Abstract
Background
Placenta growth factor (PlGF) is an important co-factor in retinal neovascularization. To examine whether retinal pigment epithelial (RPE) cells may represent a source for PlGF during retinopathy, we determined whether human RPE cells in vitro produce and respond to PlGF. In addition, we determined whether the cells express receptors for PlGF, i.e. flt-1 and neuropilins.
Methods
Cultured human RPE cells of passages 3–5 were used. The regulation of the PlGF gene and protein expression by growth factors and cytokines was evaluated by quantitative PCR and ELISA. Proliferation rates and chemotaxis were determined by a bromodeoxyuridine and a Boyden chamber assay.
Results
Human RPE cells express mRNAs for various members of the vascular endothelial growth factor family and for their receptors, including mRNAs for PlGF, flt-1, KDR, and neuropilins-1 and -2. The expression levels of the mRNAs for neuropilins-1 and -2 were significantly higher than those for flt-1 and KDR. Members of the transforming growth factor (TGF)-β superfamily of growth factors (BMP-4, TGF-β1, and β2) were strong inducers of PlGF gene expression, and evoked secretion of PlGF-2 protein by RPE cells. Exogenous PlGF-2 induced chemotaxis in RPE cells and reduced slightly the cell proliferation at high concentrations.
Conclusion
The findings that RPE cells produce and respond to PlGF indicate that the factor exerts an autocrine/paracrine action on these cells. It is suggested that increased expression of TGF-β-related growth factors during diabetic retinopathy may cause PlGF secretion by RPE cells contributing to the stimulation of cell migration as a critical component of the progression of fibrovascular membranes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pathological angiogenesis is a serious consequence of important eye diseases such as diabetic retinopathy and age-related macular degeneration. Though the vascular endothelial growth factor (VEGF) and its receptors (VEGF-Rs) have been critically implicated in mediating pathological neovascularization [10, 20, 27], it became evident that the synergistic action of other proangiogenic factors and of their receptors is required for the angiogenic effect of VEGF [6]. One of the receptors expressed in fibrovascular tissues and in choroidal neovascular membranes is neuropilin-1 [7], and it has been found that the expression level of neuropilin-1 correlates with the degree of neovascularization [16]. Neuropilin-1 is a cell-surface receptor for different ligands: it is an isoform-specific receptor for VEGF-A165 [34], a receptor for the heparin-binding form of the placenta growth factor (PlGF), PlGF-2 [19, 23, 24], and a receptor for semaphorin-3A which is a member of the collapsin-semaphorin family of proteins functionally involved in axon guidance and cell migration [12, 38]. Neuropilin-1 acts as a co-receptor that enhances the binding affinity of VEGF to VEGF-R2 (KDR/flk-1) [11, 35], and therefore increases the bioactivity (proliferation and migration) of VEGF in endothelial cells [25, 34].
PlGF is a member of the VEGF family of growth factors and has at least three isoforms generated by alternative splicing of RNA, PlGF-1 (PlGF149), PlGF-2 (PlGF170), and PlGF-3 (PlGF221) [4, 18]. There is evidence that PlGF is implicated in the formation of fibrovascular tissue during proliferative diabetic retinopathy: the vitreous level of PlGF is elevated during the development of proliferative diabetic retinopathy [17, 21]; PlGF immunoreactivity is expressed in fibrovascular membranes (but not in non-vascularized epiretinal membranes or in normal retinas) [17]; and the retinal expression of PlGF mRNA is increased during diabetic retinopathy [36]. Moreover, deficient expression of PlGF has been shown to prevent the development of experimental choroidal neovascularization [30]. PlGF facilitates endothelial cell proliferation and vascular permeability by potentiating the activity of VEGF [1, 8, 26], and the presence of PlGF is required for the angiogenic effect of VEGF in the ischemic retina [5]. One major source of VEGF in the retina is the retinal pigment epithelium (RPE) [3]. However, it is not known whether RPE cells produce (in addition to VEGF) also PlGF. Therefore, we investigated the production and secretion of PlGF by human RPE cells in vitro. We determined the expression of mRNA for different members of the VEGF protein family and for the receptors of PlGF and VEGF, flt-1, KDR, and neuropilins-1 and -2, and investigated the regulation of mRNA expression by various growth factors and cytokines. Additionally, we determined whether RPE cells secrete and respond to PlGF protein. The results suggest that RPE cells may represent one major source for PlGF during retinopathy.
