Abstract
Background
Vascular endothelial growth factor (VEGF) plays an important role in many diseases of the posterior pole that are characterized by macular edema and/or intraocular neovascularization. Recently anti-VEGF agents such as ranibizumab and pegaptanib sodium have been shown to be beneficial in the treatment of choroidal neovascularization (CNV) secondary to age-related macular degeneration (ARMD). However in most parts of the world, both pegaptanib sodium and ranibizumab are not readily available. Bevacizumab, a humanized recombinant monoclonal IgG antibody that binds and inhibits all VEGF isoforms, has been proposed as an alternative treatment option.
Methods
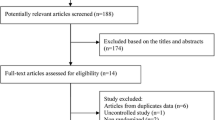
A total of 1,265 consecutive patients were injected with bevacizumab for diseases such as proliferative diabetic retinopathy, diabetic macular edema, retinal vein occlusions, and CNV of several etiologies including ARMD at eight Latin American institutions from 1 September 2005 to 31 January 2006. Of these 1,265, 92 were excluded because they were injected once and lost to follow-up. The remaining 1,173 patients constitute the subjects of this retrospective, multicenter, open label, uncontrolled interventional case series that reports the cumulative systemic and ocular adverse events following intravitreal bevacizumab during 12 months of follow-up. Patients were examined at baseline and then monthly. If the patients were unable to attend the 12-month visit, a telephone interview was conducted to assess for possible systemic complications.
Results
A total of 4,303 intravitreal injections of bevacizumab on 1,310 eyes was reported. All 1,173 patients were accounted for at the 12-month visit. Systemic adverse events were reported in 18 (1.5%) patients. These included seven (0.59%) cases of an acute elevation of systemic blood pressure, six (0.5%) cerebrovascular accidents, five (0.4%) myocardial infarctions, two (0.17%) iliac artery aneurysms, two (0.17%) toe amputations and five (0.4%) deaths. Ocular complications included seven (0.16%) bacterial endophthalmitis, seven (0.16%) tractional retinal detachments, four (0.09%) uveitis, and a case (0.02%) each of rhegmatogenous retinal detachment and vitreous hemorrhage.
Conclusion
Despite the limited follow-up, repeated intravitreal injections of either 1.25 mg or 2.5 mg of bevacizumab appears to be safe and well tolerated during the 1st year.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vascular endothelial growth factor (VEGF) plays an important role in many diseases of the posterior pole that are characterized by macular edema and/or intraocular neovascularization [1, 2]. Such diseases include proliferative diabetic retinopathy (PDR), diabetic macular edema (DME), neovascular glaucoma, retinopathy of prematurity, choroidal neovascularization (CNV) and retinal vein occlusions [1, 2]. VEGF inhibition in experimental models of diabetic retinopathy and CNV have shown promising results [3, 4]. Recently pegaptanib sodium (Macugen®, Eyetech, NY, NY), an aptamer against VEGF165, has been shown to be beneficial in the treatment of CNV secondary to age-related macular degeneration (ARMD) and DME [5, 6]. Ranibizumab (Lucentis®, Genentech, San Francisco, CA), a fragment of a humanized monoclonal antibody against all VEGF isoforms, also appears to be beneficial in the treatment of CNV secondary to ARMD [7]. However, in most parts of the world, both pegaptanib sodium and ranibizumab are not readily available. A humanized, recombinant monoclonal IgG antibody that binds and inhibits all VEGF isoforms, bevacizumab (Avastin®, Genentech, San Francisco, CA), is readily available. It has been approved by the United States Food and Drug Administration as an adjuvant agent in the treatment of metastatic colorectal carcinoma. In these patients with metastatic colorectal carcinoma, there was an increased rate of thromboembolic disease in patients receiving an intravenous infusion of bevacizumab 5 mg/kg of body weight every 2 weeks. In addition systemic hypertension was seen in a fair number of patients [8]. Michels and colleagues reported on the benefits of systemic bevacizumab administration in eyes with CNV secondary to ARMD. The most common side effect reported by them was systemic hypertension [9]. Rosenfeld et al. proposed the administration of intravitreal bevacizumab as an alternative to minimize the systemic risks associated with systemic anti-VEGF therapy [10, 11].
