Abstract
Background
Juvenile rheumatoid arthritis (JRA) is the most common systemic cause of pediatric uveitis in Europe and North America. Uveitis is commonly perceived as a frequent sequela of JRA and JRA-associated uveitis is commonly considered to have a complicated course with frequent adverse visual outcomes.
Methods
We performed a systematic literature search for series of consecutive patients with JRA (as defined by the American College of Rheumatology criteria) reporting on the frequency of uveitis and/or complications of uveitis, published between January 1980 and December 2004. The main outcome measures were: the cumulative incidence of uveitis in JRA, the cumulative incidence of adverse visual outcome and that of complications in JRA-associated uveitis. Additionally, the influence of gender, presence of antinuclear antibody (ANA) and disease onset subtype to the likelihood of developing uveitis were examined.
Results
Analysis of pooled data from the 26 eligible series suggested a cumulative incidence of uveitis in JRA of 8.3% [95% confidence intervals (CI), 7.5–9.1%]. The cumulative incidence of uveitis varied according to geographic location, being highest in Scandinavia, then the US, then Asia and lowest in India. JRA-associated uveitis was more common in pauciarticular than polyarticular onset patients [odds ratio (OR)=3.2, 95% CI, 2.33–4.36] and in ANA-positive than ANA-negative patients (OR=3.18, 95% CI, 2.22–4.54). Female gender was only a weak risk factor for the development of uveitis in JRA patients (OR=1.69, 95% CI 1.09–2.62) and was not statistically significant after considering disease onset subtypes. In JRA-associated uveitis the cumulative incidence of cumulative incidence of adverse outcome (visual acuity <20/40 OU) was 9.2% (95% CI: 4.7–15.8) of cataracts 20.5% (95% CI: 15.5–26.3), of glaucoma 18.9% (95% CI: 14.4–24.2) and of band keratopathy 15.7% (95% CI: 10.9–21.7).
Conclusion
The cumulative incidence of uveitis in JRA varies according to geographic location, presence of ANA, type of JRA onset and gender. Uveitis, adverse visual outcome, and complications in JRA are less frequent than commonly accepted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Juvenile rheumatoid arthritis (JRA)-associated uveitis is the most common systemic cause of uveitis of childhood in Europe and North America. [42, 58] Attempts to delineate the epidemiology and natural history of the ocular manifestations of JRA have been confounded by referral and publication bias, variability in study methodology including follow-up times, and by the multiplicity of classification schemes for juvenile arthritis (resulting in the overlapping, yet distinct, [6, 21, 38] entities of JRA, [7, 12], juvenile chronic arthritis (JCA) [18] and the twice revised juvenile idiopathic arthritis (JIA) [10, 45, 46]). Additionally, the introduction of routine screening for uveitis in JRA and advances in the management of JRA and JRA-associated uveitis (for example, the use of methotrexate) may have reduced the incidence of complications and may have improved visual outcome in recent years.
The range of cumulative incidence of JRA-associated uveitis has been reported to be between 1.4 and 25.0% [34, 55]. Complications of JRA-associated uveitis include secondary glaucoma (11–30% of patients) [23, 35], cataract (10–84% of patients) [16, 41], band keratopathy (0–70% of patients) and hypotony (0–17%) [11, 13, 35, 60]. An increased prevalence of myopia [20], keratoconjunctivitis sicca [29] and associations with spontaneous hyphema [22] and acquired Brown's syndrome have also been reported [59]. The cumulative incidence of patients with JRA-associated uveitis and a final visual acuity of less than 20/200 ranges from 0 to 38% [13, 31, 32, 41]. Consequently, whereas some studies suggest a complicated course in a substantial proportion of patients resulting in poor visual outcomes, yet other studies report fewer complications with better outcomes. The most common perception of the disease is more in line with the former reports [45, 31]. This is at odds with our own experience [11].
We have pooled available data published in the literature in order to appraise the frequency of JRA-associated uveitis in JRA patients, as well as the frequency of complications (cataract, glaucoma, band keratopathy) and adverse visual outcome.
