Abstract
Background
The aim of this study was to compare the IgG antibody patterns against retinal antigens in sera of patients with age-related macular degeneration (AMD) and healthy subjects to learn more about possible immunological aspects of this disease and to identify some of the most important antigens.
Methods
Sera of 140 patients were analyzed: healthy volunteers (CO, n=101) and patients with “wet” age-related macular degeneration (AMD, n=39). The sera were tested against western blots of bovine retinal antigens. The IgG antibody patterns were analyzed by multivariate statistical techniques and some antigens were identified via LC-MS/MS.
Results
All patients showed complex patterns of IgG antibodies against retinal antigens. The discriminant analysis revealed a statistical significant difference between the antibody profiles of the AMD and the CO group (P=0.000023). Not only up-regulations of antigen-antibody-reactivities in the AMD group at some molecular weight ranges, e.g. at 46 and 52 kDa, could be seen, but also down-regulations, e.g. at 18 and 36 kDa. The 18 kDa antigen band was identified as αB-crystallin, the band at 46 kDa as α-enolase, and one at 52 kDa as glial fibrillary acidic protein.
Conclusions
We could demonstrate that both groups (wet AMD and CO) show complex IgG antibody patterns against retinal antigens, which are highly specific for each group. This provides further hints for the immunological basis of the disease. These changes in the antibody profiles in “wet” AMD could represent a secondary response to retinal damage or can play a causative role in the disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Age-related macular degeneration (AMD) is the main cause of blindness in the industrialized world [1]. There are two forms of AMD: about 80% of AMD patients have what is considered the “dry” form, where visual cells loose function, and 20% have “wet” AMD, where scarring of the macula due to leaking blood vessels occurs [2, 3]. Both forms cause no pain and have decreased central visual acuity [4].
Changes in the outer retinal complex of the eye can be found in AMD patients. The eyes with “dry” age-related macular degeneration show drusen, alteration of Bruch’s membrane, atrophy, and retinal pigment epithelium changes. Patients with “wet” AMD show disciform scars, retinal pigment epithelial detachments, choroidal neovascularization and membranes [3]. The loss of photoreceptor nuclei and lipofuscin accumulation are generally an age-related phenomenon [5]. However, in AMD you find additional pathogenic extracellular matrix changes (e.g. drusen).
Known risk factors for developing age-related macular degeneration include advanced age, female gender, white race, [6] family history of AMD, [6] cigarette smoking, [7] cardiovascular diseases, hyperopia, and light-colored irises [4].
Right now, no real cure for AMD exists, patients with choroidal neovascularization (=wet AMD) can be treated with laser photocoagulation, which is not suitable for all patients, or photodynamic therapy. Further insight in the pathogenesis of age-related macular degeneration could help to find a better way to detect and treat the disease.
Anti-retinal autoantibodies have been reported in some ocular disorders, including AMD [8, 9]. It is not clear yet, whether autoantibodies play an immediate role in the etiology of age-related macular degeneration or if they are a secondary response to the retinal damage. The causal events responsible for AMD are not known so far. An autoimmune component has been suspected to be a part of the pathogenesis of several ocular pathologies like retinal vasculitis, [10] retinopathy, [11–13] and retinitis pigmentosa [14]. Through this study we are trying to gain more information about a possible autoimmune involvement in the pathogenesis of AMD.
Whatever the cause might be, these antibodies could possibly help to detect age-related macular degeneration at an earlier stage of the disease than today’s methods like Amsler grid test, [4] where people already have a defect of their central vision.
The aim of this study was to analyze the IgG antibody pattern of patients with “wet” age-related macular degeneration in comparison to healthy subjects and to identify some of the important antigens.
Materials and methods
Patients
One hundred forty patients were included in this study; they had complete ophthalmologic examinations at the Ophthalmology Department at the University of Mainz, including slit lamp and retinal examination. Thirty-nine patients with age-related macular degeneration (AMD, mean age 76.4 SD±9) and 101 age-matched healthy volunteers, with no history of eye diseases, serving as control group (CO, mean age 58.2 SD±19), were selected. The investigation was conducted in accordance to the tenets of the Declaration of Helsinki on Biomedical Research involving human subjects.