The purpose of this study is to report on the systemic and ocular safety of intravitreal injections of 1.25 mg or 2.5 mg of bevacizumab.
Materials and methods
This is an open label, uncontrolled multicenter interventional case series of all patients that were injected from 1 September 2005 to 31 January 2006 with either 1.25 mg or 2.5 mg of intravitreal bevacizumab for a variety of retinal disorders characterized by intraocular neovascularization and/or macular edema including proliferative diabetic retinopathy, diabetic macular edema, retinal vein occlusions, and CNV of several etiologies including ARMD. A total of 1,265 consecutive patients were identified at eight institutions in seven countries of Latin America. Of these 1,265 patients, 92 were excluded because they were injected once and lost to follow-up. The remaining 1,173 patients constitute the subjects of this report. The study and data accumulation were carried out in adherence to the tenets of the Declaration of Helsinki. Prior to injection, all patients were given an informed consent and offered alternative treatments. All patients were made aware of the off-label use of this medication, possible systemic and ocular complications.
Patients underwent a complete ocular examination at baseline and then monthly. Additional examinations were scheduled according to the clinical decision of each individual investigator. In addition patients underwent fluorescein angiography and optical coherent tomography at different time intervals at baseline and several time points during their follow-up. Monitored systemic conditions included myocardial infarction, stroke, systemic hypertension, thromboembolic diseases and death. Blood pressure was measured prior to bevacizumab injection and at 2 weeks following each injection. Other systemic conditions were assessed by a throrough review of systems. All patients were contacted in December 2006 and January 2007 and asked to return for a check-up. If the patients were unable to attend, a telephone interview was conducted to assess for possible systemic complications.
Bevacizumab was stored under refrigeration in two different ways: (1) a single vial of 100 mg/4 ml was re-utilized as needed and (2) the contents of the vial were aliquoted out into single-use syringes under sterile conditions. All injections were performed in the usual sterile fashion with a sterile lid speculum and 5% topical povidone-iodine [12]. Topical antibiotics were prescribed for 5 to 7 days after the injection.
Results
A total of 4,303 intravitreal injections of bevacizumab in 1,310 eyes of 1,173 patients were reported from eight centers in seven countries. The baseline demographic characteristics are summarized in Table 1. The most common indications for intravitreal bevacizumab were diabetic retinopathy and CNV of several etiologies. These are listed in Table 2. The patients have been followed for an average of 13.2 months (range 12–15 months). At the 1 month visit, 1,160 patients presented, 997 patients showed up for the 6-month vist, and 786 patients returned for the 12-month visit. For the patients missing their 12-month appointment, 387 telephone contacts were made. Thus, at the 12-month follow-up visit, all patients had been accounted for. Reinjections were reported in 786 eyes after an average of 8 weeks (range 4–14 weeks). On average each eye received 3.3 injections (range 1–10 injections). Of the 4,303 injections, 687 (16%) were given with the 1.25 mg dose and 3,616 (84%) with the 2.5 mg dose. Of all the injections, 1,833 (42%) were performed with single-use sterile syringes, and 2,470 (58%) were drawn from the same vial as needed.
Of the 1,173 patients, 18 (1.5%) suffered systemic adverse events. These included five deaths (0.4%). The most common adverse event was a transient elevation in systemic blood pressure, which was seen in seven (0.6%) patients. These elevations in blood pressure were generally mild and ocurred anywhere from 7 h to 2 weeks following injection. The only exception was an 86-year-old woman with known systemic hypertension who developed a choroidal neovascular membrane in her right eye and was injected with 1.25 mg of bevacizumab. Seven hours later she did not feel well and was seen in the Emergency Room. Her blood pressure was measured to be 240/100. Four patients developed cerebrovascular accidents resulting in two deaths. Three patients developed myocardial infarctions with two fatalities. Two additional patients suffered a myocardial infarction and a cerebrovascular accident. One managed to survive. So in total there were six (0.5%) cerebrovacular accidents and five (0.4%) myocardial infarctions. Two (0.17%) patients developed iliac artery aneurysms 13 and 14 months after bevacizumab injection. Two (0.17%) diabetic patients underwent toe amputations at 2 and 6 weeks following injection. All the systemic adverse events are summarized in Table 3.
