Abstract
Purpose
To investigate the toxic effects of perfusion of intravitreal melphalan during vitrectomy on the rabbit retina.
Methods
We performed electoretinography (ERG) in 18 eyes of 18 healthy albino rabbits before and after intraocular melphalan perfusion at concentrations of 5-, 10-, and 20-μg/ml during pars plana vitrectomy. Fellow eyes that underwent vitrectomy without melphalan served as controls. The histopathologic retinal changes were observed in both eyes of two rabbits from each group.
Results
In the 5-μg/ml perfusion group, the ERGs and histology showed no substantial changes compared with control fellow eyes during 28 days postoperatively. In the 10- and 20-μg/ml groups, the mean a-wave amplitude decreased to 52% and 31% respectively of the fellow eye; the mean b-wave amplitude decreased to 52% and 19% respectively. However, the peak implicit time of the a- and b-waves did not significantly differ in the 10- and 20-μg/ml groups during 28 days postoperatively. Histologic sections showed necrosis of the inner nuclear layer and thinning of the outer nuclear layer in the 10-μg/ml group. Loss of the outer nuclear layer and the photoreceptor layer and necrosis of the inner nuclear layer were observed in the 20-μg/ml group.
Conclusion
The intravitreal 5-μg/ml melphalan perfusion during vitrectomy appears to be nontoxic to the retina. This therapeutic modality might be a potential treatment for retinoblastoma with vitreous seeding.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Retinoblastoma, a heritable tumor, is the most common intraocular malignancy occurring in children under 15 years of age, with a frequency of approximately one in every 15,000 live births. The RB1 gene was not only the first human cancer gene cloned but also was the first of a whole class of human cancer “suppressor genes.” In the dominantly inherited form of retinoblastoma, one mutation is inherited via the germline, and the second occurs in the somatic cells. In the sporadic form, both mutations occur in the somatic cells. Although 60% of all patients have the sporadic form, the other 40% have a form of the disease with a mutation of RB1 in the germline [1].
There have been great advances in the management of retinoblastoma. External beam radiotherapy [2–5] used to be the first treatment choice for intraocular retinoblastoma based on the Reese–Ellsworth group classification [6, 7]. Strong evidence indicated that the incidence of a second malignant neoplasm increased in genetically predisposed patients treated with external beam radiotherapy. To date, systemic chemotherapy [8–11] combined with sequential aggressive local therapy has become the therapy of choice for intraocular retinoblastoma in groups A to D of the International Classification for Intraocular Retinoblastoma [12]. Although the tumor is confined to the retina without seeding in groups A and B, the tumor has spread to the vitreous and subretinal space in groups C and D. Group E eyes have been destroyed by the tumor, and enucleation is still the first-choice therapy. Group C eyes with local seeding can be salvaged at a rate close to 70%. However, group D eyes with diffuse dissemination have an unfavorable survival rate for ocular preservation.
To improve the salvage rate in groups C and D, Yamane et al. developed selective ophthalmic arterial infusion therapy [13] using a balloon catheter and intravitreal injection of melphalan [14] combined with ocular hyperthermia [15]. These methods, which were developed in a study group funded by a grant from the Health and Welfare Ministry, are now used routinely at the National Cancer Center Hospital, Tokyo, Japan. These treatments have achieved a rate of ocular preservation of 51.3% during the recent decade using intravitreal melphalan injection after ophthalmic arterial infusion combined with ocular hyperthermia [14]. However, the optimal dose of intravitreal melphalan, which kills the tumor but has no adverse retinal effects, has not been determined [16–18]. Although selective ophthalmic arterial infusion and intravitreal injection of melphalan have fewer systemic side effects, intravitreal drug delivery may be insufficient in cases with vitreous seeding because of the blood-retinal-barrier and uneven intravitreal distribution [19] of the anticancer drug. To overcome these barriers, intravitreal melphalan infusion during vitrectomy is expected to be the most effective treatment for cases with vitreous seeding.
In the current study, we observed the histologic and functional retinal changes after intraocular infusion of melphalan during pars plana vitrectomy in healthy rabbits.