All AMD patients had “wet” age-related macular degeneration with predominantly classic (>50% classic) subfoveal or juxtafoveal choroidal neovascularization. The greatest linear dimension of the entire lesion did not exceed 5400 μm. The evidence of the classic component was demonstrated via fluorescein angiography using a Heidelberg Retina Angiograph (Heidelberg Engineering, Heidelberg, Germany). Six to 8 pictures were taken of each eye, in the early phase after injection. Then another picture was taken after 15 s as well as after 1, 2, 5, and 10 min. The AMD patients also showed drusen and had a visual acuity of 6/60 or better. AMD patients with pathologic myopia or rip in the retinal pigment epithelium were excluded from this study as well as patients who were not able to obtain fluorescein angiography. Twenty-four of the AMD patients were female and 15 were male, the mean age of the AMD group was 76.4 (SD±9,) and the age ranged from 38 to 88 years.
All control patients (CO) were healthy volunteers with no history of age-related macula degeneration or any other eye disease. Sixty-four of the CO subjects were female and 47 were male, the mean age of the control group was 58.2 (SD±19) and the age ranged from 24 to 90 years.
Exclusion criteria for both groups were: other ocular diseases, diabetes mellitus and retinopathy, retinal detachment, retinal vascular obliteration, and steroid medication.
The two groups were matched for age and gender.
After informed consent was given serum was taken from both groups and centrifuged at 1000 g for ten minutes. The serum was stored at −80°C for later analysis.
Western blot analysis
Retinas were dissected from bovine eyes and homogenized in sample buffer (1M Tris, pH 7.5; 10% SDS; DTT; bromphenol blue, pH 6.8). The samples were first boiled for ten minutes and then centrifuged for one hour and the pellet was discarded. The supernatant was centrifuged and stored at −80°C for later analysis. The bovine retina extracts were used for 13.5% SDS-PAGE using a MultiGel-Long (Biometra, Goettingen, Germany). After electrophoresis the gels were transferred onto nitrocellulose membranes (Schleicher and Schuell, Dassel, Germany) by using a semi-dry blotter (Biometra, Goettingen, Germany). After blotting the membranes for one hour, the quality of the transfer was checked by staining the membranes with PonceauS solution (Sigma, Munich, Germany). The blots were then blocked with blocking buffer [5% non-fat dry milk with Tween20 in phosphate-buffered saline (PBS)] for one hour.
The blots were cut into strips and one strip of nitrocellulose was used per serum sample. The strips were incubated overnight with serum, diluted 1:40 in wash buffer (0.5% non-fat dry milk with Tween20 in PBS), as first antibody. A negative control strip (=one strip incubated only with wash buffer and no serum) and a positive control strip (=sample with known antibody reactivity) were also done for each blot to check the quality of the immunostaining. After washing the strips with Tris-buffered saline (TBS) several times, they were incubated with 1:500 diluted secondary antibody, peroxidase-conjugated Immuno Pure Goat Anti-Human IgG (H+L; Pierce, Illinois, USA), for one hour. After washing the strips with TBS the bands were visualized with 0.05% 4-chloro-1-naphthol (Sigma, Munich, Germany) with 0.015% hydrogen peroxide in 20% methanol in TBS for 20 min. Molecular weights were estimated for each band based on the distance migrated for ten known molecular weight standards (BenchMark, Invitrogen, Karlsruhe, Germany).
