Abstract
Introduction
In adults, evaluation of fundus autofluorescence (AF) plays an important role in the differential diagnosis of retinal diseases. The aim of this study was to evaluate the feasibility of recording AF in children and teenagers and to define typical AF findings of various hereditary retinal diseases during childhood.
Methods
Fifty patients aged 2 to 16 years with hereditary retinal diseases were analysed using the HRA (Heidelberg Retina Angiograph). To enhance the AF signal, a mean of up to 16 single images was calculated. Twenty healthy children (aged 4–16 years) served as controls.
Results
In many children as young as 5 years of age and even in one 2-year-old child good AF images could be obtained. To achieve high quality images, larger image series (about 50 single images) were taken and appropriate single images were chosen manually to calculate the mean. Characteristically, Stargardt disease shows a central oval area of reduced AF, often surrounded by more irregular AF. In patients with Best disease, a central round structure with regular or irregular intense AF is visualised. Some patients with X-linked retinoschisis show central radial structures. In many patients with rod-cone dystrophies, a central oval ring-shaped area of increased AF is present. In early-onset severe retinal dystrophy (EOSRD) with RPE65 mutations AF is completely absent, whereas in other forms of Leber congenital amaurosis, AF is normal.
Discussion
Fundus autofluorescence may visualise disease-specific distributions of lipofuscin in the retinal pigment epithelium, often not (yet) visible on ophthalmoscopy. AF images can be used in children to differentiate hereditary retinal diseases and to facilitate follow-up controls. In many cases, four single images are sufficient to analyse the AF pattern.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Fundus autofluorescence (AF) is due to the accumulation of lipofuscin in the retinal pigment epithelium (RPE). An important fluorescent component of lipofuscin is A2E, which is derived from N-retinylidene-phosphatidyl-ethanolamine chemically modified upon digestion of phagocytosed photoreceptor outer segments [14–17, 23]. In healthy individuals it accumulates with age within the lysosomal compartment [16, 36]. Alterations in AF reflect changes in the lipofuscin contents of the RPE that may not be visible on ophthalmoscopy.
In adults, evaluation of fundus autofluorescence (AF) plays an important role in the differential diagnosis and follow-up of retinal diseases, especially in age-related macular degeneration and hereditary diseases [3–5, 9–11]. Little is known about the feasibility of recording AF in younger children with hereditary retinal dystrophies, where testing may be hampered by lack of compliance, nystagmus and photophobia.
The aim of this study was to systematically evaluate AF in children and teenagers with hereditary retinal dystrophies and to characterise typical AF findings of various diseases.
Materials and methods
Subjects
All individuals included in this study were informed about the objectives of the examination and volunteered to participate. Informed consent was taken from the parents or legal guardians according to the tenets of the Declaration of Helsinki. The study was approved by the Ethical Committee of the University of Regensburg.
Fifty children and teenagers aged 2–16 years with hereditary retinal diseases attending our department in the years 1999–2004 were included in the study (28 boys and 22 girls). Clinical examination included best-corrected visual acuity, refraction, slit-lamp biomicroscopy and funduscopy, and evaluation of nystagmus. Diagnosis was mainly based on clinical findings and electrophysiology (according to the International Society for Clinical Electrophysiology of Vision [ISCEV] standard); molecular genetic results were available in 22 of the patients. For comparison, we also examined 20 children aged 4–16 years with no sign or symptom of any retinal disease attending our department for other causes like refractive errors, squint or anterior segment pathologies.
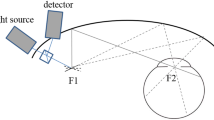
Fundus autofluorescence
Autofluorescence was recorded using a standard confocal scanning laser ophthalmoscope (Heidelberg Retina Angiograph, HRA; Heidelberg Engineering, Heidelberg, Germany). Alignment of the head and eye position and gain adjustment were performed with the infrared mode; subsequently the camera was switched to the AF laser. The detector sensitivity of the laser scanning camera was adjusted to the amount of AF present. Series of about 50 single pictures per eye were taken with a velocity of 6 images/s. Total exposure times were kept as short as possible, and the field of view was always 30×30°. To increase the signal-to-noise ratio of the AF signal, we aligned up to 16 images (a minimum of 4 images) using the software integrated into the instrument and calculated a mean image from these [22]. These single images were chosen manually on the basis of good quality and identical fundus area.