Material and methods
Animals
Eighteen adult albino rabbits (weight, 2–3 kg) were used in this study, which was conducted in accordance with the Association for Research in Vision and Ophthalmology Statement for the Use of Animals in Ophthalmic and Vision Research. The animals were anesthetized with intramuscular ketamine (35 mg/kg) and xylazine (5 mg/kg) before all procedures. Topical anesthesia was applied using proparacaine (0.5%), and the pupils were dilated with 0.5% phenylephrine and 0.5% tropicamide. All eyes were examined using a slit lamp and indirect ophthalmoscopy at the beginning of the procedure and on days 3, 7, 14, and 28 after vitrectomy. Animals with corneal or lens opacity or retinal damage were excluded from the study.
Pars plana vitrectomy
The 18 animals underwent bilateral pars plana vitrectomy. The procedure in the left eyes was performed with intraocular irrigation of melphalan at various concentrations, and the right eyes were irrigated with sterile intraocular irrigating solution (Opeguard-MA, Senju Pharmaceutical, Osaka, Japan) as a control. After an infusion cannula was placed at the sclera 1.5 mm from the limbus, the cutter was inserted into the vitreous through the sclerotomy 1.5 mm from the limbus. Under microscopic illumination and fundus contact lens, we performed core vitrectomy using Microvit (Alcon, Fort Worth, TX, USA). The vitreous cavity was perfused with irrigating solution containing melphalan at concentrations of 5-, 10-, and 20-μg/ml in the left eyes. After core vitrectomy, the vitreous gel was removed surgically as completely as possible without damaging the lens. The left eyes were irrigated for 1 hour with melphalan solution, which was then washed from the vitreous cavity with the irrigating solution without melphalan for 10 minutes. The temperature of the irrigation solution was maintained at 37 ± 1 degrees C using a blood warming device (HB-W5, Hakko Medical, Nagano, Japan). The right eyes were irrigated only with intraocular irrigating solution for 70 minutes.
Although both eyes underwent vitreous surgery, one eye was perfused by balanced salt solution. The vision of at least one eye was maintained in all treated animals until the end of the experiment.
Electroretinography analysis
The electroretinograms (ERGs) were recorded just before vitrectomy and on postoperative days 3, 7, 14, and 28. An ERG was performed using a synchronized trigger and summing amplifier (Purimus, Mayo, Nagoya, Japan) with a stimulation device (LS-W, Mayo). A white light-emitting diode built-in contact type electrode (Mayo) was used as a corneal bipolar electrode. The negative and ground electrodes were placed in the subcutaneous skin of the forehead and the earlobe. After the rabbits were anesthetized, the pupils were dilated with 1% tropicamide and 2.5% phenylephrine hydrochloride; the rabbits were dark adapted for at least 60 minutes before the recordings. Measurement of the ERGs was subject to the guidelines of the International Society for Clinical Electrophysiology of Vision [20]. The stimulus intensity and length of the maximal response were set at 8,000 cd/m2 and 0.5 msec; the rod response was set in 316.2 cd/m2 and 0.03 msec. The amplitude and peak implicit time were measured, and the ratio of the value in the melphalan-irrigated eye to that in the control eye (melphalan: control) was calculated. Dose-toxic response functions for each density measures were analyzed by repeated measures ANOVA. A t-test also was used to assess whether the amplitude and peak implicit ratio of the treated eye to the control eye had changed after melphalan perfusion. P < 0.05 was considered significant.
Histologic evaluation
All animals were killed with an intravenous injection of pentobarbital overdose while under deep anesthesia on day 28 after surgery. Both eyes of two rabbits from each group were enucleated, grossly examined, fixed in Davidson solution (95% ethanol, 10% formaldehyde, acetic acid, and distilled water) and embedded in paraffin, sectioned, and stained with hematoxylin and eosin for light microscopy examination.
