Abstract
Background
To compare the results of ultrasonic and Orbscan pachymetry in corneal haze not related to surgery.
Methods
An institutionally based, prospective, controlled clinical trial included 40 eyes of 40 consecutive patients with corneal haze not related to surgery. Fifty normal eyes were used as a control group to calculate the customized acoustic factor. Corneal haze was graded with slit-lamp by a single examiner. Ultrasonic and Orbscan II pachymetry measurements were obtained. Paired t- and Kruskal-Wallis tests were used to evaluate the difference between ultrasonic and Orbscan pachymetry measurements. Correlation of the two methods and haze grade were determined with Kendall’s tau-b correlation analysis.
Results
Eighty-five percent of patients had moderate haze. With the customized acoustic factor, Orbscan values were significantly smaller than ultrasonic pachymetry measurements (p = 0.001, paired samplet-test). Increased haze grade resulted in smaller Orbscan pachymetry measurements however, this difference was insignificant (p = 0.444, Kruskal-Wallis test). A positive correlation was found between two methods, though insignificant (p = 0.064, Kendall’s tau-b correlation). When grouped in respect of diagnoses, differences in pachymetry measurements as well as the correlation were not significant (p > 0.05).
Conclusion
An insignificant positive correlation was found between the two methods in the presence of corneal haze. Orbscan measurements were inversely related to haze grading, and were significantly lower than ultrasonic pachymetry. According to our results, we recommend that clinicians should not count on Orbscan topography alone in the presence of corneal haze.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An accurate measurement of corneal thickness is essential in keratorefractive procedures, intraocular pressure measurements, diagnosis of corneal diseases, and correlation with physiologic status of corneal endothelium. Corneal topography and pachymetry are the two most commonly used tools for this purpose.
Ultrasonic pachymetry and Orbscan II topography system were used and compared extensively in normal corneas, and a correlation was shown between the two methods [7, 14]. Orbscan was reported as the most repeatable technique; however, the results were approximately 23–30 μm higher than ultrasound [3, 9, 10, 12, 15]. So a default setting (0.92) was developed as the acoustic factor (AF), and recommended by the manufacturer to overcome this problem. With the use of AF, Orbscan values were reported to underestimate the corneal thickness with a lower difference, of the order of 10–15 μm [7, 11].
In corneal haze, the light bundles that travel through the cornea may change direction and result in variations in posterior surface appearance. Since it is an optically based analysis, Orbscan measurements might be affected by the loss of transparency in the cornea. Thus, in the present study we aimed to evaluate the ultrasonic and Orbscan pachymetry results of patients with corneal haze not related to surgery.
Materials and methods
Between July 2005 and June 2006, consecutive patients with corneal haze of different grades were prospectively included in this controlled clinical trial. The study was conducted in accordance with the ethical guidelines set forth in the 1975 Declaration of Helsinki. Institutional Review Board Approval was obtained. All patients were informed about the study, and gave written informed consent before participating to the study.
Patients with significant corneal haze on slit-lamp were included in the study group. Exclusion criteria from participation in the study were previous ocular surgery, history of contact lens use, glaucoma, and topical ocular medication use, excluding artificial tears. Only one eye of each patient was included. If one eye fulfilled the inclusion criteria it was included in the study. If both eyes had corneal opacity, measurements were obtained from both eyes and one eye was selected randomly by the toss of a coin. Forty eyes of 40 patients were included in the study group.
In a similar method, 50 eyes of 50 age-matched patients with normal eye and clear cornea were included in the control group. History of trauma, previous eye surgery, keratoconus, and any other ocular disease, and best spectacle-corrected visual acuity worse than 20/25 were defined as exclusion criteria for this group. Accepted refractive errors were hypermetropia ≤2 D, myopia ≤3 D, astigmatism ≤1 D.