Materials and methods
Materials
The recombinant growth factors and cytokines transforming growth factor-β1 (TGF-β1), TGF-β2, bone morphogenetic protein-4 (BMP-4), VEGF-A165, platelet-derived growth factor-BB (PDGF-BB), heparin-binding epidermal growth factor-like growth factor (HB-EGF), basic fibroblast growth factor (bFGF), hepatocyte growth factor (HGF), and tumor necrosis factor-α (TNFα) were purchased from R&D Systems (Wiesbaden, Germany). PlGF-2 and interleukin-1β (IL-1β), were obtained from RELIATech (Braunschweig, Germany). The following antibodies were used: a rabbit anti-human p44/p42 mitogen-activated protein kinase (MAPK) (New England Biolabs, Frankfurt/M., Germany; 1:1000), a rabbit anti-phosphorylated p44/p42 MAPK (New England Biolabs; 1:1000), a rabbit anti-human Akt (New England Biolabs; 1:1000), a rabbit anti-human phosphorylated Akt (New England Biolabs; 1:1000), a rabbit anti-human p38 MAPK (New England Biolabs; 1:1000), a rabbit anti-human phosphorylated p38 MAPK (New England Biolabs; 1:750) and an anti-rabbit IgG conjugated with alkaline phosphatase (Chemicon, Hofheim, Germany; 1:2000).
Cell culture
Human RPE cells were obtained from several donors within 48 h of death, and were prepared as described previously [9]. The use of human material was approved by the ethics committee of the University of Leipzig Medical Faculty, and was performed according to the Declaration of Helsinki. The cells were suspended in Ham F-10 medium containing 10% fetal bovine serum, glutamax II, and gentamycin, and were cultured in tissue culture flasks (Greiner, Nürtingen, Germany) in 95% air/5 % CO2 at 37°C. Cells of passages 3–5 were used. The epithelial nature of the RPE cells was identified routinely by immunocytochemistry using the monoclonal antibodies AE1 (which recognizes most of the acidic type I keratins) and AE3 (which recognizes most of the basic type II keratins) (Chemicon, Hampshire, U.K.). All tissue culture components and solutions were purchased from Gibco BRL (Paisley, UK).
DNA synthesis rate
The cells were seeded at 3×103 cells per well in 96-well microtiter plates (Greiner), and were allowed to attach for 48 h. Thereafter, the cells were growth arrested in medium without serum for 5 h, and subsequently, medium containing 0.5% serum with and without test substances was added for another 24 h. The incorporation of bromodeoxyuridine (BrdU) into the genomic DNA was measured by using the Cell Proliferation ELISA BrdU Kit (Roche, Mannheim, Germany) according to the manufacturer’s instructions. BrdU (10 μM) was added to the culture medium 5 h before fixation. To compare possible effects of the factors tested with the action of a known mitogen for RPE cells, and to reveal possible modulating effects on growth factor-evoked proliferation, PDGF was used as positive control.
Chemotaxis
Measurement of chemotaxis was performed by using a modified Boyden chamber assay. Suspensions of RPE cells (100 μl; 5×105 cells/ml serum-free medium) were seeded onto polyethylene terephthalate filters (pore size 8 μm; Becton Dickinson, Heidelberg, Germany) coated with fibronectin (50 μg/ml) and gelatin (0.5 mg/ml). Within 4 h after seeding, the cells attached to the filter and formed a semiconfluent monolayer. Thereafter, the medium was changed into medium without addivitves in the upper well and medium containing PlGF-2 or VEGF-A165 in the lower well. After incubation for 16 h, the inserts were washed with buffered saline, fixed with Karnofsky`s reagent, and stained with hematoxylin. Non-migrated cells were removed from the filters by gentle scrubbing with a cotton swab. The migrated cells were counted, and the results were expressed relative to the cell migration rate in the absence of test substances.
Western blotting
The cells were seeded at 5×105 cells per well in six-well plates in 1.5 ml serum-containing medium, and were allowed to grow up to a confluency of 80%. After growth arrest for 16 hours, the cells were pre-treated with blocking substances for 30 min and thereafter with test substances for 10 min. Then, the medium was removed, the cells were washed twice with prechilled phosphate-buffered saline (pH 7.4; Invitrogen, Paisley, UK), and the monolayer was scraped into 150 μl lysis buffer (Mammalian Cell Lysis-1 Kit; Sigma-Aldrich, Taufkirchen, Germany). The total cell lysates were centrifuged at 10,000 g for 10 min, and the supernatants were analyzed by immunoblots. Equal amounts of protein (30 μg) were separated by 10% SDS-polyacrylamide gel electrophoresis. Immunoblots were probed with primary and secondary antibodies, and immunoreactive bands were visualized using 5-bromo-4-chloro-3-indolyl phosphate/nitro blue tetrazolium.
Cytokine ELISA
The cells were cultured at 3×103 cells per well in 96-well plates (100 μl culture medium per well). At a confluency of ∼80%, the cells were cultured in serum-free medium for 16 h. Subsequently, the culture medium was changed, and the cells were stimulated by growth factors and cytokines at doses indicated, in the presence of 0.5% serum. The supernatants were collected after 6 or 24 h, and the levels of PlGF-2 or VEGF-A165 in the cultured media (50 μl or 200 μl) were determined by ELISA (R&D Systems).
