Abstract
Background
Retinitis pigmentosa belongs to a large group of degenerative diseases of the retina with a hereditary background. It involves loss of retinal photoreceptor cells and consequently peripheral vision. At present there are no satisfactory therapeutic options for this disease. Just recently the use of mesenchymal stem cells has been discussed as one therapeutical option for retinal degeneration, as they have been shown to differentiate into various cell types, including photoreceptor cells. In this article we wanted to investigate the potency of mesenchymal stem cells to induce rescue effects in an animal model for retinitis pigmentosa, the rhodopsin knockout mouse.
Methods
For the experiments, three experimental groups of 10 animals each were formed. The first group consisted of untreated rhodopsin knockout (rho-/-) animals used as controls. The second group consisted of rho-/- mice that had received an injection of mouse mesenchymal stem cells, which were transduced using an adenoviral vector containing the sequence for the green fluorescent protein (GFP) prior to transplantation. In the third sham group, animals received an injection of medium only. Thirty-five days after transplantation, GFP-expressing cells were detected in whole-mount preparations of the retinas as well as in cryostat sections. For the detection of rescue effects, semi-thin sections of eyes derived from all experimental groups were produced. Furthermore, rescue effects were also analysed ultrastructurally in ultrathin sections.
Results
Histological analysis revealed that after transplantation, cells morphologically integrated not only into the retinal pigment epithelium but also into layers of the neuroretina displaying neuronal and glial morphologies. Furthermore, significant rescue effects, as demonstrated by the occurrence of preserved photoreceptor cells, were detected.
Conclusions
Our data indicate that mesenchymal stem cells can prolong photoreceptor survival in the rhodopsin knockout mouse, also providing evidence of a therapeutical benefit in retinitis pigmentosa.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Retinitis pigmentosa is one of the most genetically heterogeneous groups of blinding diseases resulting from loss of photoreceptors with a preference for rod-mediated vision. To date there has been no successful treatment for this retinal disorder. This is the reason behind intensive research working to establish alternative therapeutical concepts for the treatment of this complex disease. Some of these concepts include the delivery of neurotrophic factors to protect photoreceptors from degeneration either by direct injection or using gene therapy approaches [13, 14, 23]. Furthermore, the use of stem cells as a therapeutical option in degenerative diseases of the retina such as retinitis pigmentosa has also been debated recently [15, 21, 32]. Using stem cells for cell replacement strategies, there are two cell types that have been characterised fairly well in recent years. One of them is the embryonic stem cell derived from the inner cell mass of the pre-implantation blastocyst, which has the potency to differentiate into cell derivatives of all three germ layers. However, in our own investigations we were able to show that ES cells bear an incalculable risk as they show an ectopic differentiation tendency, forming teratomas after subretinal transplantation, even after a thorough selection procedure [4]. The other and most promising group of stem cells are those isolated from the adult organism. In fact, just recently it has been shown that bone marrow-derived hematopoietic stem cells have the potency to rescue retinas from degeneration in two appropriate mouse models [28]. The group of bone marrow derived adult stem cells also includes mesenchymal stem cells (MSCs), which have recently experienced a high level of attention as they can be easily isolated and obtained in almost unlimited numbers [9, 25]. Furthermore, they show some neural characteristics in vitro and in vivo [5] and differentiate into astrocyte-like cells in vivo when transplanted into the normal or ischaemic brain [6, 12, 22]. Additionally, the intravenous injection of BMSCs into mice has been shown to induce neuronal differentiation in the brain [8, 11, 27]. Moreover, there are also reports about a photoreceptor differentiation of MSCs [19]. In order to investigate whether there is also a rescue potential of MSCs in retinitis pigmentosa, we used the rhodopsin knockout mouse as a model. In this animal, the retina has a normal complement of photoreceptor cells at birth, although rod outer segments never develop [17]. During the postnatal development there is a continuous degeneration of photoreceptors resulting in a complete loss [33].
Our data indicate that the subretinal transplantation of MSCs 35 days postnatally, before the loss of the majority of photoreceptor cells is complete, results in the morphological integration of the MSCs into various layers of the retina, inducing significant rescue efforts.
Materials and methods
Isolation and cultivation of mesenchymal stem cells
As the rhodopsin knockout mouse used in this study was derived from a 129 mouse background, donor mesenchymal stem cells were also taken from 129 mice (Harlan-Winkelmnn, Borchen, Germany). Animals were maintained in a 12/12 h light/dark cycle.