Table 4 lists the reported ocular complications. The most common ocular complication was subconjunctival hemorrhage, which was seen in 838 cases. Seven (0.16%) cases of a transient increase of intraocular pressure were reported. These were managed with topical medications. Four (0.09%) cases of severe uveitis were reported. These were managed with topical corticosteroids. Seven (0.16%) cases of bacterial endophthalmitis were observed. The cultures yielded five cases of coagulase negative staphylococci and one case each of Staphylococcus aureus and Streptococcus pneumoniae. Six of the seven endophthalmitis cases were injected with bevacizumab stored in sterile single-use syringes. The five eyes with coagulase-negative staphylococci were managed with pars plana vitrectomy and intravitreal antibiotics. The other two cases were managed solely with intravitreal antibiotics. Six of the seven eyes lost vision despite treatment. One eye remained at the pre-injection visual acuity of 20/100, and the rest lost vision to counting fingers, hands motions and light perception. Seven (0.16%) eyes with PDR characterized by extensive intraocular neovascularization despite extensive panretinal photocoagulation were injected with 1.25 mg of bevacizumab; only one eye had been injected with the 2.5 mg dose. At a mean of 1 week (range: 4 to 13 days), it was noticed that the neovascular membranes had regressed, but the resulting fibrous tissue led to the development or progression of tractional retinal detachment. Six of the seven eyes underwent pars plana vitrectomy with satisfactory anatomic results.
Discussion
Anti-VEGF agents gain access to the systemic circulation following an intravitreal injection [11, 13–15]. Systemic VEGF blockade can give rise to complications such as systemic hypertension, thromboembolic diseases or even death [8, 16]. In a cancer trial, hypertension was noted in 22.4% of patients treated with chemotherapy and bevacizumab compared to 8.3% in the chemotherapy-only group [8]. A mild transient, but significant elevation in mean systolic blood pressure was reported in patients with CNV secondary to ARMD who received a systemic infusion of bevacizumab [9]. In our study, a transient mild rise in systemic blood pressure was seen in seven (0.6%) patients a few hours to 2 weeks after an intravitreal injection of bevacizumab. In contrast in a smaller series of 45 patients, Kernt et al. reported significantly lower diastolic blood pressures at 1 and 6 h following an intravitreal injection of 1.25 mg of bevacizumab compared to baseline. They attributed these changes to normal physiological diurnal variations or alternatively to easing of surgery-related stress [17].
As many as 5% of all patients using systemic bevacizumab in combination with chemotherapy may be at an increased risk of developing a serious or fatal thromboembolic event [8, 18]. Fung and associates designed an internet-based voluntary survey to assess the adverse events associated with intravitreal bevacizumab. In this survey, 7,113 injections were reported on 5,228 patients. They reported 2 deaths, 5 cerebrovascular accidents and 15 blood pressure elevations in this cohort of patients [19]. Other smaller series have also confimed a lack of systemic complications following an intravitreal injection of 1.25 mg of bevacizumab [20, 21]. In our series of 1,173 patients, 18 (1.5%) developed systemic adverse events, including 5 (0.4%) deaths.
Several clinical trials examining different pharmacologic agents against exudative age-related macular degeneration have reported a mortality rate of 2% to 4% in both experimental and control groups [6, 22–24]. In addition, the rates of thromboembolic disease have ranged from 1.3% to 6%. There were no statistically significant differences between anti-VEGF treated eyes and controls [6, 25]. Spaide and colleagues conducted a retrospective study of 266 patients that underwent an intravitreal injection of 1.25 mg of bevacizumab for exudative ARMD. They reported transient ischemic attacks in two patients, a non-fatal myocardial infarction and two deaths. The mortality rate of 0.6% in our sub-group of 345 patients with ARMD is much lower than other series.
