Abstract
Purpose
To study intravitreal dexamethasone and vancomycin concentrations, when used together in patients with suspected postoperative bacterial endophthalmitis. Animal studies had suggested that dexamethasone might decrease the concentration of vancomycin.
Design
Prospective randomized clinical trial in a tertiary referral center.
Methods
Twenty-nine consecutive patients with suspected postoperative bacterial endophthalmitis underwent a vitreous biopsy followed by intravitreal injection of antibiotics (0.2 mg vancomycin, 0.05 mg gentamicin) and 400 μg dexamethasone or placebo. After 3–4 days, the intravitreal injection of antibiotics and dexamethasone or placebo was repeated. In 18 patients, a second biopsy was taken for repeat culture and measurement of vancomycin and dexamethasone concentrations.
Results
In 20/29 patients (69%) the first vitreous cultures were positive; the second culture was negative in all cases. Thirteen out of 29 patients received dexamethasone. Dexamethasone concentrations showed an average of 25 ng/ml 3 days after injection, with an estimated half-life of 5.5 h. Vancomycin concentrations in patients given dexamethasone tended to be higher compared with those in the placebo group (P=0.061).
Conclusion
Intravitreal dexamethasone does not lead to decreased vancomycin concentrations, when given simultaneously in the treatment of patients with suspected bacterial endophthalmitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postoperative bacterial endophthalmitis is a sight-threatening complication of intraocular surgery. The infecting bacteria, by replication and release of toxins, and the inflammatory response of the host contribute to the damage inflicted to the ocular structures [1]. In the treatment of bacterial meningitis, corticosteroids are of proven use, in addition to antibiotics, in reducing morbidity and mortality [3] presumably by limiting the recruitment of leucocytes, by stabilizing the blood-brain barrier (which is very similar in nature to the blood-retina barrier) and by producing cytoprotectants. Also in ophthalmology, corticosteroids have a beneficial effect on the outcome of endophthalmitis in most animal studies ([5], [7]). However, two studies ([8, [10]]) reported that dexamethasone may decrease the vancomycin concentrations, a possible concern for their combined use.
Because the results of the only two controlled trials on the potential benefit of dexamethasone as adjuvant to antibiotic treatment on the outcome of patients with suspected bacterial endophthalmitis were contradictory ([[2], 9]), we had started a placebo-controlled trial, in the course of which we obtained data on the vitreous concentrations of the injected antibiotics and dexamethasone. Unfortunately, the trial had to be stopped prematurely, because one of the study medications was no longer available. The data on vitreous concentrations of dexamethasone and vancomycin remain of interest, however, and form the subject of this communication.
Materials and methods
Starting from April 1999 consecutive patients with a diagnosis of suspected bacterial post-cataract endophthalmitis presenting at the Rotterdam Eye Hospital were asked to participate in this study. The study protocol was approved by the Institutional Review Board. The patients were randomized to either intravitreal dexamethasone or placebo as adjunct to standard antibiotic treatment.
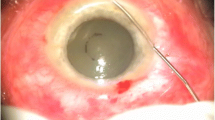
Our treatment approach has been described previously [4]. In short, a vitreous biopsy with a vitrectome was taken in patients with a vision of hand movement or better, whereas a limited core vitrectomy with an anterior chamber infusion was performed in patients with light perception only. Undiluted vitreous was collected for Gram-staining and culture before the start of empiric antibiotic therapy; the vitreous was plated within 2 h and cultured aerobically and anaerobically. Immediately after the vitreous biopsy was taken, patients received an intravitreal injection of 0.2 mg vancomycin in 0.1 ml phosphate-buffered saline and 0.05 mg gentamicin in 0.1 ml phosphate-buffered saline, as well as 400 μg dexamethasone sodium diphosphate (Decadron 20 mg/ml with 1 mg/ml paraben as preservative, resulting in 0.025 mg paraben in 0.1 ml) or placebo in 0.1 ml phosphate buffered saline.
The intravitreal injection of 0.2 mg vancomycin was repeated once after 3 or 4 days.