Mesenchymal stem cells were isolated using bone marrow aspirates from the femur bones of male adult mice.
Cell material was diluted 1:1 with DMEM low glucose and filtered through a 70-μm nylon mesh (Cell Strainer, Falcon; Becton Dickinson, Franklin Lakes, NJ, USA). The resulting cell suspension was layered on top of 15 ml Ficoll-Paque Plus (Amersham Pharmacia Biotech, Uppsala, Sweden) and centrifuged for 30 min at 800×g at room temperature. The supernatant and interface were combined, diluted to about 50 ml with PBS (0.1 M) and centrifuged for 10 min at 800×g. After discarding the supernatant, the pellet was suspended in 1 ml medium. The nucleated cells were counted, suspended at a concentration of 1×107/ml in growth medium (DMEM supplemented with 2 mg/ml L-glutamine, 50 μg/ml streptomycin and 10% (v/v) of non-heat inactivated fetal calf serum) and plated at 3×106/cm2 in 100-mm culture dishes (Falcon; Becton Dickinson). The cells were incubated for 3 days, and the non-adherent cells were removed by replacing the medium in three washing steps. After the cultures reached confluence, the cells were lifted by incubation with Accutase (PAA, Cölbe, Germany) at 37°C for 3–4 min. They were diluted and plated at a density of 2,000 cells/cm2 in 100-mm culture dishes.
Construction of HC-Ad vectors and cell labelling
The high-capacity adenoviral vector (HC-Ad) was generated as previously described [10]. The vector HC-Ad.FK7 expressing enhanced GFP (EGFP—enhanced green fluorescent protein) has also been described [10]. BMSCs were infected using a stock AdV concentration of 2×106 infectious units/μl, corresponding to 50 multiplicities of infection (MOI) for a single cell. Transduction efficiency was analysed 24 h after transduction by determining the population of cells with EGFP expression within the total cell population labelled by the Hoechst dye nuclear stain.
Alternatively, as a control, cells were labelled using the cell membrane dye PKH 67 (Sigma, Deisenhofen, Germany).
Animals, transplantation and tissue preparation
All procedures were performed in accordance with the principles of laboratory animal care as well as in accordance with the current version of the German Law on the Protection of Animals.
In order to gain statistically relevant results in each experimental group, ten 35-day-old animals were used. Mice were anaesthetised with an intraperitoneal injection of Ketanest/Rompun. Only the right eyes were used for cell injections. Sixty thousand vector-transduced mesenchymal stem cells were injected in a volume of 0.5 μl medium with a Hamilton syringe and a 30-gauge needle 1 mm from the limbus into the subretinal space of the right eye of rhodopsin knockout mice. The contralateral eye remained untreated. Alternatively, for sham operations the same volume (0.5 μl) of Hank’s balanced salt solution (HBSS) was injected.
In order to exclude false-positive cell tagging by the possible occurrence of free vector particles, four animals received injections of MSCs that were labelled by the membrane dye PKH67 prior to grafting instead of using the GFP vector.
In all experimental groups the retinas were examined funduscopically using a Leitz stereo-microscope (Leitz, Wetzlar, Germany) after the injection, and eyes showing massive subretinal haemorrhage, vitreous haemorrhage, or large retinal detachments were discarded. Thirty-five days after transplantation (70 days after birth), the eyes were enucleated and fixed in 4% paraformaldehyde in 0.1 M phosphate buffered saline (PBS), and flat-mount preparations of the retina including the retinal pigment epithelial (RPE) layer were examined. To detect injected cells and to determine the extent of the transplant site, the flat mounts were examined and photographed by fluorescence microscopy (Zeiss Axiophot; Zeiss, Oberkochen, Germany).
Immunohistochemical staining procedures
In order to investigate marker expression in transplanted GFP expressing MSCs within the flat-mount preparations, the MSCs were treated with blocking antibodies of 2% goat serum and 5% FBS for 30 min.
In experiments requiring the labelling of cytoplasmic marker proteins, the cells were further treated with 0.025% Triton X-100 for 30 min and rinsed in PBS.