PCR
The total RNA of cultured cells was extracted by using the RNeasy Mini Kit (Qiagen, Hilden, Germany), and treated with DNase I (Roche). cDNA was synthesized from 1 μg total RNA using the RevertAid H Minus First Strand cDNA Synthesis Kit (Fermentas, St Leon-Roth, Germany). PCR was carried out using the Taq PCR Master Mix Kit (Qiagen) and the primer pairs described in Table 1. A 1-μl aliquot of the first-strand mixture and 1 μM of each gene-specific sense- and anti-sense primer were used for amplification in a final volume of 20 μl. Amplification was performed for 40 cycles with the PTC-200 Thermal Cycler (MJ Research, Watertown, Mass., USA). Each cycle consisted of 30 s at 94°C, 60 s at 60°C, and 2 min at 72°C.
Quantitative PCR (qPCR) was performed with the Single-Color Real-Time PCR Detection System (BioRad, Munich, Germany). The PCR solution contained 1 μl cDNA, specific primer set (1 μM each) and 10 μl of QuantiTect SYBR Green PCR Kit (Qiagen) in a final volume of 20 μl. The PCR parameters were initial denaturation and enzyme activation (one cycle at 95°C for 15 min); denaturation, amplification and quantification, 45 cycles at 95°C for 30 s, 60°C for 30 s, and 72°C for one minute; melting curve, 55°C with the temperature gradually increased (0.5°C) up to 95°C. The amplified samples were analyzed by standard agarose gel electrophoresis. The mRNA expression was normalized to the levels of GAPDH mRNA, by using the mathematical model of Pfaffl [29].
Statistics
The rates of BrdU incorporation, migration, and VEGF secretion are expressed as percent of untreated control (100%). For each test, at least three independent experiments were carried out in triplicate. Data are expressed as means±SD (mRNA analysis) or SEM; statistical significance (Student’s t-test, non-parametric Mann-Whitney U-test) was accepted at P<0.05.
Results
mRNA expression
To investigate whether RPE cells may produce and respond to PlGF, we performed firstly a RT-PCR analysis to determine whether cultured human RPE cells express mRNA for different members of the VEGF family of growth factors and their receptors. As shown in Fig. 1a, gene expression for VEGF-A, -B, -C, -D, and PlGF was detected. The expression level of the mRNA for VEGF-B was significantly higher compared with the level of VEGF-A mRNA, whereas no difference was observed in respect to the gene expressions of VEGF-A and -C (Fig. 1b). On the other hand, significant lower mRNA levels were observed for VEGF-D and PlGF compared to VEGF-A mRNA (Fig. 1b). The cells expressed the mRNAs for the receptors of these factors, VEGF-R1 (flt-1), VEGF-R2 (KDR/flk-1), neuropilin-1, and neuropilin-2 (Fig. 1a). The expression levels of the mRNAs for neuropilins were higher when compared with the mRNAs for flt-1 and KDR, as indicated by the significantly (P<0.001) lower cycle threshold numbers necessary for the detection of the mRNAs by qPCR (Fig. 1b). In addition to the cultured RPE cells, we investigated the mRNA expression in acutely isolated RPE cells. We found that, similarly to cultured cells, acutely isolated cells expressed the various mRNAs for the members of the VEGF family and their receptors (data not shown). The expression of the mRNAs for PlGF and its receptors suggest that RPE cells may produce and respond to this factor.
Cultured human RPE cells express mRNA for different members of the VEGF family of growth factors, as well as for their receptors. a RT-PCR analysis revealed the presence of mRNA for VEGF-A, -B, -C, -D, and PlGF, as well as for the receptors VEGF-R1 (flt-1), VEGF-R2 (KDR), neuropilin-1, and neuropilin-2. The cells were investigated after 16 (1) or 40 h (2) of serum-free culturing. The negative control (-) was done by adding water instead of cDNA. b Mean±SD number of cycles necessary to detect the mRNAs for the members of the VEGF family of growth factors (left) and for their receptors (right) by qPCR in cells which were cultured for 16 h. The detection thresholds were normalized to the relative cycle number necessary for the detection of GAPDH mRNA. A lower relative cycle number means a higher expression level of the mRNA. Significant differences versus. the cycle number for VEGF-A (left) and flt-1 mRNAs (right), respectively: *P<0.001
Regulation of mRNA expression
Since various growth factors and cytokines have been implicated in the progression of fibrovascular disease, we investigated using qPCR analysis whether the expression of mRNA for PlGF is regulated by different factors in RPE cells. The cells were treated with the factors for 2 or 24 h, and the relative mRNA levels in comparison to unstimulated control was determined. As shown in Fig. 2a, members of the TGF-β superfamily of growth factors (BMP-4 and TGF-β1) significantly increased the expression of mRNA for PlGF both at 2 and 24 h of culturing. Various other growth factors examined (VEGF, HGF, HB-EGF, PDGF) showed no influence on the expression of PlGF mRNA. This stimulation pattern was different from the pattern of the cytokine-dependent expression of mRNA for VEGF-A (Fig. 2b). PDGF, TGF-β1, and HB-EGF increased significantly the gene expression of VEGF-A after 2 h of incubation, while gene expression was decreased in the presence of BMP-4 and PlGF-2. The data suggest that the genes for PlGF and VEGF-A are differentially regulated in RPE cells by cytokines.
