Abstract
Background
This is a retrospective study designed to investigate the effect of pars plana vitrectomy (PPV) with internal limiting membrane (ILM) peeling on diabetic macular edema in eyes that do not have a taut hyaloid and have been refractory to standard laser treatment.
Methods
Review of 26 eyes of 20 patients consecutively were treated with PPV with ILM peel for refractory diabetic macular edema. Eyes were included if they had been unresponsive to conventional treatment defined as at least two focal laser applications by a retina specialist. Paired t-testing was performed to determine if a change in both optical coherence tomography (OCT)—measured retinal thickness and logarithm of the minimum angle of resolution (logMAR) visual acuity occurred prior to and following PPV with epiretinal membrane vitrectomy. In addition, we performed multivariate regression analysis to determine if any clinical variables predicted a change in visual acuity.
Results
The mean age in the sample was 65 years (range 29–81 years). The mean follow-up time was 242 days (range 35–939). Sixteen of the 26 eyes were phakic and the remaining ten were pseudophakic. There was a statistically significant improvement of mean visual acuity from a preoperative logMAR vision of 1.0 to a best postoperative vision of 0.75 (p=0.016, paired t-test). Thirteen (50%) of the 26 eyes gained at least two lines of best-corrected Snellen acuity, three (11.5%) had a decline of at least two lines, and ten (38.5%) showed stable visual acuity. Regression analysis demonstrated that baseline worse visual acuity was the only clinical variable that was associated with improvement in visual acuity (beta=0.602, p=0.016; R 2=28.7). Fourteen eyes had preoperative and postoperative OCT. Thirteen eyes (93%) had a significant decrease in foveal thickness; with an average preoperative thickness of 575 μm compared to a postoperative average of 311 μm (t=3.65, p=0.002). No surgical complications were observed during the follow-up period.
Conclusions
Surgery for refractory diabetic edema without a taut hyaloid is associated with a significant improvement in visual acuity and diminution of retinal thickness as measured by OCT. Further investigations are warranted to define the role of surgery in the management of persistent diabetic macular edema.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Macular edema is the most frequent cause of vision loss in patients with diabetes. The Early Treatment Diabetic Retinopathy Study showed that treatment with focal laser for clinically significant macular edema reduced the rate of moderate visual loss by 50%. However, few patients respond with improvement in vision, and up to 25% of treated patients go on to have moderate visual loss [21]. Treatment options for eyes with diffuse edema or those that have failed to improve following laser are even less likely to have improvement in vision. Grid macular photocoagulation has been the standard treatment in these eyes; however, the visual outcomes are often disappointing [7]. An alternative option is the use of vitrectomy with hyaloid removal; the utility is based on the concept that vitreous traction on the macula promotes fluid accumulation. Several studies have reported favorable outcomes with vitrectomy techniques in eyes with an obviously taut hyaloid [2, 3, 9, 11, 19, 20, 22]. Additional studies have reported more modest success with vitrectomy in eyes without hyaloidal interface abnormalities [4, 8, 13, 17, 20]. Except for one of these studies the internal limiting membrane (ILM) was not approached [2]. Gandorfer et al. evaluated the results of pars plana vitrectomy (PPV) with ILM removal in 12 eyes with diffuse edema, most of which were associated with a taut hyaloid. Eleven out of the 12 eyes had at least two lines of vision improvement. The present study was designed to help clarify whether or not eyes without an obvious taut posterior hyaloid that had failed laser treatment would benefit from vitrectomy with ILM removal. We report the functional and anatomic results of peeling the ILM in eyes with persistent, refractory diabetic edema that did not have a clinically taut hyaloid.
