with 4+ cells, and one eye with a shallow AC. Missing fundus scores and cell measurements were analyzed as missing data.
Visual acuity, time interval since last uveitis attack, FA leakage score, and anterior chamber flare measured by LFCP in the remission group are shown in Table 2. Mild posterior capsular lens opacity was present in four patients (bilaterally in three patients and in the right eye of one patient) in the remission group. However, it was possible to obtain good-quality fluorescein angiograms in all. None of the patients in this group had posterior synechiae. Flare values in the right and left eyes of the healthy controls and Behçet patients without ocular involvement are shown in Table 3.
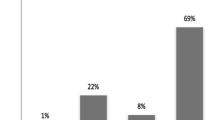
Statistical analysis of flare values in the left eyes of the study groups showed that there was no significant difference between the flare values of the healthy control and non-ocular BD groups (P = 0.256). Mean flare value in the remission group was significantly higher than in the healthy control group and the non-ocular BD group (P < 0.001 for each comparison). Flare readings showed a wide range in the attack group and the median flare was 22.1 photons/msec. The mean flare value of this group was significantly higher than those of all other groups (P < 0.001 for each comparison) (Fig. 2).
In the attack group, anterior chamber flare measured with LFCP showed a significant correlation with the cell count (rho = 0.538, P < 0.001) and with all clinical scores, including AC cell score (rho = 0.705, P < 0.001), vitreous haze score (rho = 0.588, P < 0.001), and fundus score (rho = 0.464, P = 0.001). Cell count by LFCP had a significant correlation with the AC cell score (rho = 0.866, P < 0.001), but not with the vitreous haze score (rho = 0.277, P = 0.057), or the fundus score (rho = 0.188, P = 0.206). Linear regression analysis revealed similar results.
Flare readings were obtained at 3 months in 42 patients in the attack group who had regular follow-up visits. Figure 3 shows reduction in flare values following treatment in this subgroup of patients. Only one patient had a recurrent uveitis attack within 3 months, and had the highest flare value (32 photons/msec) at 3 months.
In the remission group, there was no FA leakage in 25 of 49 right eyes and 22 of 50 left eyes. Figure 4 shows the scatter graph of FA leakage score and flare values in all eyes in the remission group. For a flare value of >6 photons/msec, the sensitivity of LFCP flare measurement in detecting FA leakage was 67% and its specificity was 98%. A significant correlation was found between the FA leakage score and the LFCP flare values, both in the right eyes (rho = 0.688, P = 0.01) and in the left eyes (rho = 0.825, P = 0.01). Linear regression analysis of the correlation between the flare values and FA leakage score revealed an R coefficient of 0.869 in the right eyes and 0.814 in the left eyes.
Thirty patients (57 eyes) in the remission group had follow-up after enrollment in the study. In this subgroup, flare was higher than 6 photons/msec in 11 of 28 right eyes and in 17 of 29 left eyes. Eight right eyes and seven left eyes had a recurrent uveitis attack during follow-up. Kaplan-Meier survival analysis in both the right and the left eyes of these 30 patients in the remission group showed that the risk of recurrent uveitis attack was significantly higher in eyes with high flare values than in eyes with low flare values (right eyes, Log-Rank = 13.05, P < 0.001; left eyes, Log-Rank = 5.56, P = 0.0184) (Fig. 5). Systemic treatment had not been discontinued in any of the patients who had recurrent uveitis attacks.
Discussion
We undertook this project to investigate whether LFCP is a useful tool to quantify intraocular inflammation in patients with Behçet uveitis. We found that patients with BD without ocular involvement did not have a sub-clinical flare rise; AC flare and cell count had a significant correlation with the clinical score of AC cells; and flare values also showed a significant correlation with the clinical scores of posterior segment inflammation and leakage on FA. Our results suggest that flare value measured by LFCP is an objective marker of overall inflammatory activity in the eye in BD. Furthermore, we found that sub-clinical high flare values were associated with a higher risk of recurrent uveitis attacks.
Accuracy and reproducibility of laser flare photometry have been proven in previous studies [7, 18, 19, 23]. It identifies small differences in aqueous humor opalescence and detects clinically relevant flare in eyes without detectable flare at slit-lamp examination. Previous studies have shown the influence of age and pupillary dilation on flare values in healthy individuals [18–20]. Therefore, participants between 20 and 40 years of age were included in the study. Our results in healthy individuals are consistent with those reported in the same age range [18, 19].
Okamoto and associates reported that flare measured by LFCP was significantly higher in psoriasis patients without clinical ocular involvement than in healthy controls [24]. A sub-clinical flare rise may be expected in BD patients as well, because the underlying pathology is vasculitis that affects all organ systems. Patients with BD without ocular involvement were compared to healthy controls to test this hypothesis. We did not find any significant difference in flare values between these groups. Although patients in the non-ocular BD group were significantly older than healthy individuals, they did not have higher flare values. Changes in age within the 20–40 years range did not seem to affect the flare values.