Data analysis
The data were acquired using a colour flatbed scanner (Epson GT-9000; Epson, Duesseldorf, Germany). Digital image analysis and evaluation of western blots was performed by BioDocAnalyze (Biometra, Goettingen, Germany), which created densitometry data of the blots showing grey-intensity values versus relative mobility (Rf-values). The Rf-axis (=molecular weight) was broken into 70 classes so that each variable of the vector represents 1/70 of the molecular weight region. For each molecular weight of this 70 class data vector the corresponding grey value of the densitograph of each western blot, which represents the intensity of the antigen-antibody-reaction, was calculated and normalized according to the entire area under the curve. Thus, each variable of the data vector represents the percent area of the peaks of the electrophoretic lane at the corresponding Rf-region.
Based on the densitographs of each western blot multivariate statistical techniques were used to detect differences in the distribution of antibodies against retinal antigens. The densitographic data, such as peak height, localization, and area under the curve were exported to Statistica (Statsoft, Tulsa, Arizona, USA) and the statistical calculations were then performed by Statistica. The profiles were compared by an analysis of discriminance.
This technique has been successfully used as standard protocol to analyze antibody patterns in patients with myasthenia gravis, [15] Tourette syndrome, [16] Sydenham chorea, [17] PANDAS, [18] and glaucoma [19–21].
This digital analysis technique of western blots allows quantitative profiling of many antibodies or antigens at once. The discriminant analysis can calculate the differences between groups and tests whether the antibody pattern of a certain patient is similar to the pattern of a particular group.
LC-MS/MS
Protein identification was performed by MS/MS as described previously [22].
We manually cut the corresponding immunoreactive bands out of the SDS-gel and put them into reaction tubes. The gel pieces were treated with acetonitrile and incubated with 400 μl buffer containing 100 mM ammonium bicarbonate (pH 8.0) for 30 min. The pieces were incubated with 400 μl acetonitrile (50%) containing 100 mM ammonium bicarbonate for one hour before they were incubated with 50 μl acetonitrile (100%) for 15 min. The gel pieces were centrifuged to complete dryness in a Concentrator (Eppendorf, Hamburg, Germany). The individual gel pieces were covered with 10 μl trypsin solution (0.04 μg/μl; Roche, Grenzach-Wyhlen, Germany) for 10 min followed by the addition of 20 μl 25 mM ammonium bicarbonate and incubated for rehydration and digestion (37°C, 7 hr). The digested samples were centrifuged at 13 000 rpm for one minute and the tryptic digests were separated by high performance liquid chromatography (Thermo Electron, Waltham, MA, USA). This liquid chromatography is coupled online to an ion-trap electrospray MS/MS (Thermo Electron, LCQ, Deca Plus).
All MS/MS spectra were converted into Seaquest files and used for data base searches with MASCOT (http://www.matrixscience.com) using NCBI and SwissProt data bases.
Results
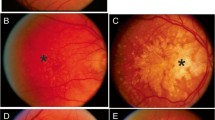
The sera of all patients with age-related macular degeneration (AMD) and all healthy subjects (CO) showed complex staining patterns of IgG antibodies against retinal antigens (Fig. 1). The antibodies we detected were in a molecular weight range from 10 to 180 Kilodalton (kDa).
Western blots of antibody patterns in patients’ sera made visible by Chloronaphthol staining. IgG antibodies against bovine retinal antigens in patients with wet age-related macular degeneration (AMD) and healthy subjects (CO). The molecular weight range (up to 180 kDa) can be seen on the left side. Each strip represents one patient
The analysis of discriminance showed a statistical significant difference between the antibody profiles of patients with age-related macular degeneration and control subjects (P=0.000023).
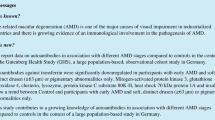
Figure 2 demonstrates the mean antibody reactivity of both groups (AMD and CO) for each molecular weight region. Some antibody peaks are elevated in the AMD group compared to control subjects, for example at about 14, 46, 52, 64 and 82 kDa.