Results
The distribution of age and retinal diseases of the 50 patients is shown in Fig. 1. AF images were obtained in 48 out of 50 children with hereditary retinal diseases and in 19 out of 20 children with no retinal disease. Only 3 children (one aged 3 years with Leber congenital amaurosis, one aged 4 years with X-linked retinoschisis, and one aged 4 y with strabismus) could not cooperate sufficiently to obtain at least four images showing the same image area without artefacts. Photophobia and nystagmus made testing difficult, especially in patients with Leber congenital amaurosis (4 patients), but these problems were overcome by showing a fixation light behind the examiner, using larger image series and choosing manually the single images for calculating means.
Age-matched controls
Children in this group had no signs or symptoms of hereditary retinal disease, but 8 had strabismus. In all 19 children in whom we could obtain images, AF was easily detectable outside the fovea, optic nerve head, and large vessels. The fovea was darker than the surrounding retina, and AF was absent in the area of the optic nerve head and the large vessels (Fig. 2).
Stargardt macular dystrophy/cone-rod-dystrophy
We examined 14 children aged 6–16 years with either Stargardt macular dystrophy (STGD; 12 children with normal electroretinogram [ERG], with or without fundus flavimaculatus, 5 with molecular genetically determined ABCA4 mutations) or with cone-rod dystrophies (CRD; 2 children with reduced amplitudes in photopic more than scotopic Ganzfeld ERG). In all patients we were able to obtain AF images. These showed a central oval area of reduced AF in all patients. In patients with fundus flavimaculatus, this area was surrounded by small disseminated spots of reduced and increased AF (Fig. 3b,c). The AF aspect of CRD was similar (Fig. 3d).
Autofluorescence in patients with Stargardt disease/cone-rod dystrophy. a Stargardt disease (in a 10-year-old girl, VA 0.1/0.1): central oval area of reduced AF surrounded by small disseminated spots of reduced and increased AF. b Stargardt disease with fundus flavimaculatus (in a 9-year-old girl, VA 0.1/0.1): central oval area of reduced AF surrounded by small disseminated spots of reduced and increased AF. c Stargardt disease with fundus flavimaculatus (in a 10-year-old girl, VA 0.1/0.1, mutation in ABCA4): central oval area of reduced AF with some irregularities inside, surrounded by small disseminated spots of reduced and increased AF. d Cone-rod dystrophy (in a 10 year-old girl, VA 0.1/0.1, no molecular genetics performed): central oval area of reduced AF surrounded by small disseminated spots of increased AF
Best vitelliform macular dystrophy
Seven children aged 5–12 years with molecular genetically determined Best vitelliform macular dystrophy were examined [34]. AF images were of obtained in all of them.
Deposits of lipofuscin-like material were visualised in all patients. A typical vitelliform lesion shows as a central round area of increased AF (Fig. 4a). In the pseudohypopyon stage, increased AF is more pronounced in the lower part of the lesion (Fig. 4b). Later stages present with more irregular AF within the lesion and with disseminated spots of increased AF (Fig. 4c).
Autofluorescence in patients with Best vitelliform macular dystrophy. a A 5-year-old boy, with hBest1 mutation, VA 1.0/1.0, vitelliform stage: central round areas of increased AF. b An 11-year-old boy, with hBest1 mutation, VA 0.8/0.8, pseudohypopyon stage: increased AF (more pronounced in the lower part of the lesions). c A 14-year-old boy, with hBest1 mutation, VA 0.3/0.9, OD vitelliruptive stage with some scarring, OS vitelliform stage: irregular AF within the lesion with disseminated spots of increased AF, OD centrally: no AF corresponding to the scar
X-linked juvenile retinoschisis
Seven boys aged 4–15 years with X-linked juvenile retinoschisis (XLRS) were examined. One 4-year-old boy did not have sufficient cooperation for AF. Examples of AF images are shown in Fig. 5. Central AF was abnormal in all patients. Some patients showed central radial structures (Fig. 5a–c), others a more irregular AF pattern (Fig. 5d).