The current scoring systems that are used to monitor patients with uveitis are based on the grading of inflammatory signs separately [21, 22]. Although it may not be a problem in isolated anterior or posterior uveitic entities, it becomes confusing in patients with panuveitis and even more so in patients with Behçet uveitis who have variable involvement of the anterior and posterior segments of the eye. In clinical studies of Behçet uveitis, the outcome measures that assessed effect of a treatment have been variable, including the evolution of individual clinical signs [25], the frequency of uveitis attacks [26], and the score of only fundus findings [27]. Laser flare-cell photometry may provide a tool to collect comparable data. Schalnus and Ohrloff reported that the flare values increased in both anterior and posterior uveitis compared to normal eyes, but did not significantly differ between them [28]. On the other hand, the authors found that the diffusion coefficient of blood–aqueous barrier was significantly increased in eyes with anterior uveitis compared to normal eyes and eyes with posterior uveitis, suggesting that the proteins may enter the aqueous from the posterior segment in eyes with posterior uveitis [28]. In a study of Guex-Croiser and associates, blood–aqueous barrier disruption was found to be severe in BD, moderate in pars planitis and posterior sarcoidosis, and close to normal in toxoplasmosis and birdshot chorioretinopathy [9]. The authors commented that the aqueous flare in BD was equal to or higher than in anterior uveitis; however, the mean flare value reported in their study (331.8 ± 47.7 photons/msec) was based on data from only four patients. Relative contribution of anterior and posterior segment of the eye to the diffusion of proteins into the aqueous humor may be variable during uveitis attacks in patients with BD. In the present study, standard deviation was very small in the control groups; whereas in the attack group, even after the exclusion of outliers, flare values showed a wide range reflecting the variable severity of uveitis attacks, a well-known feature of BD. The prognostic significance of high flare during uveitis attacks was not analyzed in the present study. Gonzales and associates reported a significant association between high laser flare photometry values and complications of uveitis in a heterogenous population of patients with various uveitic entities [12]. In their series, mean flare was higher than 20 photons/msec in all subgroups of patients with uveitic complications. Prognostic implications of flare during uveitis attacks of patients with BD may be revealed after long-term follow-up. Takeuchi and associates reported that more than three attacks per year, strong vitreous opacity and exudates within the retinal vascular arcades during uveitis attacks were significant risk factors for poor visual outcome in patients with BD who had a follow-up of at least 5 years [29]. Patients included in the present study have not had long-term follow-up yet.
In our study, we found a strong correlation between flare values and posterior segment inflammatory signs, especially vitreous haze. It has also been our clinical impression that the vitreous haze during attacks was associated with diffuse retinal vascular damage and thus determined the severity of ocular involvement in our patients. Clinical assessment and grading of inflammatory findings are of utmost importance in the management of uveitis patients, and we do not suggest the use of LFCP to replace clinical grading. The present study suggests that AC flare may be a cumulative measure of intraocular inflammation, and flare measurement with LFCP may be used as an objective and quantitative method of monitoring uveitis in patients with BD. Although the quantification of AC cells by LFCP had a strong correlation with the clinical grading of AC cells, this technique seems to need further improvement, because we had difficulty in obtaining reliable measurements at high clinical grades and in eyes with a shallow AC. Furthermore, the correlation of flare was stronger with the clinical grade of AC cells than with the cell counts obtained by LFCP (rho = 0.705 vs rho = 0.538). We believe that the clinical grading of cells by an experienced examiner is still more reliable than LFCP cell count.