The estimated mortality rate of non-insulin-dependent diabetic patients has been reported to be 5.4% [26]. In contrast in our series, 0.55% (3/548) of diabetic patients passed away.
The different mortality rates between our series and the rest of the literature may be explained by our small sample size, short-term follow-up of our patients and the biases inherent in a retrospective review. Alternatively, the different ethnic background of our population from that of the aforementioned clinical trials could explain different rates of mortality in different populations. In any event, there did not seem to be an increased number of deaths.
Another concern has to do with the fact that bevacizumab is not manufactured or labeled for intravitreal injection. Several electrophysiologic and histologic studies have shown the lack of ocular toxicity of intravitreal bevacizumab in cell cultures, animal and human eyes at least in the short term [27–31].
Bacterial endophthalmitis is an expected and dreaded complication of any intravitreal injection. Sterile technique and antisepsis with instillation of topical povidone iodine 5% into the conjunctival fornix prior to an intravitreal injection may reduce the risk of endophthalmitis [12]. The rate of bacterial endophthalmitis for intravitreal injections of a variety of substances such as pegaptanib sodium, ranibizumab, gancyclovir, fomivirsen, cidofovir, triamcinolone and gas is 0.1% to 0.6% [6, 7, 32]. Our rate of bacterial endophthalmitis of 0.16% per injection is similar to those reported in the literature [32]. One might think that the re-utilization of a single vial might be a risk factor in the development of infectious endophthalmitis. However, in 86% (6/7) of our cases of bacterial endophthalmitis the injected bevacizumab had been stored in single-use sterile syringes. Interestingly in our study, the rate of bacterial endophthalmitis was 0.04% in subjects who were injected from a single multi-use vial. In contrast, the rate of bacterial endophthalmitis was 0.33% (6/1,833 injections) in eyes injected with single-use sterile syringes.
Intraocular inflammation has been shown to be the dose-limiting toxicity of intravitreal ranibizumab [11]. In fact, the manufacturer switched from a lyophilized formulation to a liquid formulation. Given that bevacizumab and ranibizumab are derived from the same molecule, it is somewhat surprising that in our study only four cases of severe anterior uveitis were reported. These were easily managed with topical corticosteroids. However, this is consistent with the findings of Ziemssen and colleagues that showed that the aqueous flare in 60 patients injected with 1.25 mg of intravitreal bevacizumab for age-related macular degeneration had a slight increase only in the first post-injection day as measured by the flaremeter [33].
Seven eyes with progressive proliferative diabetic retinopathy despite aggressive panretinal photocoagulation underwent adjuvant bevacizumab injections. In a matter of days, the neovascularization regressed, but the resulting fibrous scar tissue led to the development or progression of tractional retinal detachments. Six of the seven eyes underwent pars plana vitrectomy with satisfactory anatomic results. Therefore, caution should be exercised when injecting these eyes, and the patients should be warned that vitrectomy might be warranted after all.
In summary, an intravitreal injection of either 1.25 mg or 2.5 mg of bevacizumab appears to be safe and well tolerated during the 1st year. Limitations of our study include its short term, its lack of randomization, its lack of controls and its retrospective design, which preclude any estimation of the long-term safety of intravitreal bevacizumab. Furthermore, the detection of systemic adverse events such as myocardial infarction was based solely on a thorough review of systems. Patients did not undergo routine cardiac examination. Therefore, our rate of adverse events probably underestimates the true rate of events as clinically silent events went undetected. Continued monitoring of the adverse side effects in these patients is essential to determine if chronic inhibition of VEGF by bevacizumab remains safe.
