Abstract
Background
Cytokine levels are elevated in the ocular fluid of diabetic patients. It is unclear whether aqueous humor levels of vascular endothelial growth factor (VEGF) and interleukin-6 (IL-6) are related to the vitreous fluid levels of these substances and to the progression of diabetic retinopathy.
Methods
Aqueous humor and vitreous fluid samples were obtained during cataract and vitreous surgery from ten eyes of ten patients with diabetic macular edema and 26 eyes of 26 patients with proliferative diabetic retinopathy (PDR). The VEGF and IL-6 levels in aqueous humor, vitreous fluid, and plasma were measured by enzyme-linked immunosorbent assay.
Results
VEGF and IL-6 levels in aqueous humor were significantly correlated with those in vitreous fluid (ρ=0.793 and ρ=0.737, respectively). VEGF levels in aqueous humor and vitreous fluid were significantly correlated with the corresponding IL-6 levels (ρ=0.631 and ρ=0.687, respectively). The aqueous and vitreous levels of VEGF were significantly correlated with the severity of diabetic retinopathy (ρ=0.659 and ρ=0.771, respectively). Aqueous and vitreous levels of IL-6 were also significantly correlated with the severity of diabetic retinopathy (ρ=0.742 and ρ=0.746, respectively). Aqueous and vitreous levels of both VEGF and IL-6 were significantly higher in the patients with active PDR than those in quiescent PDR.
Conclusions
Our results suggest that there is a significant relationship between VEGF and IL-6 levels in aqueous humor and in vitreous fluid. Measurement of the aqueous levels of VEGF and IL-6 may be useful to analyze the pathogenesis of diabetic retinopathy and to predict disease activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent studies have shown that the expression of many cytokines is increased in diabetes and cytokine levels are elevated in the ocular fluid of diabetic patients [5, 6]. It has been suggested that the activity or a severity of diabetic retinopathy can be assessed by obtaining a sample of the aqueous humor or vitreous fluid at operation [2, 15]. However, surgical harvesting of vitreous fluid is associated with a risk of vitreous hemorrhage, retinal tears, and retinal detachment, while it is difficult to obtain the vitreous samples for diagnostic or investigative purpose without performing surgery. On the other hand, obtaining aqueous fluid samples is a far easier and less risky procedure. If the cytokine levels in aqueous humor reflect those in vitreous fluid, we could investigate the pathogenesis and activity of diabetic retinopathy by measuring cytokines in aqueous samples. However, it has been unclear whether the aqueous levels of substances such as vascular endothelial growth factor (VEGF) and interleukin-6 (IL-6) are related to their vitreous levels.
VEGF causes structural changes of the retinal vessels [5, 6] and plays a major role in the development of diabetic retinopathy and diabetic macular edema (DME) [5, 6]. Many of the effects of VEGF are actually mediated via other factors/cytokines and the events that induce VEGF production can initiate the release of cascade of factors, although it is still unclear how this occurs. IL-6 is a multifunctional cytokine that may indirectly cause an increase of vascular permeability and neovascularization by inducing the expression of VEGF [7], or else may directly induce an increase of endothelial permeability and new vessel formation [19]. We previously reported that the aqueous humor levels of both VEGF and IL-6 were correlated with the severity of diabetic retinopathy, the grade of fundus findings, and the severity of DME [13, 14]. VEGF and IL-6 levels in the vitreous fluid and aqueous humor may show some relationship, but are not equivalent.
The present study was performed to investigate whether the VEGF and IL-6 levels in aqueous humor were related to those in vitreous fluid and to the progression of diabetic retinopathy. We found that the aqueous levels of both VEGF and IL-6 were correlated with their vitreous levels, and also showed a strong correlation with each other. Furthermore, the aqueous humor levels of VEGF and IL-6 were correlated with not only the severity of retinopathy but also activity of retinopathy. These results suggest that measurement of cytokines and factors in the aqueous humor may be useful for predicting the activity of diabetic retinopathy.