Corneal haze was graded with slit-lamp (Topcon SL-7F, Topcon Co., Japan) by a single examiner (RAY) according to the grading scale of Fantes [6]. Each patient underwent pachymetry measurements that were taken between 11 a.m. and 2 p.m., at least 3 hours after awakening. To avoid any possible artifact caused by the contact of the ultrasonic pachymetry probe, pachymetry measurements were performed first with Orbscan Topography System (Orbscan II, Bausch & Lomb, France) followed by ultrasonic pachymetry (UP-1000 Ultrasonic pachymeter, Nidek Co, Japan). Each pachymetry was performed by one technician, who was masked to the results of the other. Orbscan measurements were performed once, and the value corresponding to the area with haze was accepted as the pachymetry measurement fo that eye. On the other hand, the technician who obtained the ultrasonic pachymetry measurements was instructed to take the measurements from the area with haze. Five consecutive ultrasonic pachymetry measurements were taken, and the mean of these was recorded as the ultrasonic pachymetry value.
In the control group, the Orbscan and ultrasonic measurements were performed. The custom AF was calculated in this group, and the same custom AF was applied to the study group.
The results of both measurements were recorded to SPSS software (Statistical Package for the Social Sciences, version 10.0, SPSS Inc, Chicago, IL, USA). The difference between ultrasonic and Orbscan pachymetry measurements was calculated using paired t-test. The difference within groups according to the haze grading and diagnoses was compared with Kruskal-Wallis test. Kendall’s tau-b correlation analysis was performed to evaluate the correlation of the two methods and haze grade. Any difference with significance of less than 0.05 was accepted as statistically significant.
Results
The control group had a mean age of 55.6 ± 11.7 years (ranging between 18 and 71 years). The mean ultrasonic pachymetry was 551.64 ± 29.89 μm. With Orbscan topography system without AF correction the mean pachymetry value was 572.63 ± 27.96 μm. The customized AF was determined as 0.964.
In the study group there were 22 females and 18 males, with a mean age of 56.4 ± 17.9 years (ranging from 16 to 78 years). The patients were grouped according to the grade of haze (Table 1). Eighty-five percent of the patients had moderate haze.
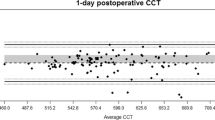
The mean pachymetry values of distributed haze grades are shown on Table 2. With the use of customized AF, the Orbscan pachymetry values were significantly smaller than the ultrasonic pachymetry measurements (p = 0.001, paired sample t-test). The histogram and scatter diagram representation of corneal pachymetry in relation to haze grading with ultrasonic and Orbscan measurements are shown in Figs. 1, 2 and 3. With the increase in haze grading, the results of Orbscan pachymetry measurements were smaller; however, this was insignificant (p = 0.444, Kruskal-Wallis test). The difference in ultrasonic pachymetry measurements was not significantly different concerning the haze grade (p = 0.483). A positive correlation was found between the ultrasonic and Orbscan pachymetry measurements (τ b = 0.205); however, this was not statistically significant (p = 0.064). The pachymetry values were not significantly correlated when evaluated for haze grade (p > 0.05).
The mean pachymetry measurements according to the etiological diagnosis of corneal opacities are shown in Table 3. The pachymetry measurements were not significantly different between ultrasonography and Orbscan measurements (p > 0.05). The Orbscan pachymetry measurements were not significantly different when compared in relation to the diagnoses (p = 0.067). However, the ultrasonic pachymetry showed a significant difference (p = 0.022), which was the result of the higher numbers in Fuchs’ endothelial dystrophy (mean 690 μm). When we excluded these eyes, the difference was insignificant in both ultrasonic and Orbscan pachymetry measurements (p = 0.057 and 0.051 respectively). The correlation of both methods was insignificant in respect of the diagnosis (p > 0.05). Kendall’s tau-b correlation could not be computed for Fuchs’ endothelial dystrophy because only two eyes had this diagnosis.
Discussion
The Orbscan topography system requires clear reflections on the epithelial and endothelial corneal surfaces and homogenous composition of the diverse optical media to obtain correct measurements [1]. A decreased accuracy in corneal thickness measurements has been reported in the presence of haze [1]. Some authors have suggested that use of Orbscan should be limited to corneas devoid of light scattering sources such as opacities, scarring, deposits, or edema [13]. However, corneal topography as well as pachymetry maps are required in some cases with haze during follow-up or planning treatment. Thus, we designed this study to evaluate the corneal thickness in the presence of mild to severe haze not related to surgery, to determine if both methods are accurate or, if not, which method is accurate in these eyes.