Effect of different growth factors and cytokines on the gene expression of PlGF (a) and VEGF-A (b) in human RPE cells. The factors were applied at 10 ng/ml for 2 or 24 h. The mRNA levels were determined by qPCR, and are expressed as folds of control. Means±SEM of three to six independent experiments using cells from different donors. Significant differences versus. untreated control: *P<0.05; **P<0.01; ***P<0.001
To investigate whether PlGF-2, TGF-β1, or VEGF-A165 also regulate the expression of the genes for other members of the VEGF protein family and for their receptors, a comparative gene expression analysis was carried out using qPCR. Exogenous PlGF-2 did not significantly alter the gene expression of VEGF-B, C, and D, and of the receptors (Fig. 3a). Similarly, exogenous BMP-4 had no effects on the gene expression of the other members of the VEGF protein family and of the receptors investigated (not shown). Exogenous TGF-β1 stimulated the gene expression of flt-1 and neuropilin-2 after 24 h of incubation, and decreased the mRNA level for neuropilin-1 (Fig. 3b). VEGF-A strongly enhanced the gene expression of the VEGF receptors, flt-1 and KDR, while it had no effects on the gene expression of neuropilins and the other VEGF subtypes investigated (Fig. 3c). The data suggest that members of the TGF-β superfamily of growth factors, but not VEGF-A, stimulate gene expression of PlGF in RPE cells.
Effects of exogenous PlGF-2 (a), TGF-β1 (b), and VEGF-A165 (c), respectively, on the gene expression of members of the VEGF protein family and of their receptors. The factors were applied at 10 ng/ml for 2 or 24 h. The mRNA levels were determined by qPCR, and are expressed as folds of control. Means±SEM of three to six independent experiments using cells from different donors. Significant differences versus untreated control: *P<0.05; **P<0.01
Secretion of PlGF-2
Since RPE cells express mRNA for PlGF (Fig. 1a) we investigated whether the cells secrete PlGF protein. The cells were stimulated with different growth factors and cytokines, as well as with serum, for 24 h, and subsequently, the concentration of PlGF-2 in the cultured media was measured by ELISA. The cells constitutively secreted PlGF-2 protein; the concentration of PlGF-2 in the supernatants at unstimulated conditions was ∼5 pg/ml. Addition of various members of the TGF-β superfamily of growth factors (BMP-4, TGF-β1, TGF-β2) to the culture medium significantly enhanced the content of PlGF-2 in the supernatants (Fig. 4a). Different growth factors (VEGF, PDGF, HB-EGF, bFGF, HGF) and pro-inflammatory cytokines (TNFα, IL-1β) did not enhance the release of PlGF-2 by the cells, while serum displayed a slight stimulating effect (Fig. 4a). The TGF-β1- and BMP-4-evoked stimulation of PlGF secretion was dose-dependent (Fig. 4a, inset). TGF-β1 evoked secretion of PlGF-2 at concentrations above 0.01 ng/ml, while the effect of BMP-4 was observed only at higher concentrations above 1 ng/ml. The data suggest that the secretion of PlGF is evoked mainly by TGF-β-related cytokines.
Human RPE cells secrete PlGF and VEGF proteins upon stimulation with members of the TGF-β superfamily of growth factors. a Secretion of PlGF-2. Inset: Concentration dependence of the effects of TGF-β1, BMP-4, and VEGF on the secretion of PlGF-2. b Secretion of VEGF-A165. The cells were stimulated with different factors (each at 10 ng/ml) and serum (5%), respectively, for 24 h; subsequently, the protein concentration in the cultured media was measured by ELISA. Data are expressed as percentage of untreated control (100%). Means±SEM of three to six independent experiments carried out in duplicate. Significant differences versus. untreated control: *P<0.05; **P<0.01; ***P<0.001
Secretion of VEGF-A
RPE cells are a major source of VEGF in the retina [3]. To investigate whether PlGF may alter the secretion of VEGF by RPE cells, we measured the content of VEGF-A protein in the supernatants that were derived from RPE cells cultured in the absence and presence of various growth factors and cytokines. The cells constitutively secreted VEGF-A, with concentrations between 100 and 250 pg/ml measured in the supernatants at untreated conditions. As shown in Fig. 4b, TGF-β1 and TGF-β2 strongly increased the VEGF-A content of the cultured media while BMP-4 and PlGF-2 were without effects. PDGF and HB-EGF evoked secretion of VEGF while bFGF and HGF were ineffective (Fig. 4b). Similar results were obtained in cultures that were stimulated for 6 or 24 h (not shown). It is concluded that PlGF does not alter the secretion of VEGF by RPE cells.