The mean antigen-antibody-reactivity of patients with wet age-related macular degeneration (AMD) and control subjects (CO) were plotted against the corresponding molecular weight of the retinal antigen. A very complex pattern could be found in both groups. The x-axis shows the molecular weight (kDa) and the y-axis the density of the antigen-antibody-reactivity (U) against the retinal antigens
The band at about 52 Kilo Dalton (see Figs. 2, 3a) was identified as glial fibrillary acidic protein (GFAP) via LC-MS/MS. Figure 3a shows the mean number of peaks for both groups at 52 kDa. The AMD group showed a significant increase (8.7±SE) in comparison to control subjects (6.1±SE).
The mean number of peaks with standard deviation (±SE) of the wet age-related macular degeneration group (AMD) and the control group (CO). The x-axis shows the group (CO and AMD) and the y-axis the number of peaks. a The number of peaks at 52 kDa. An up-regulation can be seen in the AMD group (8.7±SE) compared to controls (6.1±SE). b The mean number of peaks at 18 kDa. The number of peaks was decreased in the AMD group (4.7±SE) compared to healthy controls (7.8±SE). c The mean number of peaks at 46 kDa. The AMD group (12.6±SE) showed an up-regulation of antibodies at 46 kDa in comparison to the CO group (6.8±SE)
The antigen at 46 kDa was identified as α-enolase. The AMD group (12.6±SE) had a significant up-regulation at 46 kDa in comparison to healthy controls (6.8±SE; see Fig. 3c).
In some areas a down-regulation of the antibody reactivity of the age-related macular degeneration group compared to healthy subjects could be found, e.g. at 18, 24, 36 and 174 kDa.
The antigen-antibody-reaction at approximately 18 kDa was identified as α-crystallin.
Figure 4 shows the canonical roots of IgG antibodies in the sera of the two groups: patients with age-related macular degeneration (AMD) and control subjects (CO). Canonical roots represent the similarity of the antibody patterns of different patients. The closer the points are to each other, the more similar were the antibody patterns of the western blots of these patients.
Canonical roots of patients with wet age-related macular degeneration (AMD) and healthy subjects (CO). These canonical roots were derived from discriminant analysis and were plotted for each single patient. This two-dimensional graph shows the similarity of the two patient groups. The closer the points to each other, the more similar the antibody patterns were on the western blots of these patients
Discussion
The clinical pathology and natural history of AMD are still not fully understood. To date, there is growing evidence of an autoimmune involvement in the pathogenesis of age-related macular degeneration. Earlier studies could detect an increased level of antibodies against retinal tissue in the sera of AMD patients compared to control subjects [8, 9, 23]. Carboxyethylpyrrole (=CEP) autoantibodies titers were significantly higher in patients with age-related macular degeneration compared to healthy subjects [24]. CEP adducts are produced by the oxidation of docosahexaneoic acid-rich lipids. They identified, e.g. two carboxypropyl pyrrole-modified albumin (HSP) peptides of 1141 and 2021 Dalton by MALDI-TOF.
A significantly elevated level of C-reactive protein (CRP) has been found in patients with intermediate and advanced stages of AMD compared to controls [25]. This may support the hypothesis that inflammation is associated with the pathogenesis of AMD [26]. CRP is a measure of systemic inflammation but may also be associated with local ocular immune function.
A recent study by Patel et al. showed that sera of patients with age-related macular maculopathy and age-related macular degeneration contain autoantibodies to retinal tissue [27]. Anti-retinal antibodies can also be found in other diseases like small-cell cancer of the lung, [28, 29] retinitis pigmentosa, [30, 31] and paraneoplastic retinopathy [11]. It is still not know, if these antibodies are an epiphenomenon or if they are causative for AMD.
Our multivariate statistical methods could calculate complex IgG antibody patterns in the sera of AMD patients and control subjects (Fig. 1). We were able to detect quantitative differences in the antigen-antibody-reactivity of both groups (P=0.000023). Through the multivariate statistical methods used not only up-regulations of some antibody peaks (e.g. at 46 and 52 kDa) in patients with AMD but also down-regulations of other peaks (e.g. at 18 and 24 kDa) could be seen.