Materials and methods
We conducted a meta-analysis, i.e. a formal and systematic review and quantitative analysis of the literature on JRA-associated uveitis and its complications [47]. We included series published between January 1980 and December 2004 reporting the incidence of uveitis (and/or the complications of JRA-associated uveitis) in consecutive patients diagnosed with JRA according to the American College of Rheumatology (ACR) criteria [7, 12]: persistent arthritis (swelling of a joint or limitation of motion with heat, pain or tenderness) of one or more joints for at least 6 weeks after exclusion of infectious, metabolic, traumatic and neoplastic causes as well as other autoimmune diseases (including psoriatic arthritis, ankylosing spondylitis, inflammatory bowel disease, systemic lupus erythematosus). We chose to use the ACR criteria, as these have been used for more than 30 years, they are familiar to most ophthalmologists in North America and are practical to use. In contrast, the more recent criteria for JIA have undergone two revisions in the last 7 years [10, 44, 46] and their validity has been questioned by some [6, 21, 50], as has the exclusion of patients with a family history of psoriasis in a second degree relative from the category of oligoarthritis [5, 50, 57]. Series of patients with juvenile arthritis diagnosed and classified by the European League against Rheumatism (EULAR) [18], World Health Organization/ International League Against Rheumatism (WHO/ILAR) [10, 44, 46], the Answell and Bywaters criteria [3] or in which the diagnostic criteria used were not specified were excluded. We did not include case reports. Our search strategy is summarized in Table 1.
All eligible studies were retrieved in hard copy and abstracted by one of the authors (P.E.C.). The total number of patients with JRA, the number of patients with each subtype of JRA, the sex and age distribution, the incidence of uveitis among all patients and in each subgroup of patients, length of follow-up, the visual outcomes and the incidence of complications of JRA-associated uveitis were extracted.
Adverse visual outcome was defined as visual acuity of less than 20/40 OU. Cumulative incidence of JRA-associated uveitis was calculated as the ratio of patients with uveitis to patients with JRA in the subgroup considered. Similarly the cumulative incidence of a given complication was calculated as the ratio of patients with the complication to patients with JRA in the subgroup considered. Subgroup analysis was carried out according to disease onset pattern (pauciarticular, polyarticular or systemic), gender, presence of antinuclear antibody (ANA) and according to geographic location (US, Scandinavian, Asian, Indian). Additionally, in order to see what the role of referral bias might be, we have presented separately the pooled results after excluding studies from single tertiary referral centers. Not all studies could be used for subgroup analysis or calculation of cumulative incidence rates of specific complications; on each occasion, all the available data were used. Since some series provided data for some subgroup analysis and not others, meaningful multivariate analysis for risk factors such as gender, ANA status and type of disease onset was not possible. 95% confidence intervals (CI) calculated using the exact binomial method are reported throughout our study. Comparisons were tested for statistical significance using the Fisher exact test or Spearman's R correlation coefficient and odds risk ratios were calculated.
Results
Thirty-six studies were identified as potentially relevant [1, 4, 8, 9, 11–16, 19, 23–25, 27, 30, 33–37, 39–41, 43, 47, 48, 51–56, 58, 60, 61]. Twenty-one series of JRA patients were included [1, 8, 9, 11–14, 19, 34, 35, 37, 39–41, 48, 52–55, 61, as well as five series of patients with JRA-associated uveitis [23, 24, 42, 51, 60]. Ten studies were excluded either because of overlap with series published at a later date (three studies) [36, 56, 58], because they used a duration criterion other than the ACR criterion of 6 weeks for the diagnosis of JRA (three studies) [16, 30, 33] or because they included patients that did not have JRA (four studies) [4, 15, 27, 47].
Methodological quality of included studies
The methodological quality of the studies meeting the inclusion criteria was variable. The length of follow-up was not specified in 12 of 25 series; the mean follow-up ranged from 2 to 12.7 years in the remaining 13 series (Tables 2 and 6). With the exception of a single prospective study [37], the remainder were retrospective studies. Only four of the studies were population based [11, 35, 37, 39], while four were multicenter studies [9, 13, 25, 41] including a single nationwide survey [25]. The majority of series came from the USA [1, 8, 9, 11–13, 23, 24, 34, 41, 52, 60], with four series from India [14, 48, 53, 55], three from East Asia [26, 40, 61], three from Scandinavia [19, 35, 37], and one each from Canada, Italy and New Zealand [39, 42, 51]. Sixteen studies provided data on the cumulative incidence of complications in patients with JRA-associated uveitis, while 13 studies provided data on the visual outcome of patients with JRA-associated uveitis (Table 6). With the exception of the series by Foster et al. [23, 24], none of the remaining series specified the diagnostic criteria for diagnosis of complications. Information on sex distribution, ANA positivity, age at onset of uveitis and interval to uveitis from diagnosis of JRA was lacking in the majority of the studies. The number of patients in each series ranged from 52 to 760.