Autofluorescence in patients with X-linked juvenile retinoschisis. a A 5-year-old boy, VA 0.4/0.4: central radial structures of increased AF. b Same patient as a at the age of 7 years (VA stable): clearer AF image due to better cooperation: central radial structures of increased AF. c A 14-year-old boy, VA 0.4/0.4: centrally irregular AF. d A 15-year-old boy, VA 0.6/0.4: radiating AF structure corresponding to the cystic maculopathy
Rod-cone dystrophy
We examined 12 children aged 2–15 years. These included 11 patients with rod-cone dystrophy (RCD) and one with Bardet-Biedl syndrome. A characteristic feature was a parafoveal ring of increased AF. This ring showed a high degree of interocular symmetry, the size of the ring was not correlated with visual acuity (Fig. 6).
Autofluorescence in patients with rod-cone dystrophies: parafoveal ring of increased AF in all patients. a A 2-year-old girl, VA 0.3/0.3, rod-cone dystrophy (OD: left: central area of increased AF, right: lower part of the retina with confluent spots of increased AF). b A 6-year-old boy, VA 0.16/0.16, rod-cone dystrophy. c An 11-year-old girl, VA 0.05/0.05, rod-cone dystrophy (the patients in Fig. 6b and c are siblings). d A 15-year-old girl, VA 0.1/0.2, Bardet-Biedl-syndrome
Leber congenital amaurosis/early onset severe retinal dystrophy
Ten children aged 3–14 years were examined, 4 with typical Leber congenital amaurosis (LCA) and 6 with early onset severe retinal dystrophy (EOSRD) associated with RPE65 mutations [22, 25]. Testing was difficult due to photophobia and nystagmus. One 3-year-old boy with LCA did not show sufficient cooperation. In the other 3 children with LCA AF was clearly present (Fig. 7a). In the children with EOSRD associated with RPE65 mutations, no AF at all was visible (Fig. 7b): The image brightness over the optic disc, i.e. an area with physiological absence of AF was comparable to that of the posterior pole.
Autofluorescence in patients with Leber congenital amaurosis (LCA) and early onset severe retinal dystrophy (EOSRD). a A 7-year-old girl, VA 0.1/0.1, LCA (unknown genotype, no mutations in RPE65 detected): AF clearly present. b A 12-year-old girl, VA 0.1/0.2, EOSRD with RPE65 mutations: no AF. (As there was no AF detected, the sensitivity of the detector was upregulated. The normal optic disc does not have any AF. As image brightness over the optic disc is comparable to that of the posterior pole in this image, the brightness is due to the upregulated detector sensitivity and not due to “real” AF. For details see [22])
Discussion
This is the first systematic evaluation of fundus autofluorescence in children with hereditary retinal diseases, and age-matched children. Up to now the earliest age at which AF recordings are technically possible and whether there is any AF already present in younger children have not been clear. No more than one report of a 6-year-old child with Best disease and one age-matched control has been published [31]. In our study, evaluation of fundus AF could be obtained in most children starting from 5 years of age, and even in one 2-year-old girl. We could not see any correlation of the images with age. AF findings in healthy children were similar to those in adults [6, 10, 18, 22, 27].
To achieve high quality images, it is mandatory to record image series of about 50 single images and to choose appropriate single images manually. Light safety in young children with retinal degeneration and with normal retinal status is crucial. Special care was given to shorten exposure time. The American National Standards Institute (ANSI) norm (with no differentiation between children and adults) allows exposure times of 108 min for 30°. Actual exposure times of about 1 min are therefore about a 100-fold lower than the allowed HRA thresholds.
We identified typical AF patterns in children with five hereditary retinal diseases.
