Abstract
Background
The purpose of this study was to investigate the combined use of perfluorohexyloctane (F6H8) and 1,000-centistoke silicone oil as a long-term intraocular tamponade in the treatment of complicated retinal detachment.
Methods
Sixty consecutive eyes affected by complicated retinal detachment with (1) retinal breaks of the lower two quadrants and severe proliferative vitreoretinopathy, (2) inferior giant retinal tear, (3) penetrating trauma or (4) choroidal detachment underwent pars plana vitrectomy using a combined internal tamponade of F6H8 and silicone oil. The double filling (DF) was removed after 40–50 days. The anatomical outcome and the complications due to the DF are reported.
Results
Retinal reattachment was achieved in all but one patient. Thirty-eight (63%) eyes needed further surgery with silicone oil tamponade. Silicone oil was successfully removed in 22 eyes. Sixteen (27%) eyes had retained silicone oil at the last follow-up examination. One eye showed persistent retinal detachment despite further surgery. Main complications of the DF were recurrent retinal detachment of the upper retina in six (10%) eyes and membrane formation in 25 (42%) eyes.
Conclusions
A combined internal tamponade of F6H8 and silicone oil may be a useful tool in the treatment of complicated retinal detachment involving the lower quadrants of the retina.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Retinal detachments with large lower retinal breaks and/or inferior proliferative vitreoretinopathy (PVR) are still a challenge to the surgeon. Up to now, silicone oil has been the most commonly used long-term vitreous substitute. It has a lower specific gravity than intraocular fluid and therefore provides a fairly good support to the upper retina; it is effective especially for superior breaks and detachments. However, an accumulation of fluid in the inferior quadrants, under the endotamponade bubble, may occur and can lead to reproliferation in the inferior retina [12]. In order to reduce inferior postoperative PVR pharmacological prevention [1], large inferior scleral buckling [14] and heavy liquid endotamponade [17] have been suggested.
The conventional perfluorocarbon liquids (i.e. perfluorodecalin, perfluoro-n-octane, perfluorotributylamine and perfluoroperhydrophenantrene) [18, 26] have a high specific gravity (ranging from 1.72 to 2.21 g/cm3) causing mechanical or toxic damage to the nerve fibre and the ganglion cell layer [2, 3, 6, 23, 24] as well as retinal pigment epithelium and photoreceptors [16]. Therefore they can be safely used only as a short-term endotamponade or as an intraoperative tool.
Recently a new class of compounds, semifluorinated alkanes (FALKs), has been available [13]. They show a lower specific density: the mostly used F6H8 has a density of 1.32 g/cm3. Its tolerance as a long-term internal tamponade has been demonstrated in experimental animals [27] and in humans [11, 21]. Kirchhof [11] has reported the use of F6H8 as a long-term endotamponade in complicated retinal detachment. It was tolerated without any obvious signs of damage to the retina or to the optic disk, with an average duration of 76 days. The most common complication (due to its low viscosity) has been early dispersion and emulsification of F6H8 into droplets, occurring after 3 days to 12 weeks, probably reducing the tamponading effectiveness. The formation of fine droplets may be the stimulus for the inflammatory response. Moreover, as reported by Hiscott [9], emulsification of F6H8 may favour the formation of epiretinal membranes.
In order to reduce emulsification of F6H8 and increase its viscosity, double-filling with silicone oil and F6H8 has been suggested [20].
Using a model eye chamber, Herbert [8] has demonstrated that silicone oil and F6H8 can join to form a united, two-layer bubble that reduces the tendency of F6H8 to disperse and changes the effectiveness of each tamponade agent on its own. The authors found that with the proper adjusting of the ratio of silicone oil and F6H8 it should be possible to optimise the tamponade effect. Wolf [25] has obtained a sufficient tamponade of inferior retinal tears using a silicone oil-RMN3 mixture (“heavy silicone oil”) with a relative density of 1.03 g/cm3.
Therefore, we have studied a mixture of silicone oil and F6H8 in vitro. At a temperature of 37°C, a ratio of 50% silicone oil and 50%, F6H8 form a homogeneous and stable mixture resulting in a density of 1.1 g/cm3 (Lepori, unpublished communication).
Since the tamponading force of the bubble depends not only on its size, shape and contact angle [26] but also on its density [19], we tried experimentally to increase the density of the double filling by increasing the F6H8 content. We found that at a volume ratio of 70% F6H8 and 30% silicone oil, the two substances form at equilibrium a biphasic solution with a lower layer of nearly pure F6H8 (density 1.33 g/cm3) and an upper solution of silicone oil and F6H8 (density 1.15 g/cm3) (Lepori, unpublished communication). We used this F6H8-silicone oil ratio as we considered it as the best compromise between tamponading effect and tendency to emulsification.