In the first 18 patients, the second injection was preceded by a vitreous biopsy using a vitrectome, to obtain a repeat bacterial culture and, if there was sufficient material left, for measurements of the intravitreal vancomycin, gentamicin and/or dexamethasone concentration. Vitreous levels of vancomycin were determined by fluorescence polarization immunoassay (AxSYM, Abbott Laboratories, Abbott Park, Ill., USA). Dexamethasone concentrations were measured with a radioimmunoassay, using antibody against dexamethasone (IgG Corporation, Nashville, Tenn., USA). Vancomycin and dexamethasone concentrations were each measured in a different laboratory, each without the possibility to measure both substances.
The primary outcome measure was Snellen visual acuity at 3 and 12 months. The difference between the dexamethasone and placebo group in vision at 3 and 12 months follow-up was tested for statistical significance with the Mann-Whitney test. Differences in vancomycin concentrations between patients treated with placebo or dexamethasone were tested for statistical significance with the Fisher exact test.
Results
Enrollment of patients
Twenty-nine patients were enrolled; in mid-June 2000 the study had to be terminated prematurely because the study drug, i.e. dexamethasone sodium diphosphate (Decadron of 20 mg/ml) was no longer available. Thirteen patients received dexamethasone, 16 patients received placebo.
Patient characteristics
The interval between cataract surgery and the first signs of endophthalmitis, presenting vision and the interval first injection of antibiotics and dexamethasone or placebo and second biopsy were similar in the two groups. (Table 1).
Microbiological findings
Before the start of treatment, 29 vitreous biopsies were obtained in 29 patients, of which 20 (69%) showed growth of micro-organisms. The relative number of positive cultures (i.e. 70%) did not differ between the placebo and dexamethasone group. Coagulase negative staphylococci (mostly Staphylococcus epidermidis) were most commonly isolated (n=15, Table 1). In this series, no Gram-negative micro-organisms were cultured.
Second biopsy
In 18 patients, a second vitreous biopsy was performed. In none of these biopsies was growth of micro-organisms observed, despite positive microbiological findings in 12 of them at first culture.
Vitreous concentrations of antibiotics
From these 18 patients, second biopsy intravitreal vancomycin concentrations were also measured in 12. In six patients, only dexamethasone concentrations were measured.
The vancomycin concentrations in seven patients in the dexamethasone group ranged from 6.8 to 16.6 μg/ml (mean 11.4, median 12), whereas those in five patients in the placebo group ranged from 2.6 to 10.8 μg/ml (mean 6.7, median 6.3). This difference in concentration just failed to reach statistical significance (Mann-Whitney test P=0.061). The interval between first drug injection and second biopsy was very similar in both groups: in the patients given dexamethasone a median of 73 (62–93) h, and a median of 71 (66–72) h in those given placebo.
Vitreous concentrations of dexamethasone
In 7 patients given dexamethasone, the vitreous concentration of this drug could be measured, and varied from 13.9 to 392 ng/ml (mean 67.4 ng/ml, median 69.0 ng/ml) at 60–73 h (median 69 h) after injection. Assuming an initial vitreous concentration of maximum 100 μg/ml dexamethasone (dose: 400 μg, distribution volume of the vitreous cavity: 4 ml), the estimated half-life of dexamethasone would amount to 5.5 h.
Follow-up and recovery of vision
On non-parametric analysis, there was a trend towards a better visual outcome at 3 months (P=0.055) and at 12 months (P=0.080) in patients treated with dexamethasone.
Discussion
The main findings of this aborted randomized trial was that in patients who presented with suspected postoperative bacterial endophthalmitis, the intravitreal administration of dexamethasone, together with antibiotics, may improve the visual outcome at 3 and 12 months after the acute episode and that dexamethasone did not affect the pharmacokinetics of vancomycin administered intravitreally, nor did it result in a delay in microbiological clearance.
A major limitation of the clinical study, however, was its small sample size. Because the study dexamethasone (Decadron 20 mg/ml) was withdrawn from the market by the manufacturer and the remaining commercially available formula (Decadron 5 mg/ml) contained 4 times as much of the preservative paraben (a concentration shown only just safe in rabbit eyes [6]), the study was stopped after enrolment of 29 patients.
Our treatment with a low but adequate dose of vancomycin (0.2 mg, instead of the usual dose of 1 mg) and gentamicin (0.05 mg, half the lowest dose ever reported to cause macular infarction: 0.1 mg) resulted in antibiotic concentrations well above minimal inhibitory concentration for most micro-organisms for well over a week, while minimizing potential retinotoxic effects [4].