Cell proliferation
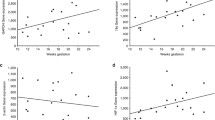
Since RPE cells express receptors for PlGF (Fig. 1) we determined whether exogenously applied PlGF may modulate cell responses which are important in the growth of fibrovascular tissue, i.e. cell proliferation and migration. Cell proliferation was determined by measurement of the DNA synthesis rate. Addition of PlGF-2 (at 10 ng/ml) to the culture medium did not alter the proliferation of RPE cells (Fig. 5a). In contrast, PDGF, a known mitogen for RPE cells [14], enhanced cell proliferation, while TGF-β1 and β2 decreased the proliferation at control conditions and in the presence of exogenous PDGF (Fig. 5a). BMP-4 and VEGF-A were without effects on cell proliferation. PDGF evoked a dose-dependent increase of RPE cell proliferation (Fig. 5b). PlGF-2, at a high concentration of 100 ng/ml, slightly decreased the cell proliferation (Fig. 5b).
PlGF is a motogen but not a mitogen for human RPE cells. a PDGF but not PlGF-2 nor BMP-4 stimulated the proliferation of RPE cells. TGF-β1 and -β2 decreased control proliferation, and inhibited the proliferation evoked by PDGF. All factors were tested at 10 ng/ml. b Dose-dependence of the effects of PlGF-2 and PDGF on the cell proliferation rate. c Dose-dependence of the chemotactic effects of PlGF-2 and VEGF-A165. Means±SEM of three to six independent experiments using cells from different donors. Significant differences versus. untreated control: *P<0.05; **P<0.01; ***P<0.001. Significant differences versus stimulation with PDGF: °P<0.05; °°P<0.01
Chemotaxis
The chemotaxis of RPE cells was investigated by using a modified Boyden chamber assay. As shown in Fig. 5c, exogenous PlGF-2 strongly enhanced the chemotaxis of RPE cells, with significant effects at concentrations above 0.01 ng/ml. In contrast, VEGF-A evoked a significantly smaller chemotactic response. The data indicate that PlGF-2 is not a mitogen but a relatively strong motogen for RPE cells.
Phosphorylation of ERK1/2, p38, and Akt
To determine whether PlGF activates intracellular signaling pathways in RPE cells that may be associated with the stimulation of cell migration, the phosphorylation levels of extracellular signal-regulated kinases 1/2 (ERK1/2), p38 MAPK, and Akt (protein kinase B) proteins were examined by using Western blotting. Exogenous PlGF-2 did not enhance the amount of the phosphorylated proteins (Fig. 6), suggesting that the chemotactic effect of this factor is not mediated by activation of the ERK1/2, p38 MAPK, or phosphatidylinositol 3-kinase (PI3K)-Akt signaling pathways. Similarly, VEGF, BMP-4, TGF-β1, or TGF-β2 failed to evoke phosphorylation, while exogenous PDGF evoked phosphorylation of all three signaling proteins (Fig. 6). Similar results were obtained after extension of the stimulation time up to 3 h or using a higher concentration (50 ng/ml) of PlGF-2 or VEGF (data not shown).
PDGF but not PlGF-2, VEGF-A165, BMP-4, TGF-β1, or TGF-β2 evoke phosphorylation of ERK1/2 (a), p38 (b), and Akt proteins (c) in human RPE cells. Amounts of total proteins are shown above; amounts of phosphorylated proteins are shown below. The cultures were stimulated with the growth factors (10 ng/ml) for 10 min. Similar results were obtained in three independent experiments using cells from different donors
Discussion
It has been shown that the co-expression of receptors for VEGF and PlGF, KDR and neuropilin-1, in fibrovascular tissues correlates with the degree of neovascularization in young patients with proliferative diabetic retinopathy [16]. PlGF facilitates endothelial cell proliferation and vascular permeability by potentiating the activity of VEGF [1, 8, 26], and the presence of PlGF is required for the angiogenic effect of VEGF in the ischemic retina [5]. Here, we show that human RPE cells produce, in addition to VEGF, also PlGF, and that PlGF stimulates the chemotaxis of RPE cells. The PlGF secreted by RPE cells may facilitate the formation of fibrovascular membranes in the course of the proliferative diabetic retinopathy, via stimulation of endothelial cell proliferation and RPE cell migration.
The present results confirm previous findings that human RPE cells in vitro express both VEGF receptors, flt-1 and KDR (Fig. 1a) [15]. In addition to the VEGF receptors, we found that RPE cells express receptors for PlGF, the neuropilins, and that the gene expression of neuropilins is significantly greater compared to the gene expression of VEGF receptors, flt-1 and KDR (Fig. 1a,b).