The aim of this paper is to evaluate the anatomic outcome and the complications which have occurred in eyes with severe retinal detachment using a combined intraocular tamponade with F6H8 and silicone oil.
Materials and methods
This study was an interventional case series of 64 consecutive eyes of 64 patients enrolled from May 2000 until August 2003. Four patients were excluded from the study because follow-up data was not available. The data of 60 patients is reported below.
Inclusion criteria
Patients affected by complicated retinal detachment in the study eye, visual acuity of 20/40 or better in the fellow eye, willingness to participate in the trial and attendance of all follow-up examinations. Complicated retinal detachment was diagnosed in eyes with (1) retinal breaks and severe proliferative vitreoretinopathy (≥C2 according to the Retina Society Classification [15]) of the lower two quadrants, (2) inferior giant retinal tears, (3) retinal detachment secondary to penetrating trauma or (4) retinal and choroidal detachment also involving the inferior retina.
After the experimental nature of the treatment was explained to the patients, informed consent was obtained. This study was approved by the local ethics committee.
Exclusion criteria
Age under 18 years, severe systemic disease, pregnancy, any uncontrolled ocular disease other than retinal detachment, participation in another study, missing informed consent.
Baseline examination
This consisted in a detailed ophthalmic history, best-corrected Snellen visual acuity, slit-lamp biomicroscopy, Goldman applanation tonometry, and direct and indirect ophthalmoscopy. The grade of PVR was defined according to the classification of the Retinal Society [15].
Follow-up examinations were scheduled one day, one week, one month, three months, six and 12 months after surgery and DF endotamponade.
Surgical technique
Surgery was performed in regional anesthesia. An encircling band (2.5 mm) was positioned, if not already present. A three-port pars plana vitrectomy was performed in all patients. Silicone oil, if present, was aspirated. The crystalline lens was removed in case of anterior PVR. The intraocular lenses (IOLs) were left in situ. Epiretinal membranes were peeled. The retina was flattened using Perfluorodecalin or Perfluoro-n-octane. Retinotomy was applied if necessary. Fluid-air exchange and endolaser photocoagulation were carried out. The vitreous cavity was then filled with a mixture of 70% F6H8 (Vitreous Substitute F6H8; Fluoron/Geuder, Heidelberg, Germany) and 30% 1,000-centistoke silicone oil.
The DF was removed after 40–50 days in regional anesthesia. Sclerotomies were applied as for pars plana vitrectomy, and an infusion cannula was positioned. Under endoillumination and microscopic visualisation a Teflon tip cannula was held over the optic disc and the DF aspirated using the active aspiration of the vitrectomy system. Finally several BSS-air exchanges were performed.
Main outcome
We investigated the efficacy and safety of the DF as internal tamponade. The primary study goal was to evaluate the anatomical and functional results: success was defined as complete retinal reattachment posterior to the encircling band. The secondary study goal was to record the rate of complications occurring due to the double filling. Best-corrected visual acuity is reported at entrance examination and at the last follow-up visit.
Results
Study population
We investigated 60 eyes of 60 patients (43 male, 17 female). The mean age was 62 years (range 18–80). Follow-up ranged from 3 to 34 months (mean 23 months). At entrance examination, 47 patients showed retinal detachment with retinal breaks of the lower two quadrants and severe proliferative vitreoretinopathy. Five eyes were affected by retinal detachment secondary to penetrating trauma, four eyes suffered from retinal detachment with inferior giant retinal tear, and four eyes presented a retinal and choroidal detachment (Table 1).
Forty-five (75%) patients were affected by recurrent retinal detachment: 36 patients had undergone one previous surgery, nine had received two or more previous surgeries. Previous surgeries consisted in scleral buckling (19 eyes), surgery for repair of penetrating trauma (three eyes) and vitrectomy (23 eyes: 14 with silicone oil, nine with gas) (Table 2). Fifteen patients had not been operated on before.
Preoperative best-corrected visual acuity (BCVA) ranged from light perception to 20/200 (Table 2). At entrance examination 24 eyes were phakic, 27 pseudophakic and nine aphakic.
Membrane peeling was performed in 54 cases, retinotomy was necessary in 11 cases, the crystalline lens was removed in 19 eyes. The DF was injected without complications. Intraoperative retinal reattachment was achieved in all cases.
One month follow-up
Anatomic outcome
In all eyes, one month after surgery the posterior pole was attached and the tamponade of the lower two retinal quadrants was very good. Complete retinal reattachment was achieved in 54 eyes, while in six eyes a recurrent retinal detachment of the upper retina, not involving the posterior pole, occurred.