The following primary antibodies were used: anti-pan cytokeratin (Sigma) 1:1000, anti Map-2 (Sigma) 1:100, and anti GFAP (Progen, Heidelberg, Germany) 1:1000. Incubations were performed overnight at 4°C. Secondary antibodies were used at the following dilutions: Cy3-conjugated affinity-purified goat anti-mouse or anti-rabbit IgG (Rockland; Gilbertsville, PA, USA) 1:1000.
Light and electron microscopy and evaluation of rescue effects
For light- and electron microscopical investigations, the enucleated eyes were processed as follows. After removal of the corneas the eyes were fixed overnight at 4°C in glutaraldehyde (4% solution in 0.1 M cacodylate buffer, pH 7.4). Fluorescent areas in flat-mount preparations were excised and post-fixed with 1% osmium tetroxide at room temperature in 0.1 M cacodylate buffer for 3 h, stained en bloc with uranyl acetate. Dehydration was then performed by a series of incubations in the following order: ethanol 50% (30 min), ethanol 70% (overnight), ethanol 96% (3×20 min), absolute ethanol (3×20 min), acetone (3×20 min) and acetone + Araldite (overnight). The eyes were then embedded in Araldite for 48 h. Semi-thin sections (0.7 μm) were produced from the region of the transplant using a Reichert Ultracut R ultrathome (Leitz). Sections were stained using methylene blue dye (Sigma). A temporal-nasal orientation was maintained throughout the section procedure. Rescue effects were quantified using an Axiophot light microscope (Zeiss) in representative sections adjacent to or within 300 μm of the injection site. Average cell numbers of preserved photoreceptor nuclei for each retina were established by counting the number of cells in a 100-μm region of the outer nuclear layer (using an eyepiece graticule and viewing the stained section with a ×40× oil immersion lens) resulting in a final magnification of ×400. Care was taken to avoid the outer quarter to third of the retina where the retinal layers became thinner. The evaluation was carried out blinded and counts were made every 20 sections so that 10 counts were made per eye throughout the experimental groups.
Additionally, ultrathin sections (70 nm) were obtained from each group stained with uranyl acetate and lead citrate and were observed under an electron microscope (model 902 A; Zeiss).
Statistical analysis
Data and statistical analysis were performed using Microsoft Excel software (Seattle, WA, USA). Data are given as mean ± SEM. Comparison between the two groups was made using the Student’s t test. For all statistical tests p<0.05 was considered significant.
Results
Mesenchymal stem cells
Mouse mesenchymal stem cells were cultivated according to the above mentioned procedure. After adhesion to the plastic culture dish, MSCs exhibited the typical spindle-like morphology and were arranged in a foray fashion. The adhesion to the culture dish also served as a criterion to distinguish MSCs from free floating hematopoietic cells (Fig. 1a). Further characterisation was performed by the immunocytochemical detection of the cell surface marker CD90 specifically expressed in MSCs. These investigations revealed a proportion of more than 85% of MSCs positive for this marker protein of mesenchymal stem cells (Fig. 1b).
Morphological and immunocytochemical analysis of cultivated mouse mesenchymal stem cells (MSCs). a Phase contrast microscopy of mouse MSCs in the cell culture dish 3 days after plating. b Immunocytochemical detection of the stem cell marker CD90 in MSCs 5 days after plating. Scale bar = 20 μm in a and 15 μm in b
Subretinal transplantation of mesenchymal stem cells in rho-/- mice
In order to study the adaptive quality and integrative potency of GFP-labelled MSCs in the recipient tissue of the retina, they were injected microsurgically into the subretinal space of 35-day-old rho-/- mice.
Transplantation success could be investigated by detection of GFP expression in the fundus of the eye directly after cell injection using a stereofluorescence microscope (not shown). After a survival time of 35 days, the animals were sacrificed and the eyes enucleated. In flat-mount preparations of the retinas including the retinal pigment epithelial layer, MSCs could be easily identified due to their GFP expression (Fig. 2a). Cells showed an integrative potential within the retinal pigment epithelium, exhibiting the typical hexagonal shape of RPE cells (Fig. 2b). Immunohistochemical investigations demonstrated that the GFP-expressing cells (Fig. 2c), which had integrated within the RPE layer, showed a co-labelling for cytokeratin similar to the surrounding local RPE cells (Fig. 2d,e). Furthermore, formation of cell contacts of GFP-expressing MSCs (Fig. 2f) with the neighbouring RPE cells was demonstrated by the expression of the tight junction protein ZO-1 (Fig. 2g,h).
