Abstract
Background
Dry eye is a common condition, affecting approximately 10–20% of the adult population. Artificial tears are often effective in relieving symptoms in mild and moderate dry eye by replenishing deficient tear volume. Sodium hyaluronate has been proposed as a component in artificial tears, due to its viscoelastic rheology. This paper reports on a study carried out to assess the efficacy of two recently developed eyedrops containing 0.1% and 0.3% sodium hyaluronate (SH) in the treatment of moderate dry eye.
Methods
Thirteen subjects were recruited with moderate dry eye. Forty microlitres of 0.1% SH, 0.3% SH, or 0.9% saline were instilled in both eyes, and the subjects’ symptom intensity and non-invasive break-up time (NIBUT) were measured at 5, 15, 30, 45, and 60 min, and then hourly, until 6 h after drop instillation. This was repeated twice following an interval of 7(±1) days, but with a different treatment so that at the end of the final visit each subject had trialled all products. Drop allocation was randomized and double-masked.
Results
Both symptoms and NIBUT improved with all treatments. These changes were of a larger magnitude and longer duration with the SH containing eyedrops than with saline. SH of 0.3% tended to perform better than 0.1% SH and achieved statistical significance (P=0.04) for NIBUT when considered over the whole 6-h study period.
Conclusions
Sodium hyaluronate of 0.1% and 0.3% reduces symptoms of ocular irritation and lengthens NIBUT in subjects with moderate dry eye more effectively than saline, in terms of peak effect and duration of action.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dry eye is a common condition, affecting approximately 10–20% of the adult population [7]. Artificial tears are often effective in relieving symptoms in mild and moderate dry eye by replenishing deficient tear volume. Unfortunately, the low ocular residency time of watery formulations necessitates frequent instillation, whilst more viscous artificial tears blur vision and interfere with blinking.
Sodium hyaluronate (SH) is a glycosaminoglycan with a viscoelastic rheology. It consists of repeating disaccharide units of N-acetyl-D-glucosamine and sodium-D-glucuronate. Several authors have reported the use of SH in artificial tears [1, 3, 8, 9]. Between blinks its relatively high viscosity improves tear film stability and reduces washout from the ocular surface, but reduced viscosity under shear stress permits uninterrupted blinking. Additionally, SH effectively binds water and resists dehydration, and promotes epithelial wound healing [6].
This study assessed the efficacy of two commercially available eyedrops containing 0.1% and 0.3% SH in the treatment of moderate dry eye. The SH contained in these is obtained by bacterial fermentation and has a restricted molecular weight, averaging 1.6×106 Da. Both products have a pH of 7.4. The 0.1% SH drop is approximately isotonic with tears in normals (300 mOsm/l) and preserved with polyhexanide, whereas the 0.3% SH drop is relatively hypotonic (150 mOsm/l), preservative-free, and contains trace quantities of calcium, magnesium, potassium, sodium and chloride ions.
Materials and methods
Thirteen subjects (aged between 21 and 34 years, including 8 women and 5 men) with moderate dry eye were recruited from students and patients attending primary care clinics at Cardiff University (Cardiff, UK). Informed consent was obtained and the study approved by the School of Optometry and Vision Sciences' research ethics committee. Moderate dry eye was defined as symptoms of ocular irritation (soreness, scratchiness, grittiness, dryness, and/or burning) with an intensity >40 mm on a 100-mm visual analogue scale (VAS; 0 mm and 100 mm indicating no symptoms and maximum intensity respectively) and non-invasive break-up time (NIBUT) <5 s in at least one eye at a screening visit. Exclusion criteria included an intraocular difference in NIBUT >5 s; ocular disease other than moderate dry eye; severe dry eye, defined as conjunctival or limbal hyperaemia, palpebral conjunctival observations, or blepharitis, grade 4 (severe) on the EFRON grading scale [4]; abnormalities to the nasolacrimal drainage apparatus, including permanent or temporary punctal occlusion; refractive surgery within the previous 12 months; and contact lens use.