Postoperative fundus examination showed a slight interface below the optic nerve, the retina was well visible (Fig. 1).
Complications due to the double filling (Table 3)
Table 3
In 58 patients no significant dispersion or emulsification was evident in the anterior and posterior segment on slit-lamp examination. In two eyes DF macro bubbles were detected in the anterior chamber, even if no corneal damage was evident (Fig. 2). Elevated intraocular pressure (IOP) of at least 30 mmHg occurred in two patients. One patient showed a persistent hypotony (IOP less than 5 mmHg) with the DF in situ. Five patients were still phakic and developed a posterior subcapsular opacity 20–40 days after surgery. Epiretinal membranes occurred in 22 eyes, subretinal in three. Six recurrences of the upper retina with the DF in situ were observed (as above mentioned).
DF removal
The DF was removed after 31–93 days (mean 44 days) in all patients in regional anesthesia. In all cases the bubble of the endotamponade was easily detectable and removed.
In 19 cases the retina was completely reattached: the DF was removed and exchanged with BSS.
In 11 eyes, retinal holes of the upper retina or epiretinal membranes in the superior sector were evident so membrane peeling and endolaser-fotocoagulation was performed; the DF was exchanged with air-gas mixture.
Thirty eyes required standard silicone oil for the following reasons: six eyes presented a recurrent retinal detachment of the upper retina, 11 eyes showed diffuse epiretinal membranes and were peeled, three eyes underwent a retinotomy for subretinal membranes, five eyes presented redetachment during DF removal, while five eyes had received several unsuccessful previous surgeries.
Three months follow-up
Anatomic outcome
Thirty-nine eyes were attached without any endotamponade, and 20 were attached with silicone oil filling. In one eye the retina remained completely detached despite further surgery using silicone oil.
Silicone oil was used for the following reasons:
-
Four out of the 19 eyes that underwent DF-BSS exchange, showed retinal redetachment 1–4 weeks after surgery. They underwent further surgery and received a new endotamponade with silicone oil.
-
Four out of the 11 eyes filled with air-gas mixture were found to be detached after the gas was absorbed and required surgery with silicone oil filling.
-
Thirteen out of 30 eyes that underwent DF-silicone oil exchange, retained silicone oil, while in the remaining 17 eyes it had been removed successfully by the 3 months visit.
Six months follow-up
Anatomic outcome (Table 2)
Complete reattachment was achieved in 59 eyes, 44 (73%) without any endotamponade. As above mentioned in one eye the retina remained detached despite further surgery. 16 (27%) eyes retained silicone oil at the 6 months follow-up examination.
Twelve months follow-up
Fifty-two patients completed the 12 months follow-up. Fifty-one (98%) eyes presented complete retinal reattachment, 40 (77%) without any tamponade. As already mentioned in one eye retinal reattachment could not be achieved because of severe reproliferation. Twelve (23%) eyes out of 52 still retained silicone oil tamponade: the removal is not planned at the moment, since these eyes had already undergone several unsuccessful previous surgeries for retinal detachment and needed a long-lasting silicone oil tamponade.
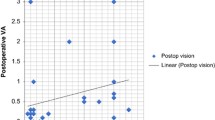
Functional outcome at last follow-up examination (Table 2)
Postoperative BCVA ranged from light perception to 20/25. BCVA improved in 46 (77%) eyes, decreased in two (3%) eyes and remained unchanged in 12 (20%) eyes. Twenty-nine (48%) patients had a visual acuity better than or equal to 20/400.
Discussion
Vitreoretinal surgery has been facilitated by substances used as intraoperative tools and internal tamponades. The ideal vitreous replacement substance should tamponade retinal holes in any location, fill the globe, displace the PVR stimulating environment in the inferior part of the vitreous cavity and be compatible with the ocular tissue. Silicone oil permits successful treatment of complicated retinal detachment with an anatomic success rate varying between 30 and 75% [4, 10]. However, many eyes with successful macular reattachment have residual retinal detachments [4], moreover PVR shows a prevalence in the inferior quadrants [7, 12]. Therefore various attempts have been made to develop a heavier-than-water substitute [11, 17, 22, 25].
To the best of our knowledge, no randomised clinical trial on the efficacy of the heavier-than-water endotamponade exists: various agents have been studied with anatomic success rates varying between 50% [5], 83% [11], 86% [21] 94% [25], and 100% [22], depending on the different period of follow-up, and on the definition of anatomic success. In fact, only Kirchhof considered retinal reattachment without any endotamponade a success [11].