Cheng et al. recommended using a customized AF in Orbscan pachymetry [4]. For the calculation of the custom AF we designed an age-matched control group with clear corneas and refractive error in low ranges. The customized AF was determined as 0.964. With this customized AF, in corneas with haze the Orbscan pachymetry showed significantly lower readings than those for ultrasonic pachymetry. There was an insignificant positive correlation between the two measurements. The increase of haze grading showed no change in ultrasonic pachymetry measurements. On the other hand, smaller Orbscan pachymetry measurements were obtained with the increase in the haze grade. However, this difference was insignificant.
Optical quality of the cornea has been reported to be altered following excimer laser, and Orbscan has been found to underestimate the corneal thickness [11]. This underestimation was particularly significant in the early postoperative period, and gradually decreased with time [4]. The difference has been suggested to be due to the subepithelial haze, stromal interface, modifications in anterior corneal contour and increased reflectivity in the interface that was shown in confocal studies [4, 11]. Prisant et al. suggested that stromal haze was probably the most important factor in underestimation, which resulted probably from deviation of light rays while passing through the cornea, and thus resulting in a displacement of the posterior profile of the slit [11]. Accordingly, Iskander et al. reported that Orbscan measurements did return to normal with the disappearance of the haze in the cornea [8]. In the present study, although the correlation was not statistically significant the increase in haze grade resulted in lower measurements with Orbscan. We agree with earlier authors [4, 8, 11] that corneal haze results in underestimation of corneal thickness possibly related to the reduced transparency and disturbed light scatter. Supporting this theory, Cairns et al. investigated the accuracy of Orbscan II with different materials, and found that the results were more accurate in a material that scattered light in all directions [2]. On the other hand, in a semitransparent material the light was not evenly scattered but transmitted to a certain extent. Thus, the authors claim that the edges of the slit are less defined due to the reduced scatter. Boscia et al. proposed that in eyes with haze, the newly formed type-III collagen- and proteoglycan debris- filled vacuoles resulted in a high level of light scatter, with an ensuing increase in the refraction index of the cornea. In corneas with haze, the maximum level of light intensity lies at the interface between nontransparent and transparent corneal tissue, and the instrument might assume this interface to be the backspace of the cornea [1].
In patients with corneal haze following refractive surgery, Fakhry et al. found a significant correlation between the grade of haze and the decrease in Orbscan pachymetry readings [5]. Similar to that in patients with corneal haze who did not have previous eye surgery, the Orbscan results were lower than ultrasonic measurements. We believe that this study is unique, in that it includes patients who have significant corneal haze not related to surgery. One limitation is the diverse group of diagnosis. However, we believe that careful grading by a single observer was adequate to group the patients properly. Also, taking the measurements by two technicians who were masked to the other measurement strengthens the results. To our knowledge, there is no published paper comparing the corneal thickness measurements according to the clinical diagnoses. So we were unable to compare our results with literature. However, the Orbscan measurements showed lower readings than ultrasonic ones if they were grouped according to the diagnosis. These patients with corneal haze usually visit the clinician’s office frequently, sometimes at long intervals. As clinicians, we need to follow these eyes with monitoring the intraocular pressure and corneal thickness measurements, in addition to corrected visual acuity. Even though some of these eyes do not need surgery of the cornea, some may need cataract removal or filtrating procedures. Thus, we believe that careful monitoring of corneal thickness measurements is important in these eyes.
In conclusion, in patients with corneal haze, a positive though insignificant correlation was found between Orbscan and ultrasonic pachymetry methods. Orbscan measurements showed significant lower readings than those for ultrasonic pachymetry, and were inversely related to haze grade. According to our results, it seems that ultrasonic pachymetry measurements are superior to the Orbscan in corneas with a moderate degree of haze. We strongly recommend surgeons to use ultrasonic pachymetry and not to rely on the results of Orbscan topography in corneas with any degree of haze. Further investigation is required, particularly with larger numbers of patients with different diagnoses that result in corneal opacities. Furthermore, newly developed devices should be tested for their accuracy in these cases, since conclusions and planning might be assumed from these results.