We found an up-regulation of the antigen-antibody-reactivity in the AMD group at about 52 kDa compared to the control group (CO; see Fig. 3a). These results correlate with the findings in a study by Chen et al. in which they showed a antibody reactivity at 48 to 52 kDa [23].
The antigen that corresponded with the antibody band we found at 52 kDa was identified as glial fibrillary acidic protein (GFAP). The antibody reactivity at 52 kDa was up-regulated in 44% of the AMD patients (see Fig. 3a). GFAP is the main intermediate filament protein in mature astrocytes [32]. Together with vimentin GFAP can be up-regulated as a response to stress or injury. An increased level of GPAF is found in diseases like multiple sclerosis [33] and lupus erythematosus [34]. In the retina GFAP is found in astrocytes and Mueller cells. Its level increases after optic nerve crush [35] and elevated intraocular pressure [36]. An increased expression of GFAP is also found in Mueller cells of eyes with AMD [37–39]. Anti-GFAP antibodies have already been detected in sera of patients with autism [40]. The existence of anti-GFAP antibodies in sera of AMD patients might be further proof for an autoimmune involvement in this disease, but can also be a consequence of the disease process.
One of the down-regulations of the AMD antibody pattern in comparison to the control group was found at around 18 kDa. This peak was identified as αB-crystallin and was only up-regulated in about 15% of the AMD patients.
α-Crystallins are small heat shock proteins [41], they are found in high concentrations in the lens and function as molecular chaperones. α-Crystallin has been associated with various neurological diseases, e.g. it has been found in the cerebrospinal fluid of patients with multiple sclerosis [42]. Antibodies against α-crystallin have been identified in sera of patients with cataract [43, 44]. In our study, we could demonstrate a down-regulated immunoreactivity against alpha-crystallin in the AMD group in comparison to the control group. Further studies need to address the reasons for this down-regulation of anti-α-crystallin antibodies.
Another antigen we identified in this study was α-enolase (molecular weight: 46 kDa, this peak was up-regulated in 67% of the AMD patients), it is a member of the heat shock protein family and a glycolytic enzyme [45].
Antibodies against α-enolase were identified in sera of patients with rheumatoid arthritis [46], primary membranous nephropathy [47], and lupus erythematosus [46]. Recent publications identified anti-α-enolase antibodies in sera of patients with cancer-associated retinopathy [48] as well as with autoimmune retinopathy [49]. Thus, alpha-enolase is a typical antigen, which is involved in autoimmune processes and therefore provides at least hints for autoimmune mechanisms in AMD.
It has been shown that anti-recoverin antibodies can be found in sera of CAR patients [50] and that they penetrate retinal layers [51, 52]. Recoverin is a Ca2+ binding protein. It could be shown, that the induction of small lung cancer cell lines caused the production of anti-recoverin autoantibodies and retinopathy in animals [53]. It is possible that anti-recoverin antibodies are also the main cause for retina degeneration in patients with CAR. Further studies, e.g. in animal models, will be necessary to find out more about the role antibodies play in the pathogenesis of AMD.
Our multivariate statistical methods could calculate canonical roots that show the similarity between patients with age-related macular degeneration (AMD) and control subjects (CO) in a two-dimensional graph (see Fig. 4). This figure clearly shows a separation of the two groups.
It could be possible that antibodies develop as a result of AMD followed by a secondary loss of retinal ganglion cells. It is not known yet whether those antibodies are causative for the development of the disease or are present as a consequence of the state of AMD. Nevertheless, it is a common practice to search for antibodies against “self-antigens” to prove the hypothesis of an underlying autoimmune mechanism.
It is known that natural autoantibodies occur even in the sera of healthy subjects. The variety of these auto-antigens is very complex [54, 55]. Western blot preparations permit detection of antibody activity directed against specific epitopes and due to our method of analysis we could show differences in the antibody profiles.