The success rate in complicated retinal detachment with tears and PVR involving the inferior retina ranges from 50% [5] and 78% [11]. In our series, in 15 (25%) eyes the retina was completely reattached 3 months after DF removal. Fifty-five (75%) eyes required further surgery or exchange of the DF with long-acting gas or silicone oil. At the 12-months follow-up, complete retinal attachment without any endotamponade was achieved in 77% and in 98% with silicone oil.
Our study shows that the double filling consisting in F6H8 70% and silicone oil 30% can tamponade well the inferior parts of the retina.
At the 1-month examination, macula attachment was achieved in all cases, but six recurrences of the upper retina were seen (10%) in our study. The tamponading efficacy on the upper sector in orthostatic position was probably insufficient or membrane peeling had been incompletely carried out. In comparison, Wolf [25] observed residual retinal detachments in the superior quadrants in 18% using a “heavy silicone oil” with a density of 1.03 g/cm3. The relatively high rate of redetachment may be related to the selection of the patients: in fact a high percentage (43%) of patients had undergone previous unsuccessful vitreoretinal surgeries that represent a well-known risk factor for recurrent detachment [10].
The results of our pilot study show good intraocular tolerance of the DF as a long-term endotamponade; in our experience, complications using the DF are few and relatively easily dealt with.
We did not observe clinically any obvious emulsification or dispersion in the anterior and posterior segment in 97% of the cases. Macro bubbles of the DF were detected in the anterior chamber in two patients (3%), but no corneal damage was observed. Kirchhof reported, in his series, dispersion of F6H8 in 48% [11]. Sparrow mixed liquid perfluorocarbons with silicone oil in order to reduce the emulsification rate [20]: therefore, we could assume that silicone oil had reduced the tendency of F6H8 to emulsificate or to disperse. Postoperative elevated intraocular pressure was successfully treated with medical therapy and pupillary block did not occur, even though we had not performed an iridectomy.
Hypotony, due to a ciliary body detachment, was evident in one patient and spontaneously recovered after 1 month. IOP control was maintained after removal of the DF.
With the DF in situ epiretinal membranes occurred in 22 eyes (37%) and subretinal membranes in three eyes (5%). These eyes were preoperatively affected by severe PVR; therefore, it was difficult to understand whether these proliferations were PVR membranes or a biological reaction due to the endotamponade. The rate of epiretinal or subretinal membrane formation due to heavier-than-water endotamponades is variable: De Molfetta found postoperative proliferation in 90% [5], Kirchhof reported macular pucker formation in 9% [11]. Sparrow experimentally did not find any evidence that silicone oil and perfluorocarbon liquids differ in stimulation cellular proliferation and membrane formation [20].
We emphasise that only patients with severe retinal detachments were included, and 29 (48%) patients achieved a visual acuity better than or equal to 20/400.
Our study is limited by the lack of a control group; therefore no definite conclusions concerning the advantages of DF in respect to other endotamponades are possible; a prospective randomised controlled trial comparing other endotamponades with DF for complicated retinal detachment with involvement of the inferior quadrants will be the next step to investigating the effectiveness of the DF.
References
Asaria RH, Kon CH, Bunce C, Charteris DG, Wong D, Khaw PT, Aylward GW (2001) Adjuvant 5-fluorouracil and heparin prevents proliferative vitreoretinopathy: results from a randomized, double-blind controlled clinical trial. Ophthalmology 108:1179–1183
Chang S, Zimmermann NJ, Iwamoto T, Ortiz R, Faris D (1987) Experimental vitreous replacement with perfluorotributylamine. Am J Ophthalmol 103:29–37
Chang S, Sparrow JR, Iwamoto T, Gershbein A, Ross R, Ortiz R (1991) Experimental studies of tolerance to intravitreal perfluoro-n-octane liquid. Retina 11:367–374
Cox MS, Trese MT, Murphy PL (1986) Silicone oil for advanced proliferative vitreoretinopathy. Ophthalmol 93:646–650
De Molfetta V, Bottoni F, Arpa P, Vinciguerra P, Zenoni S (1992) The effect of simultaneous internal tamponade on fluid compartimentalization and its relationship to cell proliferation. Retina 12:S40–S45