In Stargardt macular dystrophy (STGD, OMIM 248200) central oval areas of reduced AF were present in all patients. In fundus flavimaculatus these were surrounded by small disseminated spots of increased and reduced AF. These are assumed to be active flecks (increased AF) or resolved flecks (reduced AF) [20]. Our findings were similar to those in adults [9, 10, 19–21]. There was no systematic difference in AF between STGD and CRD in our patients. Lois et al. [21] postulated that patients with low levels of AF at the centre and low or normal levels temporally and nasally may have more peripheral cone and rod dysfunction than patients with higher peripheral AF levels. Cideciyan et al. [2] suggested a disease sequence for ABCA4 mutations to start with normal AF intensity, which increases and then decreases again in advanced disease stages.
In Best vitelliform macular dystrophy (OMIM 153700) deposits of lipofuscin-like material in the subretinal space can easily be visualised and are often more striking than on ophthalmoscopy. This is in accordance with descriptions in the literature [1, 10, 12, 31, 34]. Lesion size did not correlate with visual acuity, but lower visual acuity was associated with a more irregular AF pattern due to scarring or haemorrhage.
In X-linked retinoschisis (XLRS; OMIM 312700) AF imaging is not a standard diagnostic tool. Our AF findings reflect the typical radiating cystic maculopathy. AF intensity in the bright radial structures was similar to AF intensity outside the macula, AF intensity in the darker structures was comparable to a reduction in AF normally present due to shadowing effects of macular pigment. To date no AF findings have been published in patients with XLRS. This aspect in some of our patients was similar to those with isolated foveal retinoschisis [13]. Although alterations in the RPE may occur later in the disease process [8, 30], the typical finding in XLRS implies a superficial splitting within the nerve fibre layer, which can be visualised by optical coherence tomography (OCT) [7, 24, 30]. The AF alterations presented here could therefore reflect effects of differences in retinal thickness and/or shadowing effects or effects of different macular pigment content without actually representing changes in the lipofuscin content of the RPE.
Young patients with rod-cone dystrophies presented with a parafoveal ring of high-density AF. This is similar to findings in adults [26, 28, 35] and may represent a boundary of demarcation between normal and severely abnormal retinal function, as shown by correlations with pattern ERGs and fine matrix mapping [26, 28]. No areas of decreased AF were present in our patients, in contrast to older patients with decreased AF at the site of atrophic areas [32, 33].
In typical Leber congenital amaurosis AF was clearly present [22, 29]. In contrast, patients with early onset severe retinal dystrophy associated with RPE65 mutations did not show AF. Due to a defect in the retinol cycle, formation of rhodopsin is absent or largely decreased and therefore no lipofuscin is formed in the RPE [22]. Lack of AF despite an essentially normal looking fundus is a clinical marker of this genotype.
Conclusion
Evaluation of fundus autofluorescence is possible in many children as young as 5 years of age and even in some younger children. Fundus AF may visualise a disease-specific distribution of lipofuscin in the retinal pigment epithelium, often not (yet) visible on ophthalmoscopy. AF images can be used in children to differentiate hereditary retinal diseases and to facilitate follow-up controls. To achieve high quality images, it is mandatory to record larger image series and choose appropriate single images manually. In many cases, four single images are sufficient to analyse the AF pattern.