“Wet” (=exudative) age-related macular degeneration is the advanced stage of the disease and on that account we chose this subgroup of AMD patients to search for antibodies in this preliminary study. We still need to prove that the antibody profiles we found in sera of patients with wet AMD are similar to the profiles detectable in other forms of AMD and that our results are reproducible in larger study populations. More information will be needed to establish the causative role of these antibodies.
Further studies will be necessary to see if it is possible to distinguish between patients with “wet” and “dry” AMD before it is clinically detectable.
Amabati et al. developed a AMD animal model in mice, these animals were lacking the macrophage chemoattractant Ccl-2 or its congnate receptor Ccr-2 [56]. This model suggests that impaired macrophage recruitment allows accretion of proteins associated with complement activation and immune complex deposition.
The relevance and the role of antibodies in the pathogenesis of AMD are still unknown. Additional studies will be necessary to show if antibodies do appear as a secondary effect during the progression of the disease. Or if antibodies play a causative role during the pathogenesis of AMD. These studies could give new insights into the etiopathology of age-related macular degeneration and might provide new approaches for early detection and therapeutic targets.
References
Evans JR (2001) Risk factors for age-related macular degeneration. Prog Retin Eye Res 20(2):227–253
O’Malley P (1989) Retina and intraocular tumors. In: Vaughan D, Asbury T, Tabbara KF (eds) General ophthalmology, 12th edn. Prentice-Hall, New York
Hyman L (1992) Epidemiology. In: Hampton GR, Nelson PT (eds) Age-related macular degeneration. Raven, New York
Cavallerano AA (1997) Age-related macular degeneration. In: Cavallerano AA, Guntner RK, Oshinskie LJ (eds) Macular disorders. Butterworth-Heinemann, Newton
Kincaid MC (1992) Pathology of AMD. In: Hampton GR, Nelson PT (eds) Age-related macular degeneration. Raven, New York
Klein R, Peto T, Bird A, Vannewkirk MR (2004) The epidemiology of age-related macular degeneration. Am J Ophthalmol 137(3):486–495
Tomany SC, Wang JJ, Van Leeuwen R et al (2004) Risk factors for incident age-related macular degeneration: pooled findings from 3 continents. Ophthalmology 111(7):1280–1287
Penfold PL, Provis JM, Furby JH et al (1990) Autoantibodies to retinal astrocytes associated with age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 228(3):270–274
Gurne DH, Tso MO, Edward DP, Ripps H (1991) Anti-retinal antibodies in serum of patients with age-related macular degeneration. Opthalmology 98(5):602–607
Dumonde DC, Kasp-Grochowska E, Graham E et al (1982) Anti-retinal autoimmunity and circulating immune complexes in patients with retinal vasculitis. Lancet 2(8302):787–792
Adamus G, Ren G, Weleber RG (2004) Autoantibodies against retinal proteins in paraneoplastic and autoimmune retinopathy. BMC Ophthalmol 4(1):5
Savchenko MS, Bazhin AV, Shifrina ON et al (2003) Antirecoverin autoantibodies in the patient with non-small cell lung cancer but without cancer-associated retinopathy. Lung Cancer 41(3):363–367
Heckenlively JR, Fawzi AA, Oversier J et al (2000) Autoimmune retinopathy: patients with antirecoverin immunoreactivity and panretinal degeneration. Arch Ophthalmol 118(11):1525–1533
Galbraith GM, Emerson D, Fudenberg HH et al (1986) Antibodies to neurofilament protein in retinitis pigmentosa. J Clin Invest 78(4):865–869