Eckart C, Nicolai U, Winter M, Knop E (1991) Experimental intraocular tolerance to liquid perfluorooctane and perfluoropolyether. Retina 11:375–384
Fleury J, Bonnet M (1992) Prognostic value of new retinal tears associated with the development of postoperative proliferative vitreoretinopathy. Graefes Arch Clin Exp Ophthalmol 230:459–462
Herbert E, Stappler T, Wetterqvist C, Williams R, Wong D (2004) Tamponade properties of double-filling with perfluorohexyloctane and silicone oil in a model eye chamber. Graefes Arch Clin Exp Ophthalmol 242:692–696
Hiscott P, Magee RM, Colthurst M, Lois N, Wong D (2001) Clinicopathological correlation of epiretinal membranes and posterior lens opacification following perfluorohexyloctane tamponade. Br J Ophthalmol 85:179–183
Jonas JB, Knorr HLJ, Rank RM, Budde WM (2001) Retinal detachment after removal of intraocular silicone oil tamponade. Br J Ophthalmol 85:1203–1207
Kirchhof B, Wong D, Van Meurs J, Hilgers RD, Macek M, Lois N, Schrage NF (2002) Use of perfluorohexyloctane as a long-term internal tamponade agent in complicated retinal detachment surgery. Am J Ophthalmol 133:95–101
Mandai M, Takanashi T, Ogura Y, Honda Y (1990) Proliferative vitreoretinopathy shows predilection for the inferior fundus. Graefes Arch Clin Exp Ophthalmol 228:335–337
Meinert H, Roy T (2000) Semifluorinated alkanes—a new class of compounds with outstanding properties for use in ophthalmology. Eur J Ophthalmol 10:189–197
Michels RG (1984) Surgery of retinal detachment with proliferative vitreoretinopathy. Retina 4:63–83
No authors listed (1983) The classification of retinal detachment with proliferative vitreoretinopathy. Ophthalmology 90:121–125
Orzalesi N, Migliavacca L, Bottoni F, Miglior S (1998) Experimental short-term tolerance to perfluorodecalin in the rabbit eye: a histological study. Curr Eye Res 17:828–835
Peyman GA, Conway MD, Soike KF, Clark LC Jr (1991) Long-term vitreous replacement in the primates with intravitreal Vitreon or Vitreon plus silicone. Ophthalmic Surg 22:657–664
Peyman GA, Schulman JA, Sullivan B (1995) Perfluorocarbon liquids in ophthalmology. Surv Ophthalmol 39:375–395
Parel JM (1992) Olii di silicone: proprietà fisicochimiche. In: Ryan SJ (ed) Retina, vol. 3 (Italian edition). Medical Books, Palermo, pp 271–289
Sparrow JR, Jayakumar A, Berrocal M, Ozmert E, Chang S (1992) Experimental studies of the combined use of vitreous substitutes of high and low specific gravity. Retina 12:134–140
Stefaniotou MI, Aspiotis MV, Kitsos GD, Kalogeropoulos CD, Asproudis IC, Psila KG (2002) Our experience with perfluorohexyloctane (F6H8) as a temporary endotamponade in vitreoretinal surgery. Eur J Ophthalmol 12:518–522
Tanji TM, Peyman GA, Mehta NJ, Millsap CM (1993) Perfluoroperhydrophenanthrene (Vitreon) as a short-term vitreous substitute after complex vitreoretinal surgery. Ophthalmic Surg 24:681–685
Velikay M, Wedrich A, Stolba U, Datlinger P, Li Y, Binder S (1993) Experimental long-term vitreous replacement with purified and nonpurified perfluorodecalin. Am J Ophthalmol 116:565–570
Velikay M, Stolba U, Wedrich A, Li Y, Datlinger P, Binder S (1995) The effect of chemical stability and purification of perfluorocarbon liquids in experimental extended-term vitreous substitution. Graefes Arch Clin Exp Ophthalmol 233:26–30
Wolf S, Schön V, Meier P, Wiedemann P (2003) Silicone oil-RMN3 mixture (“heavy silicone oil”) as internal tamponade for complicated retinal detachment. Retina 23:335–342
Wong D, Lois N (2000) Perfluorocarbons and semifluorinated alkanes. Semin Ophthalmol 15:25–35
Zeana D, Becker J, Kuckelkorn R, Kirchhof B (1999) Perfluorohexyloctane as a long-term vitreous tamponade in the experimental animal. Experimental perfluorohexyloctane substitution. Int Ophthalmol 23:17–24
Acknowledgement
We thank Dott. Luciano Lepori, Dr. of physical chemistry, CNR (National Council of Research), Pisa, Italy, for his collaboration regarding the in vitro study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rizzo, S., Genovesi-Ebert, F. & Belting, C. The combined use of perfluorohexyloctane (F6H8) and silicone oil as an intraocular tamponade in the treatment of severe retinal detachment. Graefe's Arch Clin Exp Ophthalmo 244, 709–716 (2006). https://doi.org/10.1007/s00417-006-0317-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-006-0317-3