Results
Bilateral ERG before treatment
Before surgery, we compared the ERGs in both eyes. The a-wave amplitude and the peak implicit rates of the eye that was to undergo melphalan perfusion and those of the fellow eyes ranged from 98.8 ± 4.1% to 105.0 ± 13.3% and 97.1 ± 4.7% to 106.1 ± 5.7% respectively (Figs. 1, 2). There were no significant differences between the eyes. The b-wave amplitude and the peak implicit rates ranged from 98.9 ± 3.9% to 99.0 ± 6.0% and from 96.6 ± 6.5% to 106.5 ± 3.7% respectively (Figs. 1, 3). There were no significant differences between the eyes.
The a-wave and b-wave elicited by standard flash before and after melphalan perfusion in a representative case from each group. The amplitudes of the a- and b- waves with the 5-μg/ml perfusion of melphalan (left column) show no changes on postoperative days 3, 7, 14, and 28 days compared with the pretreatment status. The amplitudes of the a- and b-waves with the 10-μg/ml melphalan perfusion (middle column) decrease to 68 and 65% of the pretreatment status on postoperative day 3, and remain approximately 50% on days 7, 14, and 28. The amplitude of the a-wave with the 20-μg/ml perfusion (right column) decreases approximately 46%, and gradually declines up to 30% on days 7, 15, and 28. The amplitude of the b-wave decreases to 46% on postoperative day 3, and gradually declines up to 18% on days 7, 14, and 28. In all cases, the amplitudes of the a- and b-waves are normal in the control fellow eyes
The mean amplitude ratios of the a-wave (melphalan:control) in the left column and the peak implicit ratio of the a-wave in the right column before and after vitrectomy with melphalan perfusion in five albino rabbits from each group (*p < 0.05). Although the ERG amplitude of the a-wave (squares) in the 5-μg/ml perfusion group does not change significantly from the pretreatment status on days 3, 7, 14, and 28, the amplitude does decrease significantly from the pretreatment status in the 10-μg (triangles) and 20-μg (circles) groups. The amplitudes of those two groups gradually decrease from day 3 to days 7 or 14, and do not recover until day 28. The amplitude rates in each group are summarized in Table 1. The peak implicit rates of the a-wave in the 5- and 10-μg perfusion groups do not change significantly until postoperative day 28. The peak implicit rate of the a-wave in the 20-μg perfusion group tends to prolong, but the difference does not reach significance
The mean amplitude ratio (melphalan: control) (left column) and peak implicit ratio (right column) of the b-wave before and after vitrectomy with melphalan perfusion in five albino rabbits from each group (*p < 0.05). Although the amplitude of the b-wave (squares) in the 5 μg/ml perfusion group does not change significantly from the pretreatment status on postoperative days 3, 7, 14, and 28, the amplitude does decrease significantly from the pretreatment status in the 10-μg group (triangles) and the 20-μg group (circles). The amplitudes of those two groups decrease gradually from day 3 to days 7 or 14 and do not recover until day 28. The peak implicit rates of the b-wave in the 5- and 10-μg perfusion groups do not change significantly until postoperative day 28. In the 20-μg perfusion group, the peak implicit rates tend to prolong, but the difference does not reach significance
5-μg/ml melphalan perfusion group
Compared with the pretreatment status, the ERG amplitudes and peak implicit rates of the a- and b-waves in six rabbits did not change significantly from preoperatively to postoperatively on days 3, 7, 14, and 28 (Figs. 1, 2, 3). The ERG data are shown in Table 1.
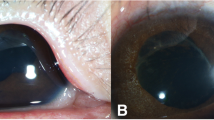
Light microscopy of a histologic section from treated eyes of two rabbits showed normal structures in all retinal layers. As a neural component, the ganglion cells, the inner and outer nuclear layers, and the photoreceptor inner and outer segments appeared normal, and did not differ from the fellow eyes. The mean retinal thickness from the inner surface to the tip of the photoreceptors was almost the same in the eye that received 5 μg melphalan and the fellow eye (Fig. 4).