Methods
This study is a retrospective study of the effect of vitrectomy with ILM peel on 26 eyes of 20 consecutive patients with diabetic macular. Eyes were included in the study if they met the following criteria: (1) macular edema causing reduced visual acuity associated with diabetic retinopathy; (2) an attached posterior hyaloid without evident traction or thickening by slit lamp biomicroscopy; (3) at least two previous focal/grid laser treatments performed according to ETDRS guidelines, without significant resolution of edema and no improvement in vision after at least 6 months; (4) persistent diffuse or cystoid leakage confirmed by a recent fluorescein angiogram. If focal leakage was present, further laser rather than surgery was offered. Eyes with significant retinal pathology other than diabetic retinopathy, or prior ocular surgery other than cataract extraction were excluded. All patients had a comprehensive preoperative evaluation. This included optical coherence tomography (OCT) [(Humphrey instruments, San Leandro, CA, USA)] when available (n=14).
After obtaining informed consent, a standardized three-port PPV with indocyanine green-assisted ILM removal was performed by a single surgeon (GS). Intraoperative confirmation of an attached but normally adherent hyaloid was made in all cases. Air/fluid exchange was not performed; none of the eyes were left with air or gas. Peripheral scatter laser was performed in all cases to prevent proliferative diabetic changes. None of the eyes received intraocular steroids. Follow-up occurred at 1 day, 1 week, and 1 month postoperatively. Additional return visits depended on clinical course. At all postoperative visits a thorough ocular exam was performed that included best-corrected visual acuity (BCVA) performed by an unbiased trained technician using standard Snellen charts, applanation tonometry, and careful slit-lamp indirect biomicroscopy. At the third postoperative visit an OCT was also obtained, if available at the clinical site. The OCT was scanned with a 6 mm measurement beam oriented at intervals of 30° centered on fixation. Macular thickness, which was defined as the distance between the inner surface of the retinal pigment epithelium layer and the inner surface of the retina, was computed using OCT retinal mapping software. All computer-generated measurements were visually inspected by the authors to ensure proper calibration. Continuous and categorical variables were described in the usual statistical fashion. The logarithm of the minimum angle of resolution (logMAR) of BCVA and the retinal thickness before and after surgery was analyzed using paired t-testing. Multivariate regression analysis was performed to evaluate the effect of gender, age, phakic status, and baseline visual acuity on the change in visual acuity.
Results
Baseline characteristics, including phakic status, preoperative and postoperative visual acuity, and length of follow-up, are shown in Table 1. The average age of the patients was 65 years (range 29–81). Sixteen were phakic at the time of surgery and the remaining ten were pseudophakic. There were equal numbers of males and females. Average length of follow-up in this study was 242 days. For the purposes of statistical analysis visual acuity was converted to the logMAR equivalents. Mean preoperative logMAR vision was 0.982; there was no statistical difference in baseline visual acuity when phakic eyes were compared to those that were pseudophakic (t=1.44, df=18, p=0.167). Mean logMAR visual acuity improved to 0.75, an improvement of 0.23 units (t=2.65, df=19, p-value=0.016, 95% CI=0.049–0.419). Thirteen (50%) of the 26 eyes gained at least two lines of Snellen acuity, three (11.5%) had a decline of at least two lines, and ten (38.5%) showed stable vision. Loss of two lines of vision was attributed to cataract progression in two eyes and increased foveal lipid deposition in one eye. Our regression model demonstrated that the only factor related to the change in visual acuity was the preoperative visual acuity, worse initial vision was associated with improvement (B=0.602, p=0.016) R 2=28.7.
In the 14 eyes that had preoperative and postoperative OCT measurements, foveal thickness ranged from 425 um to 973 μm (Median 575±141 μm). The postoperative range of foveal thickness in the same group of eyes was 82–516 (median 311±116 um). The average change in thickness was 260 μm [(95% confidence interval, 126–394 um) paired t-test p=0.002] (Table 2). In 13 of the 14 eyes (93%) in which OCT was available, the central thickness was reduced postoperatively (Table 3).
There were no surgery-related complications, including endophthalmitis, vitreous hemorrhage, retinal breaks or detachments. Epiretinal membrane (ERM) formation was not observed in any eyes during the postoperative period. Six of the 16 phakic patients developed visually significant progression of cataract at latest follow-up.