Cumulative incidence of JRA-associated uveitis
As seen in Table 3, the cumulative incidence of JRA associated uveitis was 8.3% (95%CI, 7.5–9.1%). The cumulative incidence of uveitis in patients with pauciarticular onset JRA is 12.4% (95%CI, 10.9–13.9%), in patients with polyarticular onset JRA 4.3% (95% CI, 3.3–5.5%) and in patients with systemic onset JRA 1.8% (95% CI, 1.0–3.0%). Excluding series from single tertiary referral centers did not significantly alter the results. Since most cases of uveitis occur within the first 4 years after onset of arthritis [2, 45], we performed an analysis of pooled data after excluding series which specified a mean follow-up time of less than 4 years: the cumulative incidence of JRA-associated uveitis was 11.4% (95% CI, 9.9–13.2), 13.3% (95% CI, 11.0–15.8) for pauciarticular onset JRA patients and 5.1% (95% CI, 3.0–8.0) for polyarticular onset JRA patients.
For studies providing the mean length of follow-up, there was no correlation between mean length of follow-up and cumulative incidence of uveitis (Spearman R=−0.31, P=0.622). Similarly, there was no correlation between year of publication of a study and the cumulative incidence of uveitis in the total group of JRA patients (R=0.35, P=0.13) or pauciarticular onset JRA patients (R=0.17, P=0.51). This was also true considering US-based series alone (to avoid confounding from geographic variation).
Geographic variation in the cumulative incidence of JRA-associated uveitis
As seen in Table 3, the cumulative incidence of uveitis in JRA patients from US-based series was lower than in Scandinavian series (P<0.0001) but higher than in series from East Asia (P<0.0001) or India (P<0.0001). The cumulative incidence of uveitis for pauciarticular onset patients in US series was similar to that of Scandinavian series (P=0.3965) but higher than series from East Asia (P=0.0050) or India (P<0.0001). Finally, polyarticular onset JRA patients from Scandinavian series had the highest incidence of uveitis, followed by patients from the US, India and East Asia (P=0.0189, P<0.0001, P=0.0028). Differences in the cumulative incidence between studies from East Asia and India did not reach statistical significance.
Effect of JRA onset type on the cumulative incidence of uveitis
Considering the series which provide cumulative incidence for uveitis in both pauci- and polyarticular onset JRA patients (Table 2), the odds risk ratio (OR) of uveitis in pauciarticular onset JRA patients compared to polyarticular onset JRA patients is 3.20 (95% CI, 2.36–4.33).
Effect of gender on the cumulative incidence of uveitis
The cumulative incidence of JRA-associated uveitis in girls was 10.2% (95% CI, 8.3–12.3%) compared to 6.3% (95% CI, 4.2–9.0%) in boys (OR=1.70, 95% CI, 1.09–2.62). Differences in the cumulative incidence of JRA-associated uveitis between the two genders in pauci- or polyarticular onset JRA patients were not statistically significant (P=0.391 and P=0.734, respectively). It should be emphasized that not all the studies that provided data on cumulative incidence of JRA-associated uveitis provided data on each subgroup of patients (Table 4).
Gender differences in the cumulative incidence of JRA-associated uveitis were not statistically significant when the data from series from tertiary referral centers were excluded (P=0.0545). These comparisons did not take into account ANA status.
Effect of ANA on the cumulative incidence of uveitis
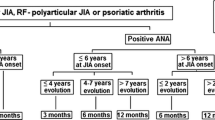
The cumulative incidence of uveitis in ANA positive patients was 17.7% (95% CI, 14.8–20.9%) compared with 6.3% (95% CI, 4.7–8.3%) of ANA negative patients, (OR=3.18, 95% CI, 2.22–4.54), as shown in Tables 5 and 6. In pauciarticular onset patients, the cumulative incidence of uveitis in ANA positive patients was 17.2% (95%CI 13.7–21.2%) compared with 7.5% (95% CI, 5.1–10.7) in ANA negative patients (OR=2.57, 95% CI, 1.62–4.07). There was no statistically significant difference in the cumulative incidence of uveitis between ANA positive and ANA negative polyarticular onset patients (OR=1.92, 95%CI, 0.82–4.48). The results were similar considering data from Scandinavia or North America alone (data not shown).