Zimmermann CW, Grus FH, Dux R (1995) Multivariate statistical comparison of autoantibody-repertoires (western blots) by discriminant analysis. Electrophoresis 16(6):941–947
Wendlandt JT, Grus FH, Hansen BH, Singer HS (2001) Striatal antibodies in children with Tourette’s syndrome: multivariate discriminant analysis of IgG repertoires. J Neuroimmunol 119(1):106–113
Singer HS, Loiselle CR, Lee O et al (2003) Anti-basal ganglia antibody abnormalities in Sydenham chorea. J Neuroimmunol 136(1–2):154–161
Singer HS, Loiselle CR, Lee O et al (2004) Anti-basal ganglia antibodies in PANDAS. Mov Disord 19(4):406–415
Grus FH, Joachim SC, Hoffmann EM, Pfeiffer N (2004) Complex autoantibody repertoires in patients with glaucoma. Mol Vis 10:132–137
Joachim SC, Grus FH, Pfeiffer N (2003) Analysis of autoantibody repertoires in sera of patients with glaucoma. Eur J Ophthalmol 13(9–10):752–758
Joachim SC, Pfeiffer N, Grus FH (2005) Autoantibodies in patients with glaucoma: a comparison of IgG serum antibodies against retinal, optic nerve, and optic nerve head antigens. Graefes Arch Clin Exp Ophthalmol 243(8):817–823
Grus FH, Joachim SC, Bruns K et al (2006) Serum Autoantibodies to {alpha}-Fodrin Are Present in Glaucoma Patients from Germany and the United States. Invest Ophthalmol Vis Sci 47(3):968–976
Chen H, Wu L, Pan S, Wu DZ (1993) An immunologic study on age-related macular degeneration. Yan Ke Xue Bao 9(3):113–120
Gu X, Meer SG, Miyagi M et al (2003) Carboxyethylpyrrole protein adducts and autoantibodies, biomarkers for age-related macular degeneration. J Biol Chem 278(43):42027–42035
Seddon JM, Gensler G, Milton RC et al (2004) Association between C-reactive protein and age-related macular degeneration. Jama 291(6):704–710
Anderson DH, Mullins RF, Hageman GS, Johnson LV (2002) A role for local inflammation in the formation of drusen in the aging eye. Am J Ophthalmol 134(3):411–431
Patel N, Ohbayashi M, Nugent AK et al (2005) Circulating anti-retinal antibodies as immune markers in age-related macular degeneration. Immunology 115(3):422–430
Luiz JE, Lee AG, Keltner JL et al (1998) Paraneoplastic optic neuropathy and autoantibody production in small-cell carcinoma of the lung. J Neuroophthalmol 18(3):178–181
Jankowska R, Witkowska D, Porebska I et al (2004) Serum antibodies to retinal antigens in lung cancer and sarcoidosis. Pathobiology 71(6):323–328
Brinkman CJ, Pinckers AJ, Broekhuyse RM (1980) Immune reactivity to different retinal antigens in patients suffering from retinitis pigmentosa. Invest Ophthalmol Vis Sci 19(7):743–750
Kumar M, Gupta RM, Nema HV (1983) Role of autoimmunity in retinitis pigmentosa. Ann Ophthalmol 15(9):838–840
Lewis GP, Fisher SK (2003) Up-regulation of glial fibrillary acidic protein in response to retinal injury: its potential role in glial remodeling and a comparison to vimentin expression. Int Rev Cytol 230:263–290
Norgren N, Sundstrom P, Svenningsson A et al (2004) Neurofilament and glial fibrillary acidic protein in multiple sclerosis. Neurology 63(9):1586–1590
Sanna G, Piga M, Terryberry JW et al (2000) Central nervous system involvement in systemic lupus erythematosus: cerebral imaging and serological profile in patients with and without overt neuropsychiatric manifestations. Lupus 9(8):573–583
Chen H, Weber AJ (2002) Expression of glial fibrillary acidic protein and glutamine synthetase by Muller cells after optic nerve damage and intravitreal application of brain-derived neurotrophic factor. Glia 38(2):115–125
Lam TT, Kwong JM, Tso MO (2003) Early glial responses after acute elevated intraocular pressure in rats. Invest Ophthalmol Vis Sci 44(2):638–645