Despite the fact that TGF-β inhibits the proliferation of cultured endothelial cells [2, 13], it has been found to be a strong inducer of angiogenesis in vivo [31], probably via induction of angiogenic factors in cell types surrounding proliferating vessels [28]. Here, we describe that members of the TGF-β superfamily of growth factors strongly stimulate the gene expression of PlGF (Fig. 2a) and the secretion of PlGF protein in human RPE cells (Fig. 4a). In contrast, various other growth factors and pro-inflammatory cytokines displayed no effects on the expression of PlGF by RPE cells. In addition to PlGF, the RPE cells also produce and secrete VEGF. However, the cytokine-dependent regulation of PlGF and VEGF expression differed markedly. TGF-β induced elevation of gene and protein expression of both PlGF and VEGF (Figs 2 and 4), while BMP-4 increased the gene expression of PlGF and decreased the gene expression of VEGF. Distinct other growth factors (PDGF and HB-EGF) stimulated the expression of VEGF but not of PlGF (Figs 2 and 4). The present results support previous findings of a major role of TGF-β in the induction of VEGF secretion by RPE cells [22], and indicate that TGF-β plays also a crucial role in the expression of PlGF by RPE cells. It has been shown that the retinal expression of the mRNA for TGF-β1 is increased during the development of diabetic retinopathy, along with an increased gene expression of VEGF and PlGF [36]. The present results suggest that RPE cells stimulated by TGF-β-related growth factors may represent one source of the increased expression of PlGF in the diabetic retina. We found that PlGF did not induce secretion of VEGF (Fig. 4b), and vice versa, VEGF did not increase the secretion of PlGF (Fig. 4a), disclosing a direct relationship between PlGF and VEGF at the level of RPE cells. Apparently, TGF-β induces relatively independently the production and secretion of VEGF and PlGF in RPE cells. However, further studies are necessary to evaluate the relationships of the action of TGF-β on different cell types involved in the process of fibrovascular disease.
It has been shown previously that the receptor for PlGF, neuropilin-1, stimulates the migration of vascular endothelial cells, via activation of PI3K, p85, and RhoA [39]. We found that PlGF stimulates the chemotaxis of RPE cells (Fig. 5c), while it had only a slight inhibiting effect on cell proliferation at high concentration (Fig. 5b). The intracellular signaling pathways that are stimulated in RPE cells after activation of neuropilins by PlGF, and that stimulate cell migration, remains to be determined. As expected, the failure of an effect of PlGF on cell proliferation (Fig. 5a,b) is associated with an absence of enhanced phosphorylation of ERK1/2 by PlGF (Fig. 6). In various cell systems, cell migration is supported by activation of the p38 MAPK [32, 33, 37]. However, we did not found enhanced phosphorylation of p38 after stimulation with PlGF (Fig. 6). Likewise, Akt protein did not show phosphorylation in the presence of extracellular PlGF (Fig. 6), suggesting that PlGF did not stimulate the PI3K-Akt pathway in RPE cells.
In summary, we show that TGF-β-related growth factors induces the production and secretion of both VEGF and PlGF by RPE cells. Moreover, the migration of RPE cells stimulated by PlGF may contribute to the growth of fibrovascular tissue. It remains to be proven whether RPE cell-derived PlGF contributes to the progression of pathological neovascularization in situ.
Abbreviations
- bFGF:
-
basic fibroblast growth factor
- BMP:
-
bone morphogenetic protein
- BrdU:
-
bromodeoxyuridine
- ERK:
-
extracellular signal-regulated kinase
- flt:
-
FMS-related tyrosine kinase1 (VEGF-R1)
- GAPDH:
-
Glyceraldehyde-3-phosphate dehydrogenase
- HB-EGF:
-
heparin-binding epridermal growth factor-like growth factor
- HGF:
-
hepatocyte growth factor
- IL:
-
interleukin
- KDR:
-
kinase insert domain receptor (VEGF-R2)
- MAPK:
-
mitogen-activated protein kinase
- PCR:
-
polymerase chain reaction
- PDGF:
-
platelet-derived growth factor
- PI3K:
-
phosphatidylinositol-3 kinase
- PlGF:
-
placenta growth factor
- RPE:
-
retinal pigment epithelium
- TGF:
-
transforming growth factor
- TNF:
-
tumor necrosis factor
- VEGF:
-
vascular endothelial growth factor
- VEGF-R:
-
VEGF receptor
References