One week after the screening appointment, following basal measurements of symptom intensity and NIBUT, 40 μl of 0.1% SH (Vismed light; TRB Chemedica, Haar/Munich, Germany), 0.3% SH (Vismed gel; TRB Chemedica), or 0.9% saline (Minims; Chauvin Pharmaceuticals, Romford, Essex, UK) were instilled in both eyes by micropipette. Symptom and NIBUT measurements were taken at 5, 15, 30, 45, and 60 min, and then hourly until 6 h after drop instillation. This procedure was repeated twice following an interval of 7(±1) days, but with a different treatment so that at the end of the final visit each subject had trialled all three products. The allocation of eyedrops was randomized and instillation was performed by a person other than the observer, so that they were always masked to the treatment.
At all time points symptom intensity was quantified with a 100-mm VAS and NIBUT measured using a Tearscope Plus (Keeler, Windsor, UK). This latter apparatus consists of a circular, cold light source that projects a grid onto the tear film, which acts as a convex mirror, forming an image that can be visualized with a slitlamp biomicroscope. The time elapsing from a blink to the first detectable distortion of the grid's image is the NIBUT. Three values were recorded for each time point, and a fourth recording was taken when an obvious outlier was present.
The data were reviewed blind and analysed with S-PLUS (MathSoft, Version 4.0, Cambridge, UK) and Excel 97 (Microsoft, Redmond, WA, USA). Following data analysis it was decided that, due to the correlation between outcome and basal values, the best expression of results was the equivalent change expressed as a percentage. Baseline values for each treatment were those recorded immediately before drop instillation. Also, because the multiple NIBUT recordings at each time point frequently had a large variability, often approaching the mean, it was decided to estimate the average value by the median (generally less precise, but poorly influenced by outliers).
For both the symptom intensity and NIBUT data, an average effect was calculated for the time periods 0–1, 1–3, 3–6 and 0–6 h. This was achieved by dividing the integration of the responses (area under the curve) by the duration of the sampling interval. Time points were grouped both to reduce data variability and the number of hypothesis tests required when comparing treatments, the latter lessening the probability of a type-1 error. Parametric or non-parametric tests were used as appropriate to compare treatments with the baseline and each other.
Results and discussion
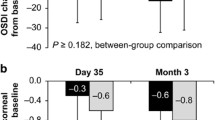
All treatments decreased symptom intensity and lengthened NIBUT from the baseline in the initial hour following their instillation (Figs. 1, 2). Over time, the efficacy of all treatments declined. During the 1–3 and 3–6-h time intervals, a statistically significant treatment effect persisted for 0.1% and 0.3% SH, but not for saline. The seemingly paradoxical finding that average NIBUT was lower in the first sampling period than in the second with 0.3% SH, was suspected by the examining investigator to reflect a limitation of NIBUT testing. This is because the NIBUT test is unable to differentiate between grid distortion secondary to tear thinning and that occurring as a result of an irregular tear surface produced by incomplete mixing of the viscous 0.3% SH drop with tears, immediately after its instillation.
Change in symptom intensity from baseline to treatment effect, expressed as a percentage of the baseline. The mean treatment effects of three sampling intervals (0–1, 0–3 and 3–6 h), quotient of area under curve and duration of interval, are shown with their 95% confidence intervals. SH sodium hyaluronate
Change in non-invasive break-up time (NIBUT) from baseline to treatment effect, expressed as a percentage of the baseline. The mean treatment effects of three sampling intervals (0–1, 0–3 and 3–6 h), quotient of area under curve and duration of interval, are shown with their 95% confidence intervals
Symptomatic relief and improvements in NIBUT with 0.1% SH and 0.3% SH were superior to saline at all sampling points. However, statistical significance was not achieved for symptoms in the last few hours of the study (Tables 1, 2). A benefit of sodium hyaluronate over saline in improving both subjective and objective measures of dry eye has been reported previously [3], and is likely in part to be due to its longer ocular residence time. It has not, however, been reported in all studies [8]. Comparing the two SH products, 0.3% SH tended to have a greater average effect on symptoms and NIBUT than 0.1% SH, but these differences only achieved statistical significance (P=0.04) when considered across the whole 6-h study period.
As noted in the introduction, the two SH-containing treatments did not only differ in the concentration of this viscoelastic. For example, the 0.1% SH drop was preserved and isotonic with tears, whereas the 0.3% SH drop was preservative-free and relatively hypotonic. It is thus possible that other properties may have accounted for the measured differences in symptoms and NIBUT.