The histologic samples of the rabbit retinas from the posterior fundus 4 weeks after vitrectomy with 5-, 10-, and 20-μg/ml concentrations of melphalan. Top: all retinal layers have a normal configuration like the control fellow eye after perfusion of melphalan at a concentration of 5 μg/ml. Middle: with the 10-μg/ml concentration, necrosis of the inner nuclear layer, thinning of the outer nuclear layer due to decreased nuclei, and occasional loss of photoreceptors are observed. Bottom: with the 20 μg/ml concentration, the retina is extremely thin. The outer nuclear layer and the photoreceptors have been replaced by scar tissue. One array of pyknotic nuclei remains in the inner nuclear layer. Few ganglion cells remain, but the inner plexiform layer is extremely attenuated. The retinal thickness from the inner surface to the tip of the photoreceptors is almost the same in the eye with 5-μg melphalan and the fellow eye. The retinal thickness is 10% attenuated in the eye with 10-μg melphalan compared with the fellow eye. The retinal thickness of the eye with 20-μg melphalan has become only 30% that of the fellow eye
10-μg/ml melphalan perfusion group
Compared with the pretreatment status, the ERG amplitude rates of the a- and b-waves in six rabbits decreased to about 68% and 65% on day 3 after vitrectomy, slightly declined until day 7, and became stable by day 28 (Figs. 2, 3). The data are shown in Table 1. The peak implicit times of the a- and b-waves were not prolonged significantly compared to the fellow eyes. Histologic sections from the treated eyes of two rabbits showed condensation of the nuclei in the inner nuclear layer and a reduced number of nuclei in the outer nuclear layer, which resulted in thinning of the outer nuclear layer. The photoreceptor inner and outer segments showed occasional defects, but the remaining photoreceptors appeared normal. The fellow eyes had a normal retinal structure. The mean retinal thickness was about 10% attenuated in the eye with 10 μg melphalan compared with the fellow eye (Fig. 4).
20-μg/ml melphalan perfusion group
The ERG amplitude rates of the a- and b-wave also showed a significant decrease compared with the fellow eyes. The ERG amplitudes of all waves decreased significantly after intravitreal perfusion of melphalan. The amplitudes decreased to about 46% at day 3 after vitrectomy and progressively decreased, becoming almost flat on day 28. The peak implicit times of the a- and b-wave did not increase significantly during the 28 days. The detailed data are listed in Table 1.
Histological sections from treated eyes of two rabbits showed severe retinal attenuation. The outer nuclear layer, the outer plexiform layer, and the photoreceptors were replaced by scar tissue. One array of pyknotic cells remained in the inner nuclear layer. Few ganglion cells remained, but the inner plexiform layer was attenuated. The fellow eyes had a normal retinal structure. The retinal thickness of the eye with 20 μg melphalan became only about 30% that of the fellow eye (Fig. 4).
Slit-lamp examination and indirect ophthalmoscopy
Slit-lamp examination and indirect ophthalmoscopy during the experimental period showed no corneal opacity, cataract, intraocular hemorrhage, retinal detachment, or any other complications after vitrectomy with intraocular melphalan irrigation.
Discussion
Our study showed that there were no adverse effects on the ERG amplitude and peak implicit rates of the a- and b-waves during the 4 weeks after vitrectomy with a 5-μg/ml melphalan infusion in rabbit eyes. The histologic sections appeared normal in all retinal layers 4 weeks after the 5-μg/ml melphalan infusion. However, the eyes treated with the 10-μg/ml melphalan perfusion developed necrosis in the inner nuclear layer and attenuation of the outer nuclear layer. The amplitudes of the a- and b-waves decreased, while the implicit times were not prolonged.
Retinal necrosis was more severe in the eyes treated with the 20-μg/ml melphalan perfusion. The outer retinal layers, including the outer nuclear layer and the photoreceptors, were replaced by scar tissue. The ERG amplitudes of the a- and b-waves also decreased significantly compared with the preoperative values.