Autiero M, Waltenberger J, Communi D, Kranz A, Moons L, Lambrechts D, Kroll J, Plaisance S, De Mol M, Bono F, Kliche S, Fellbrich G et al. (2003) Role of PlGF in the intra- and intermolecular cross talk between the VEGF receptors flt1 and flk1. Nat Med 9:936–943
Baird A, Durkin T (1986) Inhibition of endothelial cell proliferation by type beta-transforming growth factor: interactions with acidic and basic fibroblast growth factors. Biochem Biophys Res Commun 138:476–482
Blaauwgeers HG, Holtkamp GM, Rutten H, Witmer AN, Koolwijk P, Partanen TA, Alitalo K, Kroon ME, Kijlstra A, van Hinsbergh VW, Schlingemann RO (1999) Polarized vascular endothelial growth factor secretion by human retinal pigment epithelium and localization of vascular endothelial growth factor receptors on the inner choriocapillaris. Evidence for a trophic paracrine relation. Am J Pathol 155:421–428
Cao Y, Ji WR, Qi P, Rosin A, Cao Y (1997) Placenta growth factor: identification and characterization of a novel isoform generated by RNA alternative splicing. Biochem Biophys Res Commun 235:493–498
Carmeliet P, Moons L, Luttun A, Vincenti V, Compernolle V, De Mol M, Wu Y, Bono F, Devy L, Beck H, Scholz D, Acker T et al. (2001) Synergism between vascular endothelial growth factor and placental growth factor contributes to angiogenesis and plasma extravasation in pathological conditions. Nat Med 7:575–583
Castellon R, Hamdi HK, Sacerio I, Aoki AM, Kenney MC, Ljubimov AV (2002) Effects of angiogenic growth factor combinations on retinal endothelial cells. Exp Eye Res 74:523–535
Cui JZ, Hinz BJ, Greve MD, Potter MJ, Hornan D, Samad A, To E, Matsubara JA (2003) Expression of neuropilin-1 in choroidal neovascular membranes. Can J Ophthalmol 38:41–45
Dull RO, Yuan J, Chang YS, Tarbell J, Jain RK, Munn LL (2001) Kinetics of placenta growth factor/vascular endothelial growth factor synergy in endothelial hydraulic conductivity and proliferation. Microvasc Res 61:203–210
Enzmann V, Kaufmann A, Hollborn M, Wiedemann P, Gemsa D, Kohen L (1999) Effective chemokines and cytokines in the rejection of human retinal pigment epithelium (RPE) cell grafts. Transpl Immunol 7:9–14
Frank RN, Amin RH, Eliott D, Puklin JE, Abrams GW (1996) Basic fibroblast growth factor and vascular endothelial growth factor are present in epiretinal and choroidal neovascular membranes. Am J Ophthalmol 122:393–403
Fuh G, Li B, Crowley C, Cunningham B, Wells JA (1998) Requirements for binding and signaling of the kinase domain receptor for vascular endothelial growth factor. J Biol Chem 273:11197–11204
Fujisawa H (2004) Discovery of semaphorin receptors, neuropilin and plexin, and their functions in neural development. J Neurobiol 59:24–33
Heimark RL, Twardzik DR, Schwartz SM (1986) Inhibition of endothelial regeneration by type-beta transforming growth factor from platelets. Science 233:1078–1080
Hinton DR, He S, Graf K, Yang D, Hsueh WA, Ryan SJ, Law RE (1998) Mitogen-activated protein kinase activation mediates PDGF-directed migration of RPE cells. Exp Cell Res 239:11–15
Hoffmann S, Masood R, Zhang Y, He S, Ryan SJ, Gill P, Hinton DR (2000) Selective killing of RPE with a vascular endothelial growth factor chimeric toxin. Invest Ophthalmol Vis Sci 41:2389–2393
Ishida S, Shinoda K, Kawashima S, Oguchi Y, Okada Y, Ikeda E (2000) Coexpression of VEGF receptors VEGF-R2 and neuropilin-1 in proliferative diabetic retinopathy. Invest Ophthalmol Vis Sci 41:1649–1656
Khaliq A, Foreman D, Ahmed A, Weich H, Gregor Z, McLeod D, Boulton M (1998) Increased expression of placenta growth factor in proliferative diabetic retinopathy. Lab Invest 78:109–116
Maglione D, Guerriero V, Viglietto G, Ferraro MG, Aprelikova O, Alitalo K, Del Vecchio S, Lei KJ, Chou JY, Persico MG (1993) Two alternative mRNAs coding for the angiogenic factor, placenta growth factor (PlGF), are transcribed from a single gene of chromosome 14. Oncogene 8:925–931
Migdal M, Huppertz B, Tessler S, Comforti A, Shibuya M, Reich R, Baumann H, Neufeld G (1998) Neuropilin-1 is a placenta growth factor-2 receptor. J Biol Chem 273:22272–22278
Miller JW, Adamis AP, Shima DT, D’Amore PA, Moulton RS, O’Reilly MS, Folkman J, Dvorak HF, Brown LF, Berse B et al. (1994) Vascular endothelial growth factor/vascular permeability factor is temporally and spatially correlated with ocular angiogenesis in a primate model. Am J Pathol 145:574–584