References
Adamis AP, Aiello LP, D’Amato RA (1999) Angiogenesis and ophthalmic disease. Angiogenesis 3:9–14
Adamis AP, Shima DT (2005) The role of vascular endothelial growth factor in ocular health and disease. Retina 25:111–118
Qaum T, Xu Q, Joussen AM, et al (2001) VEGF-initiated blood-retinal barrier breakdown in early diabetes. Invest Ophthalmol Vis Sci 42:2408–2413
Saishin Y, Saishin Y, Takahashi K, et al (2003) VEGF-TRAP(R1R2) suppresses choroidal neovascularization and VEGF-induced breakdown of the blood-retinal barrier. J Cell Physiol 195:241–248
Cunningham ET Jr, Adamis AP, Altaweel M, et al (2005) A phase II randomized double-masked trial of pegaptanib, an anti-vascular endothelial growth factor aptamer, for diabetic macular edema. Ophthalmology 112:1747–1757
Gragoudas ES, Adamis AP, Cunningham ET Jr, et al (2004) Pegaptanib for neovascular age-related macular degeneration. N Engl J Med 351:2805–2816
Heier JS, Antoszyk AN, Pavan PR, et al (2006) Ranibizumab for treatment of neovascular age-related macular degeneration: a phase I/II multicenter, controlled, multidose study. Ophthalmology 113(642):e1–e4
Hurwitz H, Fehrenbacher L, Novotny W, et al (2004) Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 350:2335–2342
Michels S, Rosenfeld PJ, Puliafito CA, et al (2005) Systemic bevacizumab (Avastin) therapy for neovascular age-related macular degeneration twelve-week results of an uncontrolled open-label clinical study. Ophthalmology 112:1035–1047
Rosenfeld PJ, Fung AE, Puliafito CA (2005) Optical coherence tomography findings after an intravitreal injection of bevacizumab (avastin) for macular edema from central retinal vein occlusion. Ophthalmic Surg Lasers Imaging 36:336–339
Rosenfeld PJ, Moshfeghi AA, Puliafito CA (2005) Optical coherence tomography findings after an intravitreal injection of bevacizumab (Avastin) for neovascular age-related macular degeneration. Ophthalmic Surg Lasers Imaging 36:331–335
Aiello LP, Brucker AJ, Chang S, et al (2004) Evolving guidelines for intravitreous injections. Retina 24:S3–19
Drolet DW, Nelson J, Tucker CE, et al (2000) Pharmacokinetics and safety of an anti-vascular endothelial growth factor aptamer (NX1838) following injection into the vitreous humor of rhesus monkeys. Pharm Res 17:1503–1510
Gaudreault J, Fei D, Rusit J, et al (2005) Preclinical pharmacokinetics of Ranibizumab (rhuFabV2) after a single intravitreal administration. Invest Ophthalmol Vis Sci 46:726–733
van Wijngaarden P, Coster DJ, Williams KA (2005) Inhibitors of ocular neovascularization: promises and potential problems. JAMA 293:1509–1513
Sane DC, Anton L, Brosnihan KB (2004) Angiogenic growth factors and hypertension. Angiogenesis 7:193–201
Kernt M, Neubauer AS, Kampik A (2007) Intravitreal bevacizumab (Avastin) treatment is safe in terms of intraocular and blood pressure. Acta Ophthalmol Scand 85:119–120
Ratner M (2004) Genentech discloses safety concerns over Avastin. Nat Biotechnol 22:1198
Fung AE, Rosenfeld PJ, Reichel E (2006) The international intravitreal bevacizumab safety survey: using the internet to assess drug safety worldwide. Br J Ophthalmol 90:1344–1349
Spaide RF, Laud K, Fine HF, et al (2006) Intravitreal bevacizumab treatment of choroidal neovascularization secondary to age-related macular degeneration. Retina 26:383–390
Avery RL, Pieramici DJ, Rabena MD, et al (2006) Intravitreal bevacizumab (Avastin) for neovascular age-related macular degeneration. Ophthalmology 113(3):363–372 e5
(2001) Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: two-year results of 2 randomized clinical trials-tap report 2. Arch Ophthalmol 119:198–207
(2001)Verteporfin therapy of subfoveal choroidal neovascularization in age-related macular degeneration: two-year results of a randomized clinical trial including lesions with occult with no classic choroidal neovascularization-verteporfin in photodynamic therapy report 2. Am J Ophthalmol 131:541–560