Detection of vector-transduced MSCs in whole mount preparations of the dystrophic retina after subretinal transplantation. a Green fluorescent protein (GFP)-expressing cells can be detected in the retinal pigment epithelial layer, the cells show the typical hexagonal morphologies of retinal pigment epithelial (RPE) cells. b Higher magnification of hexagonal GFP-expressing cells. c Grafted GFP-expressing MSCs. d, e expressing the epithelial marker cytokeratin as well as the surrounding host cells. f GFP-expressing MSCs. g Taking up close contacts with the neighbouring host cells as demonstrated by the expression of the tight junction marker ZO-1. h Merged. Scale bar: a = 40 μm, b = 20 μm, c–e = 12 μm, f–h = 15 μm
Evaluation of rescue effects
Thirty-five days after the subretinal injection of MSCs into the subretinal space of the dystrophic eyes, marked rescue effects could be detected in semi-thin sections of flat-mount preparations of retinas that were subjected to cell injection. These rescue effects were deduced from the occurrence of several rows of photoreceptor nuclei, which were preserved in the vicinity of MSC transplants that had been transduced by the GFP vector in vitro prior to cell injection. In contrast, in the control eyes of non-treated animals or sham-operated animals that had only received injection of medium without cells, hardly any photoreceptor nuclei were detected (Fig. 3a–c). In the sections obtained from the eyes that had received MSCs, the number of photoreceptor nuclei per 300 μm of retinal length facing transplants was significantly higher (14±1.7, p≤0.05) compared with the control group (2.1±1.2) as well as with the sham-operated group (2.8±3.1) (Fig. 4a). Consequently, analysis of rows of preserved photoreceptors revealed that after transplantation of MSCs there are 2.25±0.4 rows compared with 0.4±0.3 rows in the controls and 0.9±0.3 in the sham-operated animals (Fig. 4b).
Semi-thin sections of rho-/- retinas for the demonstration of rescue effects, the ganglion cell layer is at the top. a In the retina of an untreated control there are no photoreceptor cell nuclei detectable. b After injection of GFP vector transduced MSCs there are several rows of preserved photoreceptor cells (arrows). c In sham-operated retinas, similar to untreated controls, there are hardly any photoreceptor cells detectable. Scale bar = 70 μm
Quantification and statistical analysis of rescue effects. a Quantification of the number of photoreceptor cells also reveals a significant increase after transplantation in vector-transduced MSCs compared with the control groups. b Analysis of rows of preserved photoreceptor cells per 300 μm length of the retina also shows a significant increase concerning this parameter compared with the controls
Electron microscopic investigation of retinas after MSC grafting confirmed findings as observed on light microscopical level in semi-thin sections. While in untreated control preparations no photoreceptor cell nuclei are detectable (Fig. 5a), there are several receptor nuclei in MSC-treated rho-/- mice. Some of the photoreceptor cells reveal rudimentary inner segments (Fig. 5b). The occurrence of several rows of preserved photoreceptor cell nuclei in our ultrastructural investigations indicates a rescue effect on photoreceptor cell nuclei after subretinal MSC transplantation.
Ultrastructural analysis of the dystrophic retina under control conditions and after MSC grafting. a As already detected in the Semi-thin sections of the control retinas, there are neither photoreceptor nuclei nor receptor outer segments detectable. b After subretinal transplantation there are numerous preserved photoreceptor cell nuclei as well as rudimentary inner segments present. Inset: mesenchymal stem cell situated on top of the RPE layer. There is an artificial detachment of outer segments from the RPE layer due to the cell injection procedure. Scale bar in a and b = 2.5 μm and in the inset = 0.5 μm
Discussion
To date there has been no effective treatment to improve the fatal process of degenerative retinal diseases such as retinitis pigmentosa (RP). However, recent progress in basic research in ophthalmology has initiated the development of novel therapeutic options for retinal degenerations [1]. Thus, in addition to gene therapy using different viral and non-viral vectors [2, 3, 7], another novel therapeutic strategy could be the application of cell-based options with stem cells, or the combination of both methods. This is increasingly being discussed as a suitable therapy for the improvement of visual defects, such as those of RP [28].