Chronic anterior uveitis is not a feature of BD and signs of persistent inflammation are usually sought in the posterior segment after the resolution of acute attacks. Our findings confirm the sensitivity of LFCP, and may suggest its usefulness especially in eyes with poor visualization of the posterior segment. The strong correlation of flare values with FA leakage found in this study is consistent with the previous reports on the correlation of flare with FA findings in diabetic retinopathy and retinal vein occlusion [14, 15]. Fundus FA has been the gold standard in the evaluation of posterior segment involvement in patients with Behçet uveitis [3, 6, 30]. Although indocyanin green angiography has shown choroidal involvement, FA remains the main tool to detect retinal vasculopathy [31–33]. Fundus FA is still irreplaceable in the assessment of retinal nonperfusion, i.e., occlusive nature of retinal vasculitis, as well as in the detection of other pathologies such as neovascularizations and retinal pigment epithelial defects. In BD patients, FA is performed in order to document macular ischemia, scarring, or edema; to detect retinal vascular occlusions, retinal nonperfusion, and retinal neovascularizations that may require laser photocoagulation; and to show the severity and extent of retinal vasculitis, which may be seen in the form of staining of vessel walls and dye leakage from large and small retinal vessels as well as from papillary and retinal capillaries [3, 6, 30–33]. In our practice, the most common use of FA in BD patients is for the purpose of detecting persistent capillary leakage after the resolution of acute inflammatory signs. The use of FA during uveitis attacks is relatively limited because of the vitreous haze. On the other hand, our therapeutic decisions are mostly based on the FA findings after clinical remission is achieved. Persistent dye leakage on FA may indicate ongoing disease and the need for a more aggressive and prolonged systemic therapy. We have previously reported that FA guided our diagnosis and treatment in BD patients with neovascularization of the optic disc; and that 87% of the eyes with disc neovascularization had diffuse capillary leakage on FA [5]. Although the site of leakage can only be seen with FA, the strong correlation of flare values with FA leakage found in this study suggests that this quick and noninvasive method may be reliably used to quantify changes in the blood-ocular barrier functions in the follow-up of patients with BD. Guex-Croiser and associates reported that a flare rise of more than 20% predicted recurrences in patients with posterior uveitis in quiescence [9]. The predictive value of sub-clinical flare rise was reported to be 100% in BD [9]. In our study, mean flare was significantly higher in the remission group than in the control groups; however, absolute flare values were relatively low and did not exceed 21 photons/msec. Although these flare values are not generally associated with an increased risk of uveitic complications, the Kaplan-Meier method used in our study showed that even flare values higher than 6 photons/msec were associated with a higher risk of recurrent uveitis attacks in patients with BD.
In conclusion, LFCP is a useful method in the quantitative assessment of anterior and posterior segment inflammation in patients with Behçet uveitis. We believe that the use of this quantitative technique in clinical trials of Behçet uveitis may provide comparable data, as it gives an objective measure of intraocular inflammation. In clinical practice, it may reduce the need for fluorescein angiography because it seems to be especially useful in monitoring persistent retinal vascular leakage in patients who are clinically in remission. Further studies in large number of patients are needed to confirm the prognostic significance of flare in patients with Behçet uveitis.
References
Yazici H, Yurdakul S, Hamuryudan V (1999) Behçet’s syndrome. Curr Opin Rheumatol 11:53–57
Tugal-Tutkun I, Onal S, Altan-Yaycioglu R, Altunbas HH, Urgancioglu M (2004) Uveitis in Behçet disease: An analysis of 880 patients. Am J Ophthalmol 138:373–380
Mishima S, Masuda K, Izawa Y, Mochizuki M, Namba K (1979) The eighth Frederick H Verhoeff lecture. presented by Saiichi Mishima, MD Behcet’s disease in Japan: ophthalmologic aspects. Trans Am Ophthalmol Soc 77:225–279
Takeuchi M, Hokama H, Tsukahara R et al (2005) Risk and prognostic factors of poor visual outcome in Behçet’s disease with ocular involvement. Graefes Arch Clin Exp Ophthalmol 243:1147–1152
Tugal-Tutkun I, Onal S, Altan-Yaycioglu R, Kir N, Urgancioglu M (2006) Neovascularization of the optic disc in Behçet’s disease. Jpn J Ophthalmol 50:256–265
Mochizuki M, Akduman L, Nussenblatt RB (1996) Behçet disease. In: Pepose JS, Holland GN, Wilhelmus KR (eds) Ocular infection & immunity. Mosby, St Louis, pp 663–675
Ladas JG, Wheeler NC, Morhun PJ, Rimmer SO, Holland GN (2005) Laser flare-cell photometry: Methodology and clinical applications. Surv Ophthalmol 50:27–47