Melphalan, the anticancer agent of the alkylating agent series, blocks tumor cell growth by inhibiting nucleic acid biosynthesis and bone marrow suppression, and has an anticancer effect in a dose-dependent manner. Melphalan, which is commonly used to treat multiple myeloma, ovarian carcinoma, malignant melanoma, and malignant lymphoma, has been chosen for local chemotherapy of retinoblastoma because of evidence that the drug inhibits colony formation most strongly among 12 anticancer agents, using a clonogenic assay in double agar medium [16]. Inomata and Kaneko also reported that melphalan at a concentration of 4 μg/ml killed retinoblastoma cells in vitro. Those investigators found that retinoblastoma was most sensitive to melphalan combined with heating to 42 degrees C for 1 hour in vitro. Ueda et al., who studied the retinal toxicity of intravitreal melphalan on ERGs and histologic sections from albino rabbits to establish a nontoxic dose for clinical use, reported that the ERGs and histologic sections appeared normal after the 10-μg intravitreal injection. However, decreased ERG amplitudes and degeneration of the retinal structures were observed in the 20- and 90-μg injection groups [17, 18].
Conservative therapy for intraocular retinoblastoma includes external beam radiotherapy, chemotherapy, focal laser therapy [21], brachytherapy [22, 23], cryopexy [21], and photodynamic therapy. Several reports have indicated that 40% of patients have a recurrence of retinoblastoma after external beam radiotherapy, and 90% of them could have some side effects including cataract, radiation retinopathy, cosmetic deformity, and the risk of secondary neoplasm [24]. Consequently, chemotherapy combined with focal laser therapy and cryotherapy recently has become a mainstay of treatment [25, 26].
Although intravitreal melphalan injection after ophthalmic arterial injection combined with ocular hyperthermia has been performed at the National Cancer Center Hospital, the rate of ocular preservation remains about 50% in cases with vitreous seeding [14]. Using vitrectomy with intravitreal melphalan infusion, we can mechanically remove the vitreous seeding cells and maintain a precise dose of melphalan in the vitreous cavity. Because 4 μg/ml of melphalan kills retinoblastoma cells in vitro, vitrectomy with perfusion of 5 μg/ml of melphalan might be an option for treatment of retinoblastoma with vitreous seeding.
Further studies are needed to assess the long-term efficacy, complications, and safety of vitreous surgery, which might facilitate extraocular dispersion of tumor cells through the surgical wound.
References
Knudson AG Jr (1971) Mutation and cancer: statistical study of retinoblastoma. Proc Natl Acad Sci USA 68(4):820–823
Cassady JR, Sagerman RH, Tretter P, Ellsworth RM (1969) Radiation therapy in retinoblastoma. An analysis of 230 cases. Radiology 93(2):405–409
Sauerwein W, Hopping W, Bornfeld N (1997) Radiotherapy for retinoblastoma. Treatment strategies. Front Radiat Ther Oncol 30:93–96
Phillips C, Sexton M, Wheeler G, McKenzie J (2003) Retinoblastoma: review of 30 years’ experience with external beam radiotherapy. Australas Radiol 47(3):226–230
Scott IU, Murray TG, Feuer WJ, Van Quill K, Markoe AM, Ling S, Roth DB, O’Brien JM (1999) External beam radiotherapy in retinoblastoma: tumor control and comparison of 2 techniques. Arch Ophthalmol 117(6):766–770
Reese AB, Ellsworth RM (1964) Management of retinoblastoma. Ann N Y Acad Sci 114(2):958–962
Ellsworth RM (1969) The practical management of retinoblastoma. Trans Am Ophthalmol Soc 67:462–534
Gallie BL, Budning A, DeBoer G, Thiessen JJ, Koren G, Verjee Z, Ling, V, Chan HS (1996) Chemotherapy with focal therapy can cure intraocular retinoblastoma without radiotherapy. Arch Ophthalmol 114(11):1321–1328