References
Boscia F, La Tegola MG, Alessio G, Sborgia C (2002) Accuracy of Orbscan optical pachymetry in corneas with haze. J Cataract Refract Surg 28:253–258
Cairns G, McGhee CNJ, Collins MJ, Owens H, Gamble GD (2002) Accuracy of Orbscan II slit-scanning elevation topography. J Cataract Refract Surg 28:2181–2187
Chakrabarti HS, Craig JP, Brahma A, Malik TY, McGhee CNJ (2001) Comparison of corneal thickness measurements using ultrasound and Orbscan slit-scanning topography in normal and post-LASIK eyes. J Cataract Refract Surg 27:1823–1828
Cheng ACK, Rao SK, Tang E, Lam DSC (2006) Pachymetry assessment with Orbscan II in postoperative patients with myopic LASIK. J Refract Surg 22:363–366
Fakhry MA, Artola A, Belda JI, Ayala J, Alio JL (2002) Comparison of corneal pachymetry using ultrasound and Orbscan II. J Cataract Refract Surg 28:248–252
Fantes FE, Hanna KD, Waring GO III (1990) Wound healing after excimer laser keratomileusis (photorefractive keratectomy) in monkeys. Arch Ophthalmol 108:665–675
Gonzalez-Meijome JM, Cervino A, Yebra-Pimentel E, Parafita MA (2003) Central and peripheral corneal thickness measurements with Orbscan II and topographical ultrasound pachymetry. J Cataract Refract Surg 29:125–132
Iskander NG, Penno EA, Peters NT, Gimbel HV, Ferensowicz M (2001) Accuracy of Orbscan pachymetry measurements and DHG ultrasound pachymetry in primary laser in situ keratomileusis and LASIK enhancement procedures. J Cataract Refract Surg 27:681–685
Lackner B, Schmidinger G, Pieh S, Funovics MA, Skorpik C (2005) Repeatability and reproducibility of central corneal thickness measurement with Pentacam, Orbscan, and ultrasound. Optom Vis Sci 82:892–899
Marsich MM, Bullimore MA (2000) The repeatability of corneal thickness measures. Cornea 19:792–795
Prisant O, Calderon N, Chastang P, Gatinel D, Hoang-Xuan T (2003) Reliability of pachymetric measurements using Orbscan after excimer refractive surgery. Ophthalmology 110:511–515
Rainer G, Findl O, Peternel V, Kiss B, Drexler W, Skorpik C, Georgopoulos M, Schmetterer L (2004) Central corneal thickness measurements with partial coherence interferometry, ultrasound, and the Orbscan system. Ophthalmology 111:875–879
Tam ES, Rootman DS (2003) Comparison of central corneal thickness measurements by specular microscopy, ultrasound pachymetry, and ultrasound biomicroscopy. J Cataract Refract Surg 29:1179–1184
Wong AC-M, Wong C-C, Yuen NS-Y, Hui S-P (2002) Correlation study of central corneal thickness measurements on Hong-Kong Chinese using optical coherence tomography, Orbscan and ultrasound pachymetry. Eye 16:715–721
Yaylali V, Kaufman SC, Thompson HW (1997) Corneal thickness measurements with the Orbscan Topography System and ultrasonic pachymetry. J Cataract Refract Surg 106:977–981
Author information
Authors and Affiliations
Corresponding author
Additional information
Financial support was obtained from Baskent University, Ankara, Turkey [project # KA05/207]
This study is registered at ClinicalTrials.gov with the registration ID# NCT00439114.
None of the authors has any proprietary or financial interest in any product or device used in this study.
Rights and permissions
About this article
Cite this article
Altan-Yaycioglu, R., Pelit, A. & Akova, Y.A. Comparison of ultrasonic pachymetry with orbscan in corneal haze. Graefes Arch Clin Exp Ophthalmol 245, 1759–1763 (2007). https://doi.org/10.1007/s00417-007-0578-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-007-0578-5