In this respect the results of our study support the possible implementation of a cell-based strategy using mesenchymal stem cells for the treatment of various retinal defects. We show here that bone marrow-derived mesenchymal stem cells, which were transduced using an adenoviral vector carrying the sequence for the GFP prior to grafting, can very easily be identified by their vector-induced GFP expression. They have the potency to integrate within the retina of dystrophic rhodopsin knockout mice after subretinal transplantation. Integration of MSCs, preferably within the RPE layer, together with a transdifferentiation capacity of MSCs into pigment epithelial-like cells and a characteristic marker expression such as cytokeratin can be shown. Although there are also single GFP-expressing cells to be found in additional retinal layers, an integration of MSCs within the RPE suggests a strong tendency of MSCs to home in on this epithelial compartment. Similar findings regarding a homing in of MSCs in an epithelial context have been shown in the kidney. In this organ MSCs integrated into the tubular epithelium and expressed cytokeratin, indicating a differentiation into tubular epithelial cells [16].
The integrative capacity of MSCs into the retina can be exploited for the establishment of a future cure for retinal degenerations, as from this localisation in the rho-/- mouse model, MSCs have the capacity to slow down photoreceptor degeneration until at least postnatal day 70. These rescue effects can be shown histologically by the occurrence of preserved photoreceptor cell nuclei in the vicinity of the injection site. Photoreceptor nuclei neither occur in appropriate non-treated controls nor after sham surgery, which is in contrast to reports on sham surgery effects observed after similar experimental approaches using, for example, Schwann cells as grafts, also in the rho-/- mouse model [18, 24].
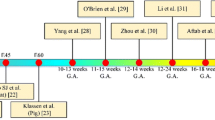
In contrast to similar studies by our group demonstrating rescue effects after transplantation of embryonic stem cells or iris pigment epithelial (IPE) cells in Royal College of Surgeons (RCS) rats, where the primary defect tends to be associated with the RPE cells [29–31] (our own unpublished data), the data presented here are most interesting, as in RP, as well as in the rho-/- mouse, the defect is situated in the photoreceptor cells themselves.
In fact, our results obtaining rescue effects after transplantation of bone marrow-derived stem cells in the subretinal space of rho-/- mouse are in line with reports by Otani et al. [28]. In contrast to our study, however, they implanted lineage-negative hematopoietic stem cells in the retinal degeneration (rd) mouse, which is also a well-established animal model for retinitis pigmentosa. These hematopoietic stem cells, however, contain endothelial precursor cells that primarily stabilize and rescue retinal blood vessels that would otherwise degenerate and secondarily induce neurotrophic rescue effects by preserving retinal nuclear layers. In an approach more closely related to our experimental procedure, it has been shown that CD 90+ bone marrow-derived stromal cells, after stimulation with activin A, taurin and EGF, have the potency to integrate within the host retina of RCS rats, forming structures similar to the photoreceptor layer, expressing photoreceptor-specific markers, although without evaluating rescue effects in the RCS model [20].
From the characterisation of bone marrow-derived MSCs, it is well known that they also have the ability to synthesize neurotrophic factors, which can even be stimulated applying cultivation protocols suitable for the selection and expansion of neural stem cells [5]. Furthermore, according to our own unpublished ELISA data from rat and human MSCs, they even synthesize the pigment epithelial factor, which is very likely to promote photoreceptor cell survival.
Therefore, it can be assumed that although there seems to be a morphological integration of MSCs within the retinal pigment epithelium, together with a limited transdifferentiation capacity of MSCs even into pigment epithelial-like cells including an appropriate marker expression, the rescue effects detected in our study are mainly due to the synthesis of trophic factors by the injected MSCs. As mentioned before, a similar effect has been shown after the grafting of Schwann cells into the rho -/- mouse [18]. Similar to MSCs, Schwann cells also synthesise a variety of trophic factors; thus, it can be assumed that in parallel to Schwann cells, MSCs serve as a kind of bioreactor for the production of therapeutic substances after transplantation. The advantage of using MSCs, though, is their autologous availability.
Nevertheless, in all cell or gene therapeutic approaches in the rho-/- mouse, the formation of outer segments has never been observed, neither after transplantation of Schwann cells [18] nor after treatment using an adeno-associated virus carrying the sequence of the ciliary neurotrophic factor [26].
Together with findings from studies using other cell-based treatment modalities, data from our experiments involving MSCs indicate that the rescue effects achieved are only a partial success, pointing in the direction of photoreceptor cell protection. However, further work needs to be performed in order to actually prove a functional recovery of photoreceptor cell survival.