Kingston JE, Hungerford JL, Madreperla SA, Plowman PN (1996) Results of combined chemotherapy and radiotherapy for advanced intraocular retinoblastoma. Arch Ophthalmol 114(11):1339–1343
Murphree AL, Villablanca JG, Deegan WF 3rd, Sato JK, Malogolowkin M, Fisher A, Parker R, Reed E, Gomer CJ (1996) Chemotherapy plus local treatment in the management of intraocular retinoblastoma. Arch Ophthalmol 114(11):1348–1356
Shields CL, De Pdotter P, Himelstein BP, Shields JA, Meadows AT, Maris JM (1996) Chemoreduction in the initial management of intraocular retinoblastoma. Arch Ophthalmol 114(11):1330–1338
Linn Murphree A (2005) Intraocular retinoblastoma: the case for a new group classification. Ophthalmol Clin North Am 18(1):41–53, viii
Yamane T, Kaneko A, Mohri M (2004) The technique of ophthalmic arterial infusion therapy for patients with intraocular retinoblastoma. Int J Clin Oncol 9(2):69–73
Kaneko A, Suzuki S (2003) Eye-preservation treatment of retinoblastoma with vitreous seeding. Jpn J Clin Oncol 33(12):601–607
Lagendijk JJ (1982) A microwave heating technique for the hyperthermic treatment of tumours in the eye, especially retinoblastoma. Phys Med Biol 27(11):1313–1324
Inomata M, Kaneko A (1987) Chemosensitivity profiles of primary and cultured human retinoblastoma cells in a human tumor clonogenic assay. Jpn J Cancer Res 78(8):858–868
Ueda M, Tanabe J, Suzuki T, Sakai H, Mochizuki K, Kitano K, Inomata M, Kaneko A (1994) Conservative therapy for retinoblastoma-effect of melphalan on in vitro electroretinogram. Nippon Ganka Gakkai Zasshi 98(4):352–356
Ueda M, Tanabe J, Inomata M, Kaneko A, Kimura T (1995) Study on conservative treatment of retinoblastoma-effect of intravitreal injection of melphalan on the rabbit retina. Nippon Ganka Gakkai Zasshi 99(11):1230–1235
Okabe J, Kimura H, Kunou N, Okabe K, Kato A, Ogura Y (2003) Biodegradable intrascleral implant for sustained intraocular delivery of betamethasone phosphate. Invest Ophthalmol Vis Sci 44(2):740–744
Marmor MF, Holder GE, Seeliger MW, Yamamoto S (2004) Standard for clinical electroretinography (2004 update). Doc Ophthalmol 108(2):107–114
Shields JA, Shields CL (1990) Treatment of retinoblastoma with cryotherapy. Trans Pa Acad Ophthalmol Otolaryngol 42:977–980
Rosengren B, Tengroth B (1977) Retinoblastoma treated with a 60CO applicator. Acta Radiol Ther Phys Biol 16(2):110–116
Shields CL, Shields JA, Minelli S, De Potter P, Hernandez C, Cater J, Brady L (1993) Regression of retinoblastoma after plaque radiotherapy. Am J Ophthalmol 115(2):181–187
Eng C, Li FP, Abramson DH, Ellsworth RM, Wong FL, Goldman MB, Seddon J, Tarbell N, Boice JD Jr (1997) Mortality from second tumors among long-term survivors of retinoblastoma. J Natl Cancer Inst 85(14):1121–1128
Shields CL, Shields JA, Needle M, de Potter P, Kheterpal S, Hamada A, Meadows AT (1997) Combined chemoreduction and adjuvant treatment for intraocular retinoblastoma. Ophthalmology 104(12):2101–2111
Friedman DL, Himelstein B, Shields CL, Shields JA, Needle M, Miller D, Bunin GR, Meadows AT (2000) Chemoreduction and local ophthalmic therapy for intraocular retinoblastoma. J Clin Oncol 18(1):12–17
Author information
Authors and Affiliations
Corresponding author
Additional information
Grant Support: Supported in part by a grant from the Health and Welfare Ministry, Japan.
Rights and permissions
About this article
Cite this article
Shimoda, Y., Hamano, R., Ishihara, K. et al. Effects of intraocular irrigation with melphalan on rabbit retinas during vitrectomy. Graefes Arch Clin Exp Ophthalmol 246, 501–508 (2008). https://doi.org/10.1007/s00417-007-0685-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-007-0685-3