Madigan MC, Penfold PL, Provis JM et al (1994) Intermediate filament expression in human retinal macroglia. Histopathologic changes associated with age-related macular degeneration. Retina 14(1):65–74
Guidry C, Medeiros NE, Curcio CA (2002) Phenotypic variation of retinal pigment epithelium in age-related macular degeneration. Invest Ophthalmol Vis Sci 43(1):267–273
Wu KH, Madigan MC, Billson FA, Penfold PL (2003) Differential expression of GFAP in early v late AMD: a quantitative analysis. Br J Ophthalmol 87(9):1159–1166
Singh VK, Warren R, Averett R, Ghaziuddin M (1997) Circulating autoantibodies to neuronal and glial filament proteins in autism. Pediatr Neurol 17(1):88–90
Klemenz R, Frohli E, Steiger RH et al (1991) Alpha B-crystallin is a small heat shock protein. Proc Natl Acad Sci USA 88(9):3652–3656
Stoevring B, Vang O, Christiansen M (2005) (alpha)B-crystallin in cerebrospinal fluid of patients with multiple sclerosis. Clin Chim Acta 356(1–2):95–101
Garcia-Castineiras S, Andino Moreno ME, Perez R, Vazquez LA (1993) Antibodies to lens crystallins after endocapsular cataract surgery. P R Health Sci J 12(2):123–128
Sandberg HO, Closs O (1979)The humoral immune response to alpha, beta and gamma crystallins of the human lens. Scand J Immunol 10(6):549–554
Iida H, Yahara I (1985) Yeast heat-shock protein Mr 48,000 is a isoprotein of enolase. Nature 315:688–690
Pratesi F, Moscato S, Sabbatini A et al (2000) Autoantibodies specific for alpha-enolase in systemic autoimmune disorders. J Rheumatol 27(1):109–115
Wakui H, Imai H, Komatsuda A, Miura AB (1999) Circulating antibodies against alpha-enolase in patients with primary membranous nephropathy (MN). Clin Exp Immunol 118(3):445–450
Dot C, Guigay J, Adamus G (2005) Anti-alpha-enolase antibodies in cancer-associated retinopathy with small cell carcinoma of the lung. Am J Ophthalmol 139(4):746–747
Weleber RG, Watzke RC, Shults WT et al (2005) Clinical and electrophysiologic characterization of paraneoplastic and autoimmune retinopathies associated with antienolase antibodies. Am J Ophthalmol 139(5):780–794
Thirkill CE, Tait RC, Tyler NK et al (1992) The cancer-associated retinopathy antigen is a recoverin-like protein. Invest Ophthalmol Vis Sci 33(10):2768–2772
Ren G, Adamus G (2004) Cellular targets of anti-alpha-enolase autoantibodies of patients with autoimmune retinopathy. J Autoimmun 23(2):161–167
Bazhin AV, Schadendorf D, Philippov PP, Eichmuller SB (2006) Recoverin as a cancer-retina antigen. Cancer Immunol Immunother pp 1–7
Thirkill CE (1997) Experimental, cancer-induced retinopathy. Ocul Immunol Inflamm 5(1):55–65
Avrameas S (1991) Natural autoantibodies: from ‘horror autotoxicus’ to ‘gnothi seauton’. Immunol Today 12(5):154–159
Lacroix-Desmazes S, Kaveri SV, Mouthon L et al (1998) Self-reactive antibodies (natural autoantibodies) in healthy individuals. J Immunol Methods 216(1–2):117–137
Ambati J, Anand A, Fernandez S et al (2003) An animal model of age-related macular degeneration in senescent Ccl-2- or Ccr-2-deficient mice. Nat Med 9(11):1390–1397
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by MAIFOR and “Schwerpunkt Praeventive Medizin” University of Mainz.
Rights and permissions
About this article
Cite this article
Joachim, S.C., Bruns, K., Lackner, K.J. et al. Analysis of IgG antibody patterns against retinal antigens and antibodies to α-crystallin, GFAP, and α-enolase in sera of patients with “wet” age-related macular degeneration. Graefe's Arch Clin Exp Ophthalmol 245, 619–626 (2007). https://doi.org/10.1007/s00417-006-0429-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-006-0429-9