Cumulative incidence of adverse visual outcome and complications of uveitis
The cumulative incidence of adverse outcome was 9.2% (95% CI: 4.7–15.8). The cumulative incidence of cataract development was 20.5% (95% CI: 15.5–26.3), of glaucoma 18.9% (95% CI: 14.4–24.2) and of band keratopathy 15.7% (95% CI: 10.9–21.7). The cumulative incidence of adverse visual outcome and of complications of uveitis was not statistically different if series from single tertiary referral centers were excluded or if only series reporting on US-based patient cohorts were considered. There were no data on adverse visual outcome or complications of uveitis in studies from East Asia or India.
Discussion
Our meta-analysis suggests that the cumulative incidence of JRA-associated uveitis in pauciarticular patients 12.4% (95% CI: 10.9–13.9) was at the low end of the 10–30% rate that is commonly quoted in reviews of JRA-associated uveitis [2, 45]. Similarly the cumulative incidence of JRA-associated uveitis in polyarticular patients (4.3%, 95% CI 3.3–5.5%) was lower than 7–37% [2]. It may be argued that this may have been the result of pooling studies with variable follow-up times and that discussion of “incidence” without reference to time-at-risk is problematic: since the vast majority of cases of uveitis occur within the first 4 years after onset of arthritis [2, 45], we analyzed pooled data exclusively from series with 4 or more years of mean follow-up, and results were not statistically different. Finally, in order to exclude referral bias, we analysed pooled data exclusively from series from population based studies or studies involving multiple centers: the results were not statistically different.
It has been suggested that the cumulative incidence of JRA-associated uveitis has decreased over the years. Indeed, a study comparing the cumulative incidence of JRA-associated uveitis between 1989 and 1975 at a major tertiary referral center in Seattle supported this finding, even though this study did not attempt to control for possible changes in referral patterns [54]. Additionally, it is widely believed that the more prevalent use of methotrexate for control of active arthritis in JRA has caused the incidence of JRA-associated uveitis to decline [1]. We did not find a decrease in the cumulative incidence of JRA-associated uveitis in studies published more recently, although some recently published studies cover such long periods of time so that their results likely include patients from the era when methotrexate use was not prevalent.
The cumulative incidence of uveitis was found to vary depending on the country of origin of the study, being significantly greater in Scandinavian series, followed by series from the US, East Asia and finally India. Access to health care and patterns of over- or under-diagnosis of JRA or uveitis (ascertainment bias) might in part account for this finding. Additionally, no study from East Asia or India specified a length of follow-up; follow-up times in these studies may have been shorter than in studies from Scandinavia or the USA. However, genetic differences (e.g. frequency of HLA haplotypes) or environmental influences acting by modulating the immune response or modulating the virulence pattern of a putative causative agent may also partly account for the geographic variation.
JRA onset type is an established major risk factor for development of JRA-associated uveitis. Pauciarticular onset tripled the risk compared to polyarticular onset. It is noteworthy that in the series included in our meta-analysis there were no patients from Europe or North America with systemic onset JRA who developed JRA-associated uveitis.
The presence of ANA was shown to be a strong risk factor for the development of JRA-associated uveitis, nearly tripling the risk of pauciarticular onset patients (OR 2.57, 95% CI 1.62–4.07). ANA determination in the child diagnosed with JRA is therefore an important consideration for the appropriate risk stratification of that child.
Unexpectedly, female gender alone was only a weak risk factor (OR 1.69, 95% CI 1.09–2.62) for the development of uveitis in JRA patients and did not reach statistical significance when onset-type was considered. While it is possible that female gender may be associated with a higher incidence of pauciarticular disease and not be an independent risk factor for JRA-associated uveitis, it is more likely that the lack of association between female gender and uveitis after considering onset type may result from smaller sample sizes as well as the proportionately larger contribution from the East Asian cohorts to these samples [25, 40]: it is possible that female gender is not a risk factor for the development of uveitis in East Asian patients. The data presented in these series are not sufficient to allow a meaningful multivariate analysis to determine whether female gender is or not an independent risk factor after accounting for onset-type and/or ANA positivity.