Mitamura Y, Tashimo A, Nakamura Y, Tagawa H, Ohtsuka K, Mizue Y, Nishihira J (2002) Vitreous levels of placenta growth factor and vascular endothelial growth factor in patients with proliferative diabetic retinopathy. Diabetes Care 25:2352
Nagineni CN, Samuel W, Nagineni S, Pardhasaradhi K, Wiggert B, Detrick B, Hooks JJ (2003) Transforming growth factor-β induces expression of vascular endothelial growth factor in human retinal pigment epithelial cells: involvement of mitogen-activated protein kinases. J Cell Physiol 197:453–462
Nakamura F, Goshima Y (2002) Structural and functional relation of neuropilins. Adv Exp Med Biol 515:55–69
Neufeld G, Kessler O, Herzog Y (2002) The interaction of neuropilin-1 and neuropilin-2 with tyrosine-kinase receptors for VEGF. Adv Exp Med Biol 515:81–90
Oh H, Takagi H, Otani A, Koyama S, Kemmochi S, Uemura A, Honda Y (2002) Selective induction of neuropilin-1 by vascular endothelial growth factor (VEGF): a mechanism contributing to VEGF-induced angiogenesis. Proc Natl Acad Sci USA 99:383–388
Park JE, Chen HH, Winer J, Houck KA, Ferrara N (1994) Placenta growth factor. Potentiation of vascular endothelial growth factor bioactivity, in vitro and in vivo, and high affinity binding to Flt-1 but not to Flk-1/KDR. J Biol Chem 269:25646–25654
Pe’er J, Folberg R, Itin A, Gnessin H, Hemo I, Keshet E (1996) Upregulated expression of vascular endothelial growth factor in proliferative diabetic retinopathy. Br J Ophthalmol 80:241–245
Pertovaara L, Kaipainen A, Mustonen T, Orpana A, Ferrara N, Saksela O, Alitalo K (1994) Vascular endothelial growth factor is induced in response to transforming growth factor-beta in fibroblastic and epithelial cells. J Biol Chem 269:6271–6274
Pfaffl M (2001) A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Res 29:2002–2007
Rakic JM, Lambert V, Devy L, Luttun A, Carmeliet P, Claes C, Nguyen L, Foidart, JM, Noel A, Munaut C (2003) Placental growth factor, a member of the VEGF family, contributes to the development of choroidal neovascularization. Invest Ophthalmol Vis Sci 44:3186–3193
Roberts AB, Sporn MB, Assoian RK, Smith JM, Roche NS, Wakefield LM, Heine UI, Liotta LA, Falanga V, Kehrl JH et al. (1986) Transforming growth factor type beta: rapid induction of fibrosis and angiogenesis in vivo and stimulation of collagen formation in vitro. Proc Natl Acad Sci USA 83:4167–4171
Saika S, Okada Y, Miyamoto T, Yamanaka O, Ohnishi Y, Ooshima A, Liu CY, Weng D, Kao WW (2004) Role of p38 MAP kinase in regulation of cell migration and proliferation in healing corneal epithelium. Invest Ophthalmol Vis Sci 45:100–109
Sharma GD, He J, Bazan HE (2003) p38 and ERK1/2 coordinate cellular migration and proliferation in epithelial wound healing: evidence of cross-talk activation between MAP kinase cascades. J Biol Chem 278:21989–21997
Soker S, Takashima S, Miao HQ, Neufeld G, Klagsbrun M (1998) Neuropilin-1 is expressed by endothelial and tumor cells as an isoform-specific receptor for vascular endothelial growth factor. Cell 92:735–745
Soker S, Miao HQ, Nomi M, Takashima S, Klagsbrun M (2002) VEGF165 mediates formation of complexes containing VEGFR-2 and neuropilin-1 that enhance VEGF165-receptopr binding. J Cell Biochem 85:357–368
Spirin KS, Saghizadeh M, Lewin SL, Zardi L, Kenney MC, Ljubimov AV (1999) Basement membrane and growth factor gene expression in normal and diabetic human retinas. Curr Eye Res 18:490–499
Surapisitchat J, Hoefen RJ, Pi X, Yoshizumi M, Yan C, Berk BC (2001) Fluid shear stress inhibits TNF-alpha activation of JNK but not ERK1/2 or p38 in human umbilical vein endothelial cells: Inhibitory crosstalk among MAPK family members. Proc Natl Acad Sci USA 98:6476–6481
Tamagnone L, Comoglio PM (2004) To move or not to move? Semaphorin signalling in cell migration. EMBO Rep 5:356–361
Wang L, Zeng H, Wang P, Soker S, Mukhopadhyay D (2003) Neuropilin-1-mediated vascular permeability factor/vascular endothelial growth factor-dependent endothelial cell migration. J Biol Chem 278:48848–48860
Acknowledgements
The authors thank Ute Weinbrecht for excellent technical assistance. This work was supported by grants from the Deutsche Forschungsgemeinschaft (KO 1547/4-1; BR 1249/2-1).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hollborn, M., Tenckhoff, S., Seifert, M. et al. Human retinal epithelium produces and responds to placenta growth factor. Graefe's Arch Clin Exp Ophthalmo 244, 732–741 (2006). https://doi.org/10.1007/s00417-005-0154-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-005-0154-9