References
Abegg M, Hafezi F, Wenzel A, Grimm C, Reme CE (2000) Therapeutic strategies in RP (retinitis pigmentosa): light at the end of the tunnel?. Klin Monatsbl Augenheilkd 216:83–89
Ali RR, Reichel MB, Thrasher AJ, Levinsky RJ, Kinnon C, Kanuga N, Hunt DM, Bhattacharya SS (1996) Gene transfer into the mouse retina mediated by an adeno-associated viral vector. Hum Mol Genet 5:591–594
Ali RR, Reichel MB, De Alwis M, Kanuga N, Kinnon C, Levinsky RJ, Hunt DM, Bhattacharya SS, Thrasher AJ (1998) Adeno-associated virus gene transfer to mouse retina. Hum Gene Ther 9:81–86
Arnhold S, Klein H, Semkova I, Addicks K, Schraermeyer U (2004) Neurally selected embryonic stem cells induce tumor formation after long-term survival following engraftment into the subretinal space. Invest Ophthalmol Vis Sci 45:4251–4255
Arnhold S, Klein H, Klinz FJ, Absenger Y, Schmidt A, Schinkothe T, Brixius K, Kozlowski J, Desai B, Bloch W, Addicks K (2006) Human bone marrow stroma cells display certain neural characteristics and integrate in the subventricular compartment after injection into the liquor system. Eur J Cell Biol 85:551–565
Azizi SA, Stokes D, Augelli BJ, DiGirolamo C, Prockop DJ (1998) Engraftment and migration of human bone marrow stromal cells implanted in the brains of albino rats—similarities to astrocyte grafts. Proc Natl Acad Sci USA 95:3908–3913
Bennett J, Tanabe T, Sun D, Zeng Y, Kjeldbye H, Gouras P, Maguire AM (1996) Photoreceptor cell rescue in retinal degeneration (rd) mice by in vivo gene therapy. Nat Med 2:649–654
Brazelton TR, Rossi FM, Keshet GI, Blau HM (2000) From marrow to brain: expression of neuronal phenotypes in adult mice. Science 290:1775–1779
Devine SM (2002) Mesenchymal stem cells: will they have a role in the clinic? J Cell Biochem Suppl 38:73–79
Dinser R, Kreppel F, Zaucke F, Blank C, Paulsson M, Kochanek S, Maurer P (2001) Comparison of long-term transgene expression after non-viral and adenoviral gene transfer into primary articular chondrocytes. Histochem Cell Biol 116:69–77
Eglitis MA, Mezey E (1997) Hematopoietic cells differentiate into both microglia and macroglia in the brains of adult mice. Proc Natl Acad Sci USA 94:4080–4085
Eglitis MA, Dawson D, Park KW, Mouradian MM (1999) Targeting of marrow-derived astrocytes to the ischemic brain. Neuroreport 10:1289–1292
Faktorovich EG, Steinberg RH, Yasumura D, Matthes MT, LaVail MM (1992) Basic fibroblast growth factor and local injury protect photoreceptors from light damage in the rat. J Neurosci 12:3554–3567
Frasson M, Picaud S, Leveillard T, Simonutti M, Mohand-Said S, Dreyfus H, Hicks D, Sabel J (1999) Glial cell line-derived neurotrophic factor induces histologic and functional protection of rod photoreceptors in the rd/rd mouse. Invest Ophthalmol Vis Sci 40:2724–2734
Haruta M (2005) Embryonic stem cells: potential source for ocular repair. Semin Ophthalmol 20:17–23
Herrera MB, Bussolati B, Bruno S, Fonsato V, Romanazzi GM, Camussi G (2004) Mesenchymal stem cells contribute to the renal repair of acute tubular epithelial injury. Int J Mol Med 14:1035–1041
Humphries MM, Rancourt D, Farrar GJ, Kenna P, Hazel M, Bush RA, Sieving PA, Sheils DM, McNally N, Creighton P, Erven A, Boros A, Gulya K, Capecchi MR, Humphries P (1997) Retinopathy induced in mice by targeted disruption of the rhodopsin gene. Nat Genet 15:216–219
Keegan DJ, Kenna P, Humphries MM, Humphries P, Flitcroft DI, Coffey PJ, Lund RD, Lawrence JM (2003) Transplantation of syngeneic Schwann cells to the retina of the rhodopsin knockout (rho(-/-)) mouse. Invest Ophthalmol Vis Sci 44:3526–3532