Relatively high concentrations of polyhexanide (0.0015%) are toxic to the corneal epithelium [2], but low concentrations (0.00005%) are not [10]. The 0.1% SH treatment contained a concentration of this preservative between these values (0.00075%), and thus it is possible that its inclusion negatively influenced the tolerance of this drop. Regarding osmolarity, elevated tear osmolarity is a characteristic of dry eye and directly compromises ocular surface integrity [5]. However, the results of studies that have compared isotonic and hypotonic eyedrops for this condition are contradictory [1, 9]. It has been reasoned that the osmolarity of eyedrops has little effect on symptoms or signs because their reductions in tear osmolarity are of a short duration and that relative to the tear film in dry eye, even formulations isotonic with normal tears are hypotonic [9]. Considering the available evidence it seems likely that preservative and osmolarity differences between the treatments were of minor importance, but would have acted to decrease the effectiveness of the 0.1% SH drop and increase that of the 0.3% SH drop.
Given that the pathogenesis of dry eye syndrome is not simply desiccation, but includes ocular surface disease and inflammation [7], it is possible that greater differences between the treatments trialled would have been found after their use for several weeks. This is predicted because SH promotes wound healing [6], and the use of topical SH for several weeks has been reported to improve conjunctival morphology compared with placebo, particularly with hypotonic solutions [1].
The three treatments used in this clinical study all improved symptoms and signs of dry eye. For saline, the effects were of a low magnitude and short duration. The SH-containing products conferred both a larger and longer therapeutic action, particularly the more concentrated 0.3% SH eyedrops. These findings suggest that the two SH formulations trialled in this study will be useful in the management of dry eye.
References
Aragona P, Di Stefano G, Ferreri F, Spinella R, Stilo A (2002) Sodium hyaluronate eyedrops of different osmolarity for the treatment of dry eye in Sjogren's syndrome patients. Br J Ophthalmol 86:879–884
Begley CG, Waggoner PJ, Hafner GS, Tokarski T, Meetz RE, Wheeler WH (1991) Effect of rigid gas permeable contact lens wetting solutions on the rabbit corneal epithelium. Optom Vis Sci 68:189–197
Condon PI, McEwen CG, Wright M, Mackintosh G, Prescott RJ, McDonald C (1999) Double blind, randomised, placebo controlled, crossover, multicentre study to determine the efficacy of a 0.1% (w/v) sodium hyaluronate solution (Fermavisc) in the treatment of dry eye syndrome. Br J Ophthalmol 83:1121–1124
Efron N (1998) Grading scales for contact lens complications. Ophthalmic Physiol Opt 18:182–186
Gilbard JP, Carter JB, Sang DN, Refojo MF, Hanninen LA, Kenyon KR (1984) Morphologic effect of hyperosmolarity on rabbit corneal epithelium. Ophthalmology 91:1205–1212
Gomes JA, Amankwah R, Powell-Richards A, Dua HS (2004) Sodium hyaluronate (hyaluronic acid) promotes migration of human corneal epithelial cells in vitro. Br J Ophthalmol 88:821–825
Johnson ME, Murphy PJ (2004) Changes in the tear film and ocular surface from dry eye syndrome. Prog Retin Eye Res 23:449–474
Nepp J, Schauersberger J, Schild G, Jandrasits K, Haslinger-Akramian J, Derbolav A, Wedrich A (2001) The clinical use of viscoelastic artificial tears and sodium chloride in dry-eye syndrome. Biomaterials 22:3305–3310
Papa V, Aragona P, Russo S, Di Bella A, Russo P, Milazzo G (2001) Comparison of hypotonic and isotonic solutions containing sodium hyaluronate on the symptomatic treatment of dry eye patients. Ophthalmologica 215:124–127
Tripathi BJ, Tripathi RC, Kolli SP (1992) Cytotoxicity of ophthalmic preservatives on human corneal epithelium. Lens Eye Toxic Res 9:361–375
Acknowledgements
The authors thank Dr Vincent Baeyens and Dr Florence Mottu for their advice and support during this study. The study was sponsored by TRB Chemedica, Geneva, Switzerland. Richard Benzi (StaBioPharm, Switzerland) gave statistical advice on study design and data analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Johnson, M.E., Murphy, P.J. & Boulton, M. Effectiveness of sodium hyaluronate eyedrops in the treatment of dry eye. Graefe's Arch Clin Exp Ophthalmo 244, 109–112 (2006). https://doi.org/10.1007/s00417-005-0028-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-005-0028-1