References
Chung JE, Spaide RF (2004) Fundus autofluorescence and vitelliform macular dystrophy. Arch Ophthalmol 122:1078–1079
Cideciyan AV, Aleman TS, Swider M, Schwartz SB, Steinberg JD, Brucker AJ, Maguire AM, Bennett J, Stone EM, Jacobson SG (2004) Mutations in ABCA4 result in accumulation of lipofuscin before slowing of the retinoid cycle: a reappraisal of the human disease sequence. Hum Mol Genet 13:525–534
Delori FC, Dorey CK, Staurenghi G, Arend O, Goger DG, Weiter JJ (1995) In vivo fluorescence of the ocular fundus exhibits retinal pigment epithelium lipofuscin characteristics. Invest Ophthalmol Vis Sci 36:718–729
Delori FC, Staurenghi G, Arend O, Dorey CK, Goger DG, Weiter JJ (1995) In vivo measurement of lipofuscin in Stargardt's disease—fundus flavimaculatus. Invest Ophthalmol Vis Sci 36:2327–2331
Delori FC, Fleckner MR, Goger DG, Weiter JJ, Dorey CK (2000) Autofluorescence distribution associated with drusen in age-related macular degeneration. Invest Ophthalmol Vis Sci 41:496–504
Delori FC, Goger DG, Dorey CK (2001) Age-related accumulation and spatial distribution of lipofuscin in RPE of normal subjects. Invest Ophthalmol Vis Sci 42:1855–1866
Eriksson U, Larsson E, Holmstrom G (2004) Optical coherence tomography in the diagnosis of juvenile X-linked retinoschisis. Acta Ophthalmol Scand 82:218–223
Gass JDM (1997) Heredodystrophic disorders affecting the pigment epithelium and retina. In: JDM Gass (ed) Stereoscopic atlas of macular diseases, diagnosis and treatment. Mosby, St. Louis, pp 303–312
Gerth C, Andrassi-Darida M, Bock M, Preising MN, Weber BH, Lorenz B (2002) Phenotypes of 16 Stargardt macular dystrophy/fundus flavimaculatus patients with known ABCA4 mutations and evaluation of genotype-phenotype correlation. Graefes Arch Clin Exp Ophthalmol 240:628–638
Holz FG (2001) Autofluoreszenz-Imaging der Makula. Ophthalmologe 98:10–18
Holz FG, Bellman C, Staudt S, Schütt F, Völcker HE (2001) Fundus autofluorescence and development of geographic atrophy in age-related macular degeneration. Trans Ophthalmol Soc UK 42:1051–1056
Jarc-Vidmar M, Kraut A, Hawlina M (2003) Fundus autofluorescence imaging in Best's vitelliform dystrophy. Klin Monatsbl Augenheilkd 220:861–867
Kabanarou SA, Holder GE, Bird AC, Webster AR, Stanga PE, Vickers S, Harney BA (2003) Isolated foveal retinoschisis as a cause of visual loss in young females. Br J Ophthalmol 87:801–803
Katz ML, Gao CL, Rice LM (1996) Formation of lipofuscin-like fluorophores by reaction of retinal with photoreceptor outer segments and liposomes. Mech Ageing Dev 92:159–174
Katz ML, Wendt KD, Sanders DN (2005) RPE65 gene mutation prevents development of autofluorescence in retinal pigment epithelial phagosomes. Mech Ageing Dev 126:513–521
Kennedy CJ, Rakoczy PE, Constable IJ (1995) Lipofuscin of the retinal pigment epithelium: a review. Eye 9:763–771
Lamb LE, Simon DJ (2004) A2E: a component of ocular lipofuscin. Photochem Photobiol 79:127–136
Lois N, Halfyard AS, Bunce C, Bird AC, Fitzke FW (1999) Reproducibility of fundus autofluorescence measurements obtained using a confocal scanning laser ophthalmoscope. Br J Ophthalmol 83:276–279
Lois N, Halfyard AS, Bird AC, Fitzke FW (2000) Quantitative evaluation of fundus autofluorescence imaged “in vivo” in eyes with retinal disease. Br J Ophthalmol 84:741–745
Lois N, Holder GE, Bunce C, Fitzke FW, Bird AC (2001) Phenotypic subtypes of Stargardt macular dystrophy—fundus flavimaculatus. Arch Ophthalmol 119:359–369
Lois N, Halfyard AS, Bird AC, Holder GE, Fitzke FW (2004) Fundus autofluorescence in Stargardt macular dystrophy—fundus flavimaculatus. Am J Ophthalmol 138:55–63
Lorenz B, Wabbels B, Wegscheider E, Hamel CP, Drexler W, Preising MN (2004) Lack of fundus autofluorescence to 488 nm from childhood on in patients with early onset severe retinal dystrophy (EOSRD) associated with mutations in RPE65. Ophthalmology 111:1585–1594