Kicic A, Shen WY, Wilson AS, Constable IJ, Robertson T, Rakoczy PE (2003) Differentiation of marrow stromal cells into photoreceptors in the rat eye. J Neurosci 23:7742–7749
Kicic A, Shen WY, Wilson AS, Constable IJ, Robertson T, Rakoczy PE (2003) Differentiation of marrow stromal cells into photoreceptors in the rat eye. J Neurosci 23:7742–7749
Kociok N (2005) Can the injection of the patient’s own bone marrow-derived stem cells preserve cone vision in retinitis pigmentosa and other diseases of the eye? Graefes Arch Clin Exp Ophthalmol 243:187–188
Kopen GC, Prockop DJ, Phinney DG (1999) Marrow stromal cells migrate throughout forebrain and cerebellum, and they differentiate into astrocytes after injection into neonatal mouse brains. Proc Natl Acad Sci USA 96:10711–10716
LaVail MM, Unoki K, Yasumura D, Matthes MT, Yancopoulos GD, Steinberg RH (1992) Multiple growth factors, cytokines, and neurotrophins rescue photoreceptors from the damaging effects of constant light. Proc Natl Acad Sci USA 89:11249–11253
Lawrence JM, Keegan DJ, Muir EM, Coffey PJ, Rogers JH, Wilby MJ, Fawcett JW, Lund RD (2004) Transplantation of Schwann cell line clones secreting GDNF or BDNF into the retinas of dystrophic Royal College of Surgeons rats. Invest Ophthalmol Vis Sci 45:267–274
Lee HS, Huang GT, Chiang H, Chiou LL, Chen MH, Hsieh CH, Jiang CC (2003) Multipotential mesenchymal stem cells from femoral bone marrow near the site of osteonecrosis. Stem Cells 21:190–199
Liang FQ, Dejneka NS, Cohen DR, Krasnoperova NV, Lem J, Maguire AM, Dudus L, Fisher KJ, Bennett J (2001) AAV-mediated delivery of ciliary neurotrophic factor prolongs photoreceptor survival in the rhodopsin knockout mouse. Mol Ther 3:241–248
Mezey E, Chandross KJ (2000) Bone marrow: a possible alternative source of cells in the adult nervous system. Eur J Pharmacol 405:297–302
Otani A, Dorrell MI, Kinder K, Moreno SK, Nusinowitz S, Banin E, Heckenlively J, Friedlander M (2004) Rescue of retinal degeneration by intravitreally injected adult bone marrow-derived lineage-negative hematopoietic stem cells. J Clin Invest 114:765–774
Schraermeyer U, Kociok N, Heimann K (1999) Rescue effects of IPE transplants in RCS rats: short-term results. Invest Ophthalmol Vis Sci 40:1545–1556
Schraermeyer U, Kayatz P, Thumann G, Luther TT, Szurman P, Kociok N, Bartz-Schmidt KU (2000) Transplantation of iris pigment epithelium into the choroid slows down the degeneration of photoreceptors in the RCS rat. Graefes Arch Clin Exp Ophthalmol 238:979–984
Schraermeyer U, Thumann G, Luther T, Kociok N, Armhold S, Kruttwig K, Andressen C, Addicks K, Bartz-Schmidt KU (2001) Subretinally transplanted embryonic stem cells rescue photoreceptor cells from degeneration in the RCS rats. Cell Transplant 10:673–680
Smith LE (2004) Bone marrow-derived stem cells preserve cone vision in retinitis pigmentosa. J Clin Invest 114:755–757
Toda K, Bush RA, Humphries P, Sieving PA (1999) The electroretinogram of the rhodopsin knockout mouse. Vis Neurosci 16:391–398
Acknowledgements
We wish to thank J. Kozlowski, C. Hoffman and S. Basnaoglu for excellent technical assistance. This work was supported by the Pro Retina Stiftung.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was funded by “Pro Retina”.
Rights and permissions
About this article
Cite this article
Arnhold, S., Absenger, Y., Klein, H. et al. Transplantation of bone marrow-derived mesenchymal stem cells rescue photoreceptor cells in the dystrophic retina of the rhodopsin knockout mouse. Graefe's Arch Clin Exp Ophthalmol 245, 414–422 (2007). https://doi.org/10.1007/s00417-006-0382-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-006-0382-7