A minority of studies provided data for visual outcome. Nonetheless, the adverse visual outcome cumulative incidence of 9.2%, although highly undesirable, is lower than commonly perceived [2]. It should be noted that no study reported on visual field deficits or measures of visual function other than visual acuity. Given a cumulative incidence of JRA-associated uveitis of 8.3%, it follows that the probability of a child with JRA developing an adverse visual outcome is less than 1%. However, it must be emphasized that this is the probability of the patient having vision of less than 20/40 OU and that individual eye visual impairment was not considered. Nevertheless, this is a valid outcome measure, since vision of 20/40 or better is consistent with a relatively good level of visual function.
The glaucoma and cataracts were complications in approximately one-fifth of patients with JRA-associated uveitis. Although definitions for these complications vary between studies and the severity of these complications may vary between patients, this is a useful estimate of the risk of development of either complication that may be quoted to the parents of a patient with JRA-associated uveitis. Since these complications both result from severe uveitis, it may be expected that they may be encountered together more often than by chance; there are insufficient data to support or refute this concept.
Our findings support the overall rationale of the current screening guidelines [2], with a slight modification. Currently, it is recommended that ANA positive pauci- and polyarticular onset JRA patients diagnosed before 7 years of age should undergo ophthalmologic examinations every 3–4 months (high risk) while ANA negative, pauci- or polyarticular onset JRA patients undergo ophthalmologic examinations every 6 months (medium risk)[2]. However, our results suggest that pauciarticular onset, ANA negative patients have the same risk of developing JRA associated uveitis (7.5%, 95%CI, 5.1–10.7%) as polyarticular onset, ANA positive patients (8.0%, 95% CI, 4.3–13.3); therefore, we suggest that consistency of screening recommendations between these two groups be considered.
Integration of immunogenetic data, [17, 28] with clinical and laboratory risk factors for occurrence of JRA-associated uveitis (such as JRA disease onset subtype, female gender, age of onset of arthritis, ANA positivity, serum concentrations of inflammatory markers) into a model that predicts patients who will develop uveitis would be highly desirable. Although prognosticators for adverse visual outcome in JRA-associated uveitis have been identified [16, 62] and a model that predicts JRA-associated uveitis severity has been developed [60], there exists no model that predicts which patients will develop JRA-associated uveitis. Until such a model is available, it is reasonable and advisable to continue to subject children with JRA to frequent ophthalmological examinations for early diagnosis of uveitis, although only a small proportion develop it.
Any analysis of the literature is subject to the limitations of each of the studies under analysis. A large, prospective population-based study of JRA patients would certainly best determine the incidence and outcomes of JRA associated uveitis. However, the relative rarity of the disease and its complications make it impractical, if not impossible to employ this strategy to answer these important questions. It is hoped that this analysis of the current literature provides a guide for physicians as they care for these patients, and discuss possible outcomes with the patients and their parents and caregivers.
References
Akduman L, Kaplan HJ, Tychsen L (1997) Prevalence of uveitis in an outpatient juvenile arthritis clinic: onset of uveitis more than a decade after onset of arthritis. J Pediatr Ophthalmol Strabismus 34:101–106