Report of a case
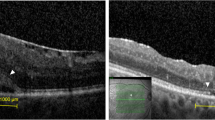
A 30-year-old male with diabetes presented with deteriorating vision in his right eye. Despite two prior laser treatments in the past his visual acuity had deteriorated to 20/400 (logMAR 1.3). Funduscopic exam revealed a markedly edematous macula with cystic changes associated with early proliferative diabetic retinal changes; neither a posterior vitreous detachment nor a thickened hyaloid was present (Fig. 1a). Fluorescein angiography demonstrated diffuse leakage of the perifoveal vasculature, without significant focal source (Fig. 1b,c). OCT was also obtained and it clearly demonstrated that the fovea was thickened to 772 μm with intraretinal cystic spaces, and there was no evidence of abnormal vitreomacular traction (Fig. 1d). The patient underwent uncomplicated PPV with ILM peel; intraoperatively the hyaloid was confirmed to be attached but not taut or thickened. Postoperatively the cystic changes resolved, fluorescein angiogram showed less leakage, and OCT measurements centered on fixation found the thickness to have decreased to 330 μm. The patient’s visual acuity in that eye improved to 20/70 (logMAR 0.54) by 9 months (Fig. 2a–d).
Color photograph (right eye). Cystic retinal thickening associated with early proliferative diabetic retinopathy in a 30-year-old patient with 20/400 vision. a Fluorescein angiogram of the same patient with early hyperfluorescence with late diffuse leakage; no obvious areas amenable to focal laser treatment are seen. Neovascularization of the disc was apparent. b,c Optical coherence tomogram (OCT) through central macula with a 6 mm scan length: marked cystic thickening without evidence of vitreomacular traction. d with a thickness of 772 um
The patient underwent uncomplicated pars plana vitrectomy with ILM peel. One month postoperatively the cystic changes resolved a, fluorescein angiogram showed less leakage b,c and OCT measurements centered on fixation found the thickness to have decreased to 330 um d; visual acuity likewise improved to 20/70 (logMAR 0.54)
Discussion
Options are limited for the treatment of eyes with diffuse diabetic edema that have failed to respond to laser photocoagulation. Vitrectomy techniques with removal of the posterior hyaloid have shown promise. In our present study, half of the eyes with macular edema gained at least two lines of visual acuity. In eyes that were followed with OCT there was an average decrease of retinal thickness by approximately 40%. None of these eyes had a taut hyaloid, a common requisite for considering surgery for macular edema. Traditional management of observation or further laser would have been unlikely to improve vision in this group of patients. Although the ETDRS showed that photocoagulation decreased the rate of moderate visual loss, only 3% had significant visual acuity improvement [21]. The efficacy of laser treatment for diffuse or refractory edema has been shown to be even more limited [1, 12, 16].
Early reports of vitrectomy techniques showed that approximately 90% of eyes with a taut hyaloid experienced visual improvement [3, 9]. Recent larger series corroborate the efficacy of vitrectomy for eyes with an abnormal hyaloid–macula interface [2, 19]. The success in this subgroup of patients is predicted by the hypothesis that the traction exerted by an attached vitreous contributes to the persistence and/or the accumulation of macular edema [14].
More modest results have been reported with vitrectomy for the treatment of eyes with an attached hyaloid that were not taut or thickened. In the two largest series of vitrectomy for this subgroup Tachi et al. and La Heij et al. reported one line of visual improvement in 31/58 (53%) and 10/21 (48%) eyes, respectively [8, 20]. In the majority of the eyes a reduction of macular edema was observed. Otani and Kishi reviewed seven patients with symmetric diabetic edema without an abnormally taut hyaloid in which one eye was randomized to vitrectomy [17]. They used OCT to demonstrate an average decrease in macular thickness of 353 μm postoperatively compared to a 60 μm average decrease in the fellow eyes. One can assume from these studies that vitrectomy is effective in decreasing the extent of macular edema in eyes with either a normal or abnormally attached hyaloid. However, the visual results are better in the latter group.