Guex-Crosier Y, Pittet N, Herbort CP (1994) Evaluation of laser flare-cell photometry in the appraisal and management of intraocular inflammation in uveitis. Ophthalmology 101:728–735
Guex-Crosier Y, Pittet N, Herbort CP (1995) Sensitivity of laser flare photometry to monitor inflammation in uveitis of the posterior segment. Ophthalmology 102:613–621
Herbort CP, Guex-Crosier Y, de Ancos E, Pittet N (1997) Use of laser flare photometry to assess and monitor inflammation in uveitis. Ophthalmology 104:64–72
Magone MT, Nussenblatt RB, Whitcup SM (1997) Elevation of laser flare photometry in patients with cytomegalovirus retinitis and AIDS. Am J Ophthalmol 124:190–198
Gonzales CA, Ladas JG, Davis JL, Feuer WJ, Holland GN (2001) Relationships between laser flare photometry values and complications of uveitis. Arch Ophthalmol 119:1763–1769
Davis JL, Dacanay LM, Holland GN, Berrocal AM, Giese MS, Feuer WJ (2003) Laser flare photometry and complications of uveitis in children. Am J Ophthalmol 135:763–771
Nguyen NX, Schonherr U, Kuchle M (1995) Aqueous flare and retinal capillary changes in eyes with diabetic retinopathy. Ophthalmologica 209:145–148
Nguyen NX, Kuchle M (1993) Aqueous flare and cells in eyes with retinal vein occlusion–correlation with retinal fluorescein angiographic findings. Br J Ophthalmol 77:280–283
Kuchle M, Nguyen NX, Martus P, Freissler K, Schalnus R (1998) Aqueous flare in retinitis pigmentosa. Graefes Arch Clin Exp Ophthalmol 236:426–433
International Study Group for Behçet’s disease (1990) Criteria for diagnosis of Behçet’s disease. Lancet 335:1078–1080
Shah SM, Spalton DJ, Smith SE (1991) Measurement of aqueous cells and flare in normal eyes. Br J Ophthalmol 75:348–352
Guillen-Monterrubio OM, Hartikainen J, Taskinen K, Saari KM (1997) Quantitative determination of aqueous flare and cells in healthy eyes. Acta Ophthalmol Scand 75:58–62
Onodera T, Gimbel HV, DeBroff BM (1993) Aqueous flare and cell number in healthy eyes of Caucasians. Jpn J Ophthalmol 37:445–451
Jabs DA, Nussenblatt RB, Rosenbaum JT (2005) Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol 140:509–516
BenEzra D, Forrester JV, Nussenblatt RB, Tabbara K, Timonen P (1991) Uveitis scoring system. Springer Verlag, Berlin
El-Maghraby A, Marzouki A, Matheen TM, Souchek J, Van der Karr M (1992) Reproducibility and validity of laser flare/cell meter measurements as an objective method of assessing intraocular inflammation. Arch Ophthalmol 110:960–962
Okamoto F, Umebayasi Y, Ohtsuka F, Hommura S (2001) Factors associated with increased aqueous flare in psoriasis. Jpn J Ophthalmol 45:172–176
Sfikakis PP, Kaklamanis PH, Elezoglou A et al (2004) Infliximab for recurrent, sight-threatening ocular inflammation in Adamantiades-Behçet diease. Ann Intern Med 140:404–406
Tugal-Tutkun I, Mudun A, Urgancioglu M et al (2005) Efficacy of infliximab in the treatment of uveitis that is resistant to treatment with the combination of azathioprine, cyclosporine, and corticosteroids in Behçet’s disease. Arthritis Rheum 52:2478–2484
Kötter I, Zierhut M, Eckstein AK et al (2003) Human recombinant interferon alfa-2a for the treatment of Bençet’s disease with sight threatening posterior or panuveitis. Br J Ophthalmol 87:423–431
Schalnus RW, Ohrloff C (1998) Vergleichende Lasertyndallometrie und Fluorophotometrie bei anteriorer und posteriorer Uveitis. Ophthalmologe 95:3–7
Takeuchi M, Hokama H, Tsukahara R et al (2005) Risk and prognostic factors of poor visual outcome in Behcet’s disease with ocular involvement. Graefes Arch Clin Exp Ophthalmol 243:1147–1152
Atmaca LS (1989) Fundus changes associated with Behçet’s disease. Graefes Arch Clin Exp Ophthalmol 227:340–344
Klaeger A, Tran AT, Hiroz CA, Morisod L, Herbort CP (2000) Indocyanine green angiography in Behçet’s uveitis. Retina 20:309–314
Gedik S, Akova YA, Yilmaz G, Bozbeyoglu S (2005) Indocyanine green and fundus fluorescein angiographic findings in patients with active ocular Behçet’s disease. Ocul Immunol Inflamm 13:51–58
Atmaca LS, Sonmez PA (2003) Fluorescein and indocyanine green angiography findings in Behçet’s disease. Br J Ophthalmol 87:1466–1468
Acknowledgements
This study was supported by the Research Fund of Istanbul University (Project number 53/03062005)
We thank Professor Rian Disci for statistical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was presented in part at the 12th International Conference on Behçet’s Disease, Lisbon, Portugal, 19–23 September, 2006
Financial disclosures: None
The authors have full control of all primary data and they agree to allow Graefes Archive for Clinical and Experimental Ophthalmology to review their data upon request.
Rights and permissions
About this article
Cite this article
Tugal-Tutkun, I., Cingü, K., Kir, N. et al. Use of laser flare-cell photometry to quantify intraocular inflammation in patients with Behçet Uveitis. Graefes Arch Clin Exp Ophthalmol 246, 1169–1177 (2008). https://doi.org/10.1007/s00417-008-0823-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-008-0823-6