American Academy of Pediatrics Section on Rheumatology and Section on Ophthalmology (1992) Guidelines for ophthalmologic examinations in children with juvenile rheumatoid arthritis. Pediatrics 92:295–296
Ansell BM, Bywaters EGL (1959) Prognosis in Still's disease. Bull Rheum Dis 9:189–192
Berk AT, Kocak N, Unsal E (2001) Uveitis in juvenile arthritis. Ocul Immunol Inflamm 9:243–251
Berntson L, Fasth A, Andersson-Gare B, Herlin T, Kristinsson J, Lahdenne P, Marhaug G, Nielsen S, Pelkonen P, Rygg M (2002) The influence of heredity for psoriasis on the ILAR classification of juvenile idiopathic arthritis. J Rheumatol 29:2454–2458
Berntson L, Fasth A, Andersson-Gare B, Kristinsson J, Lahdenne P, Marhaug G, Nielsen S, Pelkonen P, Svensson E (2001) Construct validity of ILAR and EULAR criteria in juvenile idiopathic arthritis: a population based incidence study from the Nordic countries. J Rheumatol 28:2737–2743
Brewer EJ, Bass JC, Baum J, Cassidy JT, Fink C, Jacobs J, Hanson V, Levinson JE, Schaller J, Stillman JS (1977) Current proposed revision of JRA criteria. Arthri Rheum 20:195–199
Boone MI, Moore TL, Cruz OA (1998) Screening for uveitis in juvenile rheumatoid arthritis. J Pediatr Ophthalmol Strabismus 35:41–43
Bowyer SL, Roettcher PA, Higgins GC, Adams B, Myers LK, Wallace C, Rennebohm R, Moore TL, Pepmueller PH, Spencer C, Wagner-Weiner L, Rabinovich E, Passo M, Lovell DJ, Madson K, McCurdy D, Zemel L, Schinkler KN, Szer I, Kurtin P, Lindsley C (2003) Health status of patients with juvenile rheumatoid arthritis at 1 and 5 years after diagnosis. J Rheumatol 30:394–400
Brooks P (2001) Report of the sixth joint WHO/ILAR task force meeting on rheumatic diseases, January 16, 2000, Geneva, Switzerland. J Rheumatol 28:2540–2543
Carvounis PE, Herman DC, Cha SS, Burke JP (2005) Ocular manifestation of juvenile rheumatoid arthritis in Olmsted county, MN: a population-based study. Graefe's Arch Clin Exp Ophthalmol 243:217–221
Cassidy JT, Levinson JE, Bass JC, Baum J, Brewer EJ, Fink CW, Hanson V, Jacobs JC, Masi AT, Schaller JG, Fries JF, McShane D, Young D (1986) A study of classification criteria for a diagnosis of juvenile rheumatoid arthritis. Arthri Rheum 29:274–281
Chalom EC, Goldsmith DP, Koehler MA, Bittar B, Rose CD, Ostrov BE, Keenan GF (1997) Prevalence and outcome of uveitis in a regional cohort of patients with juvenile rheumatoid arthritis. J Rheumatol 24:2031–2034
Chandrasekaran AN, Rajendran CP, Madhavan R (1996) Juvenile rheumatoid arthritis- Madras experience. Indi J Pediatr 63:501–510
Chen CS, Robertson D, Hammerton ME (2004) Juvenile arthritis-associated uveitis: visual outcomes and prognosis. Can J Ophthalmol 39:614–620
Dana MR, Merayo-Lloves J, Schaumberg DA, Foster CS (1997) Visual outcomes prognosticators in juvenile rheumatoid arthritis-associated uveitis. Ophthalmology 104:236–244
De Inocencio J, Giannini EH, Glass DN (1993) Can genetic markers contribute to the classification of juvenile rheumatoid arthritis? J Rheumatol 20:S12–S17
European League Against Rheumatism. EULAR Bulletin No. 4: Nomenclature and classification of arthritis in children. Basel: National Zeitung AG; 1977.Wood P (1978) Nomenclature and classification of arthritis in children. In: Munthe E (ed) The care of Rheumatic Children. EULAR publications, Basel, p 47
Flato B, Lien G, Smerdel A, Vinje O, Dale K, Johnston V, Sorskaar D, Moum T, Ploski R, Fore O (2003) Prognostic factors in juvenile rheumatoid arthritis: a case-control study revealing early predictors and outcome after 14.9 years. J Rheumatol 30:386–393
Fledelius H, Zak M, Pederson FK (2001) Refraction in juvenile chronic arthritis: a long-term follow-up study, with emphasis on myopia. Acta Ophthalmol Scand 79:237–239