In the present study in which a taut hyaloid was not present, we anticipated that the peeling of ILM might improve the surgical outcome. Gandorfer et al. removed the ILM in 12 eyes with a taut hyaloid; in all but one eye visual acuity improved by at least two lines [2]. The results of our series in which 50% of eyes had two lines of improvement are similar to previous studies of eyes with normally attached posterior hyaloid. Investigators of macular hole repair have suggested that removing the ILM may relieve the tangential traction that helps keep a hole open; a similar mechanism may enhance the resolution of macular edema. Alternatively, the ILM may create a diffusion barrier to the efflux of fluid out of the retina or it may affect the local environment of growth factors and cytokines that influence vascular leak. Our study was not designed to prove better efficacy if ILM is removed at the time of surgery. However, in both the series by Gandorfer et al. and our study there were no cases of postoperative ERM formation. Removing the ILM at the time of vitrectomy may reduce the risk of postoperative ERM proliferation [18]. ILM appears to provide the scaffolding that permits proliferating cells to develop a membrane [6]. Previous studies that did not peel ILM reported up to a 10% rate of ERM formation [19, 20]. ERMs could contribute to recalcitrant edema and visual disability.
In line with most series of vitrectomy techniques, cataract is a common problem following surgery. For this reason we expected pseudophakic eyes to have a better visual outcome than phakic eyes. However, we found no statistically significant difference. This is likely due to the relatively limited follow-up period; we suspect with an extended time course we would see better visual acuity in the pseudophakic cohort, and given our limited sample size we had limited power to detect a clinically relevant difference.
Recently, there has been increased interest in the use of intraocular steroids for the management of diabetic edema. Small, uncontrolled series using intravitreal triamcinolone acetonide administration have been promising [5, 10]. These studies show a dramatic reduction of macular thickness and leakage with associated improvement in visual function in many patients. Although encouraging, intravitreal corticosteroids are associated with frequent elevated intraocular pressure and occasionally endophthalmitis. Currently our approach to macular edema is to perform laser photocoagulation according to ETDRS protocol for focal leakage. If laser fails to significantly resolve edema or improve vision or if there is diffuse edema, intravitreal triamcinolone is considered. Patients with contraindications to steroid depot in the vitreous, including a history of glaucoma or active ocular infection, are not offered this treatment. Surgery may be attempted in refractory cases without a posterior vitreous detachment whether or not a taut hyaloid is present.
In conclusion, our results are consistent with prior studies suggesting a role of vitrectomy for diabetic edema. Removal of the ILM may have reduced the rate of postoperative ERM formation, although this was not systematically studied in our series. OCT was found to be a useful tool in both analyzing the state of the posterior hyaloid as well as quantifying macular thickness. As with all uncontrolled retrospective studies, many biases exist, including lack of randomization, lack of controls, and lack of robust visual acuity measurement. The improvements in vitrectomy instrumentation and safety, as well as the widespread visual morbidity associated with diabetic macular edema, make it an appropriate time to pursue a randomized, prospective study, but given the varied spectrum of the disease and surgical techniques, this will be a difficult endeavor.