Mata NL, Weng J, Travis GH (2000) Biosynthesis of a major lipofuscin fluorophore in mice and humans with ABCR-mediated retinal and macular degeneration. Proc Natl Acad Sci USA 97:7154–7159
Ozdemir H, Karacorlu S, Karacorlu M (2004) Optical coherence tomography findings in familial foveal retinoschisis. Am J Ophthalmol 137:179–181
Paunescu K, Wabbels B, Preising M, Lorenz B (2004) Longitudinal and cross sectional study of patients with early onset severe retinal dystrophy (EOSRD) associated with RPE65 mutations. Graefes Arch Clin Exp Ophthalmol http://dx.doi.org/10.1007/s00417-004-1020-x
Robson AG, El Amir A, Bailey C, Egan CA, Fitzke FW, Webster AR, Bird AC, Holder GE (2003) Pattern ERG correlates of abnormal fundus autofluorescence in patients with retinitis pigmentosa and normal visual acuity. Invest Ophthalmol Vis Sci 44:3544–3550
Robson AG, Moreland JD, Pauleikhoff D, Morrissey T, Holder GE, Fitzke FW, Bird AC, Van Kuijk FJ (2003) Macular pigment density and distribution: comparison of fundus autofluorescence with minimum motion photometry. Vision Res 43:1765–1775
Robson AG, Egan CA, Luong VA, Bird AC, Holder GE, Fitzke FW (2004) Comparison of fundus autofluorescence with photopic and scotopic fine-matrix mapping in patients with retinitis pigmentosa and normal visual acuity. Invest Ophthalmol Vis Sci 45:4119–4125
Scholl HP, Chong NH, Robson AG, Holder GE, Moore AT, Bird AC (2004) Fundus autofluorescence in patients with leber congenital amaurosis. Invest Ophthalmol Vis Sci 45:2747–2752
Tantri A, Vrabec TR, Cu-Unjieng A, Frost A, Annesley WH Jr, Donoso LA (2004) X-linked retinoschisis: a clinical and molecular genetic review. Surv Ophthalmol 49:214–230
Von Rückmann A, Fitzke FW, Bird AC (1997) In vivo fundus autofluorescence in macular dystrophies. Arch Ophthalmol 115:609–615
Von Rückmann A, Schmidt KG, Fitzke FW, Bird AC, Jacobi KW (1998) Studies of the distribution of lipofuscin in the retinal pigment epithelium using high-resolution TV laser scanning ophthalmoscopy. Ophthalmologe 95:699–705
Von Rückmann A, Fitzke FW, Bird AC (1999) Distribution of pigment epithelium autofluorescence in retinal disease state recorded in vivo and its change over time. Graefes Arch Clin Exp Ophthalmol 237:1–9
Wabbels B, Preising M, Kretschmann U, Andrassi-Darida M, Demmler A, Lorenz B (2005) Genotype-phenotype correlation and longitudinal course in 10 families with Best vitelliform macular dystrophy. Br J Ophthalmol (submitted)
Wegscheider E, Preising MN, Lorenz B (2004) Fundus autofluorescence in carriers of X-linked recessive retinitis pigmentosa associated with mutations in RPGR, and correlation with electrophysiological and psychophysical data. Graefes Arch Clin Exp Ophthalmol 242:501–511
Weiter JJ, Delori FC, Wing GL, Fitch KA (1986) Retinal pigment epithelial lipofuscin and melanin and choroidal melanin in human eyes. Invest Ophthalmol Vis Sci 27:145–152
Acknowledgements
This study was supported by grants from Deutsche Forschungsgemeinschaft (DFG Lo 457/3, DFG Lo 457/5). The authors would like to thank all patients and their families for participating in the study and Karin Heinfling, Roman Miedl and Günther Schuch for AF imaging.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented in part at the 102nd Meeting of the German Ophthalmological Society (DOG)
Rights and permissions
About this article
Cite this article
Wabbels, B., Demmler, A., Paunescu, K. et al. Fundus autofluorescence in children and teenagers with hereditary retinal diseases. Graefe's Arch Clin Exp Ophthalmo 244, 36–45 (2006). https://doi.org/10.1007/s00417-005-0043-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-005-0043-2