Foeldvari I, Biddle M (2000) Validation of the proposed ILAR classification criteria for juvenile idiopathic arthritis. International League of Associations for Rheumatology. J Rheumatol 27:1069–1072
Fong DS, Raizman MB (1993) Spontaneous hyphema associated with anterior uveitis. Br J Ophthalmol 77:635–638
Foster S, Havrlikova K, Baltatzis S, Christen WG, Merayo-Lloves J (2000) Secondary glaucoma in patients with juvenile rheumatoid arthritis-associated iridocyclitis. Acta Ophthalmol Scand 78:576–579
Foster CS, Barrett F (1993) Cataract development and cataract surgery in patients with juvenile rheumatoid arthritis-associated iridocyclitis. Ophthalmology 100:809–817
Fujikawa S, Masahiko O (1997) Clinical analysis of 570 cases with juvenile rheumatoid arthritis: results of a nationwide retrospective study in Japan. Acta Paediatrica Japonica 39:245–249
Giannini EH, Brwer EJ, Kuzmina N, Shaikov A, Maximov A, Vorontsov I, Fink C, Newman AJ, Cassidy JT, Zemel LS (1992) Methotrexate in resistant juvenile rheumatoid arthritis. Results of the USA-USSR Double blind, placebo-controlled trial. N Engl J Med 326:1043–1049
Gupta K, Chintu C, Raghu MB (1981) Juvenile rheumatoid arthritis in Zambian children. East Afr Med J 58:344–353
Haas JP, Truckenbrodt H, Paul C, Hoza J, Scholtz S, Albert ED (1994) Subtypes of HLA-DRB1*03, *08, *11, *12, *13 and *14 in early onset pauciarticular juvenile rheumatoid arthritis (EOPA) with and without iridocyclitis. Clin Exp Rheumatol 12S:7–14
Jain V, Singh S, Sharma A (2001) Keratoconjunctivitis sicca is not uncommon in children with juvenile rheumatoid arthritis. Rheumatol Int 20:159–162
Kadayitcilar S, Eidem B, Tumer B (2003) Uveitis in childhood. J Pediatr Ophthalmol Strab 40:335–340
Kanski JJ (1990) Juvenile arthritis and uveitis. Surv Ophthalmol 34:253–267
Key SN, Kimura SJ (1975) Iridocyclitis associated with juvenile rheumatoid arthritis. Am J Ophthalmol 80:428–429
Khuffash FA, Majeed HA (1988) Juvenile rheumatoid arthritis among Arab children. Scand J Rheumatol 17:393–395
Kodsi SR, Rubin SE, Milojevic D, Ilowite N, Gottlieb B (2002) Time of onset of uveitis in children with juvenile rheumatoid arthritis. J AAPOS 6:373–376
Kotaniemi K, Kaipiainen-Seppanen O, Savolainen A, Karma A (1999) A population-based study of uveitis in juvenile rheumatoid arthritis. Clin Exp Rheumatol 17:119–122
Kobayashi T, Tanaka S, Maeda M, Okubo H, Matsuama T, Watanabe N (1993) A study of prognosis in 52 cases with juvenile rheumatoid arthritis. Acta Paediatr Jpn 35:439–446
Kunnamo I, Kallio P, Pelkonen P (1986) Incidence of arthritis in urban Finnish children. A prospective study. Arthr Rheum 29:1232–1238
Laxer RM (1993) What's in a name: the nomenclature of juvenile rheumatoid arthritis. J Rheumatol 20:S1–S3
McGill NW, Gow PJ (1987) Juvenile rheumatoid arthritis in Auckland: a long term follow up study with particular reference to uveitis. Aust N Z J Med 17:305–308
Oh KT, Hong KP, Kim TH, Jun JB, Jung SS, Lee IH, Bae SC, Kim SY (1996) High incidence of HLA-B27 and low incidence of ANA in Korean juvenile rheumatoid arthritis: a descriptive cross-sectional study to analyze profiles related to prognosis [abstract]. Arthr Rheum 39:S54
Oren B, Sehgal A, Simon JW, Lee J, Blocker RJ, Biglan AW, Zobal-Ratner J (2001) The prevalence of uveitis in juvenile rheumatoid arthritis. J AAPOS 5:2–4
Paivonsalo-Hietanen T, Tuominen J, Saari KM (2000) Uveitis in children: population based study in Finland. Acta Ophthalmol Scand 78:84–88
Paroli MP, Speranza S, Marino M, Pirraglia MP, Pivetti-Pezzi P (2003) Prognosis of juvenile rheumatoid arthritis-associated uveitis. Eur J Ophthalmol 13:616–621
Petty RE, Smith JR, Rosenbaum JT (2003) Arthritis and uveitis in childhood. A pediatric rheumatology perspective. Am J Ophthalmol 135:879–884