References
Blankenship GW (1979) Diabetic macular edema and argon laser photocoagulation: a prospective randomized study. Ophthalmology 86(1):69–78
Gandorfer A, Messmer EM, Ulbig MW et al (2000) Resolution of diabetic macular edema after surgical removal of the posterior hyaloid and the inner limiting membrane. Retina 20(2):126–133
Harbour JW, Smiddy WE, Flynn HW et al (1996) Vitrectomy for diabetic macular edema associated with a thickened and taut posterior hyaloid membrane. Am J Ophthalmol 121(4):405–413
Ikeda T, Sato K, Katano T, Hayashi Y (2000) Improved visual acuity following pars plana vitrectomy for diabetic cystoid macular edema and detached posterior hyaloid. Retina 20(2):220–222
Jonas JB, Kreissig I, Sofker A et al (2003) Intravitreal injection of triamcinolone for diffuse diabetic macular edema. Arch Ophthalmol 121:57–61
Kampik A, Green WR, Michels RG et al (1980) Ultrastructural features of progressive idiopathic epiretinal membrane removed by vitreous surgery. Am J Ophthalmol 90(6):797–809
Ladas ID, Theodossiadis GP (1993) Long-term effectiveness of modified grid laser photocoagulation for diffuse diabetic maculare dema. Acta Ophthalmol 71(3):393–397
La Heij EC, Hendrikse F, Kessels AG, Derhaag PJ (2001) Vitrectomy results in diabetic macular edema without evident vitreomacular traction. Graefes Arch Clin Exp Ophthalmol 239(4):264–270
Lewis H, Abrams GW, Blumenkranz MS, Campo RV (1992) Vitrectomy for diabetic macular traction and edema associated with posterior hyaloidal traction. Ophthalmology 99(5):753–759
Martidis A, Duker JS, Greenberg PB et al (2002) Intravitreal triamcinolone for refractory diabetic macular edema. Ophthalmology 109(5):920–927
Massin P, Duguid G, Erginay A et al (2003) Optical coherence tomography for evaluating diabetic macular edema before and after vitrectomy. Am J Ophthalmol 135(2):169–177
McDonald HR, Schatz H (1985) Grid photocoagulation for diffuse macular edema. Retina 5(2):65–72
Micelli Ferrari T, Cardascia N, Durante G et al (1999) Pars plana vitrectomy in diabetic macular edema. Doc Ophthalmol 97(3–4):471–474
Nasrallah FP, Jalkh AE, Van Coppenolle F et al (1988) The role of the vitreous in diabetic macular edema. Ophthalmology 95(10):1335–1339
Nelson ML, Tennant MT, Sivalingam A, Regillo C, Belmont JB, Martidis A (2003) Infectious and presumed noninfectious endophthalmitis after intravitreal triamcinolone acetonide injection. Retina 23(5):686–691
Olk RJ (1986) Modified grid argon (blue–green) laser photocoagulation for diffuse diabetic macular edema. Ophthalmology 93(7):938–950
Otani T, Kishi S (2000) Tomographic assessment of vitreous surgery for diabetic macular edema. Am J Ophthalmol 129(4):487–494
Park DW, Dugel PU, Garda J et al (2003) Macular pucker removal with and without internal limiting membrane peeling: pilot study. Ophthalmology 110:62–64
Pendergast SD, Hassan TS, Williams GA et al (2000) Vitrectomy for diffuse diabetic macular edema associated with a taut premacular posterior hyaloid. Am J Ophthalmol 130(2):178–186
Tachi N, Ogino N (1996) Vitrectomy for diffuse macular edema in cases of diabetic retinopathy. Am J Ophthalmol 122(2):258–260
The Early Treatment Diabetic Retinopathy Study Group (1985) Photocoagulation for diabetic macular edema. Early treatment diabetic retinopathy study report number 1. Ophthalmology 103(12):1796–1806
Yamamoto T, Akabane N, Takeuchi S (2001) Vitrectomy for diabetic macular edema: the role of posterior vitreous detachment and epimacular membrane. 132(3):369–377
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have full control of all primary data and agree to allow review of their data.
Rights and permissions
About this article
Cite this article
Rosenblatt, B.J., Shah, G.K., Sharma, S. et al. Pars plana vitrectomy with internal limiting membranectomy for refractory diabetic macular edema without a taut posterior hyaloid. Graefe's Arch Clin Exp Ophthalmol 243, 20–25 (2005). https://doi.org/10.1007/s00417-004-0958-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-004-0958-z