Slakter JS, Bochow TW, D’Amico DJ, et al (2006)Anecortave acetate (15 milligrams) versus photodynamic therapy for treatment of subfoveal neovascularization in age-related macular degeneration. Ophthalmology 11:3–13
Rosenfeld PJ, Rich RM, Lalwani GA (2006) Ranibizumab: phase III clinical trial results. Ophthalmol Clin North Am 19:361–372
Geiss LS, Herman WH, PJS (2007) Mortality in Non-Insulin Dependent Diabetes. Diabetes in America, 2nd Ed. http://diabetes.niddk.nih.gov/dm/pubs/america/pdf/chapter11.pdf. Accessed February 14
Manzano RP, Peyman GA, Khan P, Kivilcim M (2006) Testing intravitreal toxicity of bevacizumab (Avastin). Retina 26:257–261
Shahar J, Avery RL, Heilweil G, et al (2006) Electrophysiologic and retinal penetration studies following intravitreal injection of bevacizumab (Avastin). Retina 26:262–269
Maturi RK, Bleau LA, Wilson DL (2006) Electrophysiologic findings after intravitreal bevacizumab (Avastin) treatment. Retina 26:270–274
Luthra S, Narayanan R, Marques LE, et al (2006) Evaluation of in vitro effects of bevacizumab (avastin) on retinal pigment epithelial, neurosensory retinal, and microvascular endothelial cells. Retina 26:512–518
Luke M, Warga M, Ziemssen F, et al (2006) Effects of bevacizumab on retinal function in isolated vertebrate retina. Br J Ophthalmol 90:1178–1182
Jager RD, Aiello LP, Patel SC, Cunningham ET Jr (2004) Risks of intravitreous injection: a comprehensive review. Retina 24:676–698
Ziemssen F, Warga M, Neuhann IM, et al (2006) Does intravitreal injection of bevacizumab have an effect on the blood-aqueus barrier function? Br J Ophthalmol 90:922
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
For a complete listing of participating members of PACORES see the Appendix.
The authors have no financial interests in the subject matter presented.
Appendix
Appendix
The following investigators belong to the Pan-American Collaborative Retina Study Group (PACORES):
The Pan-American Collaborative Retina Study Group (PACORES)*
L. Wu (PI), T. Evans, Instituto de Cirugia Ocular, San Jose, Costa Rica; J.F. Arevalo (PI), J.G. Sanchez, R.A. Garcia-Amaris, Clinica Oftalmologica Centro Caracas and the Arevalo-Coutinho Foundation for Research in Ophthalmology, Caracas, Venezuela; M. Farah (PI), M. Maia, F.B. Aggio, Universidade Federal de São Paulo-Departamento de Oftalmologia-Instituto da Visão-Sao Paulo, Brazil; H. Quiroz-Mercado (PI), J. Fromow-Guerra, V. Morales-Canton, J. Dalma-Weiszhausz, Asociación para Evitar la Ceguera en México, Mexico City, Mexico; F.J. Rodriguez (PI), R. Infante, S. Flores, D. Medina, Fundacion Oftalmologica Nacional, Universidad del Rosario, Bogota, Colombia; M.H. Berrocal (PI), V. Cruz-Villegas, University of Puerto Rico, San Juan, Puerto Rico; F. Graue-Wiechers (PI), D. Lozano-Rechy, V. Robledo, Fundacion Conde Valenciana, Mexico City, Mexico; J.A. Roca (PI), G. Reategui, Clínica Ricardo Palma, Lima, Peru; M. J. Saravia (PI), M. Martinez-Cartier, Hospital Universitario Austral, Buenos Aires, Argentina; M. Avila (PI), Universidade Federal de Goiás-Departamento de Oftalmologia-Goiânia, Brazil; RA Costa (PI), J. Cardillo, Hospital de Olhos de Araraquara, and the Universidade de Sao Paulo, Sao Paulo, Brazil.
*PI = principal investigator.
Rights and permissions
About this article
Cite this article
Wu, L., Martínez-Castellanos, M.A., Quiroz-Mercado, H. et al. Twelve-month safety of intravitreal injections of bevacizumab (Avastin®): results of the Pan-American Collaborative Retina Study Group (PACORES). Graefes Arch Clin Exp Ophthalmol 246, 81–87 (2008). https://doi.org/10.1007/s00417-007-0660-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-007-0660-z