Petty RE, Southwood TR, Baum J, Bhettay E, Glass DN, Manners P, Maldonado-Cocco J, Suarez-Almazor M, Orozco-Alcala J, Prieur AM (1998) Revision of the proposed classification criteria for juvenile idiopathic arthritis: Durban 1997. J Rheumatol 25:1991–1994
Petty RE, Southwood TR, Manners P, Baum J, Glass DN, Goldenberg J, He X, Maldonado-Cocco J, Orozco-Alcala J, Prieur AM, Suarez-Almazor ME, Woo P (2004) International League of Associations for Rheumatology classification of Juvenile Idiopathic Arthritis: second revision, Edmonton, 2001. J Rheumatol 31:390–392
Pongpanich B, Daengroongroj P (1988) Juvenile rheumatoid arthritis: clinical characteristics of 100 Thai patients. Clin Rheumatol 7:257–261
Porkodi R, Subramaniam R, Krishnamurthy V, Madhavan R, Parthiban M, Chandrasekaran AN (1990) Pattern of rheumatic diseases in South India IV. Clinical profile of juvenile rheumatoid arthritis. J Assoc Phys Ind 38:771–773
Powe NR, Schein OD, Giesen SC, Tielsch JM, Luthra R, Javitt J, Steinberg EP (1994) Synthesis of the literature on visual acuity and complications following cataract extraction with intraocular lens implantation. Arch Ophthalmol 112:239–252
Ramsey SE, Bolaria RK, Cabral DA, Malleson PN, Petty RB (2000) Comparison of criteria for the classification of childhood arthritis. J Rheumatol 27:1283–1286
Rosenberg AM, Oen KG (1986) The relationship between ocular and articular disease activity in children with juvenile rheumatoid arthritis and associated uveitis. Arthr Rheum 29:797–800
Schwartz MM, Simpson P, Kerr KL, Jarvis JN (1997) Juvenile rheumatoid arthritis in African Americans. J Rheumatol 24:1826–1829
Seth V, Kalra SK, Semwal OP, Jain Y (1996) Clinico-immunological profile in juvenile rheumatoid arthritis-an Indian experience. Ind J Pediatr 63:293–300
Sherry DD, Mellins ED, Wedgwood RJ (1991) Decreasing severity of chronic uveitis in children with pauciarticular arthritis. Am J Dis Child 145:1026–1028
Singh S, Salaria M, Kumar L, Minz R, Data U, Sehgal S (1999) Clinico-immunological profile of juvenile rheumatoid arthritis. Ind Pediatr 36:449–454
Towner SR, Michet CJ Jr, O'Fallon WM, Nelson AM (1983) The epidemiology of juvenile arthritis in Rochester, Minnesota 1960–1979. Arthr Rheum 26:1208–1213
Tsitami E, Bozzola E, Magni-Manzoni S, Viola S, Pistorio A, Ruperto N, Martini A, Ravelli A (2003) Positive family history of psoriasis does not affect the clinical expression of juvenile idiopathic arthritis patients with oligoarthritis. Arthritis Rheum 49:488–493
Tugal-Tutkan I, Havrlikova K, Power WJ, Foster CS (1996) Changing pattern in uveitis of childhood. Ophthalmology 103:375–383
Wang FM, Wertenbaker C, Behrens MM, Jacobs JC (1984) Acquired Brown's syndrome in children with juvenile rheumatoid arthritis. Ophthalmology 91:23–26
Wolf MD, Lighter PR, Ragsdale CG (1987) Prognostic factors in the uveitis of juvenile rheumatoid arthritis. Ophthalmology 94:1242–1248
Wu CJ, Huang JL, Yang MH, Yan DC, Ou LS, Ho HH (2001) Clinical characteristics of juvenile rheumatoid arthritis in Taiwan. J Microbiol Immunol Inf 34:211–214
Zulian F, Martini G, Falcini F, Gerloni V, Zannin ME, Pinello L, Fantini F, Facchin P (2002) Early predictors of severe course of uveitis in oligoarticular juvenile idiopathic arthritis. J Rheumatol 29:2446–2453
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by a research grant from the Department of Ophthalmology, Mayo Clinic, Rochester, MN and an unrestricted grant from Research to Prevent Blindness, Inc. New York, New York.
Rights and permissions
About this article
Cite this article
Carvounis, P.E., Herman, D.C., Cha, S. et al. Incidence and outcomes of uveitis in juvenile rheumatoid arthritis, a synthesis of the literature. Graefe's Arch Clin Exp Ophthalmo 244, 281–290 (2006). https://doi.org/10.1007/s00417-005-0087-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-005-0087-3