In experiments on rabbits with Staphylococcus epidermidis endophthalmitis, it was found that vancomycin concentrations were somewhat lower in animals given dexamethasone simultaneously. This somewhat increased vancomycin clearance did not interfere with the effectiveness of this drug in healing the endophthalmitis, very likely because of vancomycin’s pharmacodynamic characteristic, i.e. a full antimicrobial effect above a certain critical concentration. Park reported a similar finding in rabbits with uninfected eyes but not in eyes with severe Streptococcus pneumoniae endophthalmitis, in which an increase in half-life of vancomycin was observed. As vancomycin is cleared from the vitreous by bulk flow through the trabecular meshwork (a process speculated to be facilitated by dexamethasone), an explanation may be that this effect was counterbalanced in streptococcal endophthalmitis, which excites a severe inflammatory response, cell influx and some blockage of the trabecular meshwork. Moreover, by reducing blood-ocular barrier breakdown, dexamethasone may decrease the abnormal elimination through the broken-down blood-ocular barriers during severe inflammation. In our small study, there was a trend (P=0.061) for the concentration of vancomycin to be higher in patients given dexamethasone, rather lending support for a vancomycin concentration increasing effect of dexamethasone.
In conclusion, intravitreal dexamethasone does not lead to decreased vancomycin concentrations, when given simultaneously in the treatment of patients with suspected bacterial endophthalmitis. We have now started a new, larger, multicenter trial to study the role of preservative-free dexamethasone as an adjuvant to antibiotics.
References
Callegan MC, Engelbert M, Parke DW, Jett BD, Gilmore MS (2002) Bacterial endophthalmitis: epidemiology, therapeutics, and bacterium-host interactions. Clin Microbiol Rev 15(1):111–124
Das T, Jalali S, Gothwal VK, Sharma S, Naduvilath TJ (1999) Intravitreal dexamethasone in exogenous bacterial endophthalmitis: results of a prospective randomised study. Br J Ophthalmol 83(9):1050–1055
de Gans J, van de Beek D (2002) Dexamethasone in adults with bacterial meningitis. N Engl J Med 347(20):1549–1556
Gan IM, van Dissel JT, Beekhuis WH, Swart W, Van Meurs JC (2001) Intravitreal vancomycin and gentamicin concentrations in patients with postoperative endophthalmitis. Br J Ophthalmol 85(11):1289–1293
Jett BD, Jensen HG, Atkuri RV, Gilmore MS (1995) Evaluation of therapeutic measures for treating endophthalmitis caused by isogenic toxin-producing and toxin-nonproducing Enterococcus faecalis strains. Invest Ophthalmol Vis Sci 36(1):9–15
Kwak HW, D’Amico DJ (1992) Evaluation of the retinal toxicity and pharmacokinetics of dexamethasone after intravitreal injection. Arch Ophthalmol 110(2):259–266
Meredith TA, Aguilar HE, Drews C, Sawant A, Gardner S, Wilson LA, Grossniklaus HE (1996) Intraocular dexamethasone produces a harmful effect on treatment of experimental Staphylococcus aureus endophthalmitis. Trans Am Ophthalmol Soc 94:241–252
Park SS, Vallar RV, Hong CH, von Gunten S, Ruoff K, D’Amico DJ (1999) Intravitreal dexamethasone effect on intravitreal vancomycin elimination in endophthalmitis. Arch Ophthalmol 117(8):1058–1062
Shah GK, Stein JD, Sharma S, Sivalingam A, Benson WE, Regillo CD, Brown GC, Tasman W (2000) Visual outcomes following the use of intravitreal steroids in the treatment of postoperative endophthalmitis. Ophthalmology 107(3):486–489
Smith MA, Sorenson JA, Smith C, Miller M, Borenstein M (1991) Effects of intravitreal dexamethasone on concentration of intravitreal vancomycin in experimental methicillin-resistant Staphylococcus epidermidis endophthalmitis. Antimicrob Agents Chemother 35(7):1298–1302
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gan, I.M., Ugahary, L.C., van Dissel, J.T. et al. Effect of intravitreal dexamethasone on vitreous vancomycin concentrations in patients with suspected postoperative bacterial endophthalmitis. Graefe's Arch Clin Exp Ophthalmo 243, 1186–1189 (2005). https://doi.org/10.1007/s00417-005-1182-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-005-1182-1