Abstract
Purpose
To report a case of toxoplasmosis with optic nerve and orbital involvement as the initial presentation of HIV infection.
Method
Case report.
Results
A 46-year-old zookeeper, who had had right central retinal vein occlusion (CRVO) 2 weeks previously, presented with painless lid and conjunctival swelling and profound visual loss in his right eye (RE). Examination revealed no light perception (NLP) RE with axial proptosis and ocular motility restriction; fundal examination revealed a clinical picture of an ischaemic CRVO. MRI of the brain and orbit showed ring-enhancing targetoid lesions in the brain and inflammatory changes in the right optic nerve, extraocular muscles and orbital fat. He was subsequently found to be HIV positive and had positive toxoplasma IgG serology.
Conclusions
Immunocompromised individuals have an increased likelihood for more severe and atypical presentations; this highlights the need for increased index of suspicion for HIV infection as ocular or orbital disease may be the first manifestation of life-threatening systemic toxoplasmosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Toxoplasma gondii occurs as the initial systemic opportunistic infection in 10–38% of HIV-infected individuals [3]. However, to date, there have been few reports of ocular toxoplasmosis as the initial manifestation of HIV infection [2, 6] and even fewer with concomitant orbital involvement [4, 5]. Herein, we report a patient who presented with orbital inflammation and optic nerve involvement due to toxoplasmosis as the initial manifestation of undiagnosed HIV.
Case report
A 46-year-old zookeeper presented with a 1-day history of painless, progressive lid and conjunctival swelling and loss of vision in his right eye (RE). He was hypertensive and had been diagnosed with a right central retinal vein occlusion (CRVO) 2 weeks previously. His vision loss at that time was less profound.
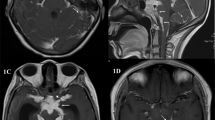
Examination revealed no light perception (NLP) RE with a relative afferent pupillary defect, axial proptosis, chemosis (Fig. 1a), ocular motility restriction and retrolental cells 1+ in the right eye. Intraocular pressure was normal. Fundal examination showed disc swelling, cotton wool spots, macular oedema and extensive flame-shaped haemorrhages (Fig. 1b).
MRI of the brain and orbit showed multiple ring-enhancing targetoid lesions in the cerebellar, occipital and frontal lobes and enhancement of the right optic nerve, extraocular muscles and orbital fat (Fig. 2). He was found to be HIV positive with a CD4 count of 11 cells/mm3 and had positive toxoplasma IgG serology (titre>1/1,024). Polymerase chain reaction performed on his vitreous sample was positive for toxoplasma. Subsequent blood investigations also revealed protein S deficiency. Chest X-ray was clear and his mantoux test was negative.
Treatment with pyrimethamine, sulphadiazine and folinic acid was commenced and maintained for 12 weeks. He was given concomitant pulsed intravenous methylprednisolone 1 g daily for 3 days. The proptosis, chemosis and ocular motility restriction resolved rapidly within 6 days. At 4 months follow-up, his eye was quiet but acuity remained at NLP. He remained systemically well and had been started on systemic anti-retroviral therapy.
Discussion
The fundal appearance revealed a likely ischaemic vascular event with no chorioretinal scars or active retinochoroiditis or vitritis to suggest toxoplasmosis infection. There was also rapid onset of proptosis, chemosis and extraocular motility restriction mimicking an acute orbital inflammation or infection. The MRI findings of the brain showed multiple ring-enhancing targetoid lesions in the cerebellar, occipital and frontal lobes, which suggested the possibility of toxoplasmosis infection in an immunocompromised individual.
Toxoplasmosis is the most common cause of a focal brain lesion in patients with AIDS. The characteristic sign of cerebral toxoplasmosis is the asymmetric ‘target’ sign. It represents multiple ring-enhancing abscesses with eccentric nodules within the abscess cavity thus giving the appearance of a ‘target’. This is highly suggestive of cerebral toxoplasmosis and, if present, should alert the clinician to the possibility of HIV infection. The other infection that may give a similar appearance is tuberculosis.
It is recognised that HIV-infected patients may have an associated protein S deficiency [1]. In our patient, this could have led to thromboembolic episodes involving the central retinal vein or artery, or even the ciliary arteries supplying the optic nerve and subsequently causing optic-nerve infarction. Opportunistic infection by toxoplasma could have also directly infiltrated the retrobulbar optic nerve and optic nerve head causing the infarction of the optic nerve and reactive orbital inflammation. The opportunistic toxoplasma infection and severe orbital inflammation could have caused an increase in intraorbital pressure and subsequent occlusion of the central retinal vessels and blood supply to the optic nerve.
To our knowledge, this the first reported case of toxoplasmosis with optic nerve and orbital involvement as the initial presentation of HIV infection. Immunocompromised individuals such as our patient have an increased likelihood for more severe and atypical presentations; this highlights the need for increased index of suspicion for HIV infection as ocular or orbital disease may be the first manifestation of life-threatening systemic toxoplasmosis.
References
Erbe M, Rickerts V, Bauersachs RM, Lindhoff-Last E (2003) Acquired protein C and protein S deficiency in HIV-infected patients. Clin Appl Thromb Hemos 9(4):325–331, Oct
Falcone PM, Notis C, Merhige K (1993) Toxoplasmic papillitis as the initial manifestation of acquired immune deficiency syndrome. Ann Ophthalmol 25(2):56–57
Gellin BG, Soave R (1992) Coccidian infections in AIDS. Med Clin North Am 76:205–228
Kronish JW, Johnson TE, Gilberg SM et al (1996) Orbital infections in patients with human immunodeficiency virus infection. Ophthalmology 103(9):1483–1492
Moorthy RS, Smith RE, Rao NA (1993) Progressive ocular toxoplasmosis in patients with acquired immunodeficiency syndrome. Am J Ophthalmol 115(6):742–747
Wei ME, Campbell SH, Taylor C (1996) Precipitous visual loss secondary to optic nerve toxoplasmosis as an unusual presentation of AIDS. Aust NZ J Ophthalmol 24(1):75–77
Author information
Authors and Affiliations
Corresponding author
Additional information
No financial support was received for this paper. The authors have no proprietary interests in the drugs and equipment used in this paper.
Rights and permissions
About this article
Cite this article
Lee, MW., Fong, KS., Hsu, LY. et al. Optic nerve toxoplasmosis and orbital inflammation as initial presentation of AIDS. Graefe's Arch Clin Exp Ophthalmo 244, 1542–1544 (2006). https://doi.org/10.1007/s00417-006-0295-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-006-0295-5