Subjects and methods
Subjects
We obtained undiluted aqueous humor samples and corresponding plasma samples from 36 diabetic patients (36 eyes) undergoing cataract surgery. After the completion of cataract surgery, undiluted vitreous fluid samples were harvested from the same patients at the start of vitrectomy. As far as we possibly could avoid harvesting the vitreous fluid included hemorrhage when we took the vitreous samples, because VEGF is derived from the platelets. Informed consent was obtained from each subject following an explanation of the purpose and potential adverse effects of these procedures. This study was performed in accordance with the Helsinki Declaration of 1975 (1983 revision) and the institutional review board of Tokyo Women’s Medical University approved the protocol for the collection of aqueous humor, vitreous fluid, and blood samples. Samples were obtained from ten patients who had clinically significant diabetic macular edema (CSME) [9] and from 26 patients with proliferative diabetic retinopathy (PDR). The CSME patients included five with diffuse macular edema and five with cystoid macular edema (CME). The patients with PDR included 13 who had vitreous hemorrhage and 13 with tractional retinal detachment. In total, the diabetic patients comprised 18 men and 18 women aged 63.8±17.2 years (mean±SD), with duration of diabetes for 16.2±8.3 years and a hemoglobin A1c (HbA1c) of 7.8±2.2%. Exclusion criteria included (1) previous ocular surgery (2) a history of ocular inflammation (3) rubeosis iridis or rubeotic glaucoma (4) rhegmatogenous retinal detachment, and (5) intraoperative capsule breaks and dialysis. All operations were performed at Tokyo Women’s Medical University Hospital.
Fundus findings
All of the patients were evaluated by careful biomicroscopic examination using a fundus contact lens. Fundus findings were confirmed preoperatively by standardized fundus color photography and fluorescein angiography (FA), which was performed with a Topcon TRC-50IA fundus camera, an image-net system (Tokyo Optical Co Ltd., Japan), and a preset lens with a slit-lamp [13, 14]. The severity of diabetic retinopathy was graded according to the modified Early Treatment Diabetic Retinopathy Study (ETDRS) retinopathy severity scale [10, 11].
According to the ETDRS scale, three eyes were level 43, three eyes were level 47, four eyes were level 53, seven eyes were level 71, six eyes were level 75, seven eyes were level 81, and six eyes were level 85. All patients with DME and PDR underwent retinal photocoagulation before vitreous surgery, receiving a mean of 1,026 shots (range: 224–1,884 shots) and the period between the end of retinal photocoagulation and surgery was from 1 to 11 months.
Neovascularization was considered to be active if the patient had perfused, multibranching preretinal capillaries, while it was defined as quiescent if active proliferation had regressed fully or if only nonperfused, gliotic vessels and/or fibrosis was present [2, 15]. Quiescent was defined as low activity of neovascularization regardless of presence of vitreous hemorrhage and/or tractional retinal detachment and was diagnosed by intraoperative findings.
Sample collection
Samples of aqueous humor were collected into sterile tubes at the start of cataract surgery and samples of vitreous fluid were also collected into sterile tubes at the time of vitreoretinal surgery and were rapidly frozen at −80°C.
Blood samples were also collected from the 36 diabetic patients. The blood was immediately placed on ice and centrifuged at 3,000g for 5 min at 4°C, after which the plasma thus obtained was rapidly frozen and stored at −80°C until assay.
Measurement of VEGF and IL-6 levels
Both VEGF and IL-6 were measured in aqueous and vitreous samples from the same eye (as well as in plasma samples) by enzyme-linked immunosorbent assay (ELISA) using kits for human VEGF and IL-6, respectively (R&D System, Minneapolis, MN, USA) [13, 14]. The VEGF kit was able to detect two of the four VEGF isoforms (VEGF121 and VEGF165), probably because these two shorter isoforms are secreted and the two longer isoforms are cell-associated. Each assay was performed according to the manufacturer’s instructions. The standard solution (diluted 100 μl for the VEGF ELISA and 200 μl for the IL-6 ELISA) and the sample (diluted 10 or 100 μl for the VEGF ELISA and 20 or 200 μl for the IL-6 ELISA) were added to the wells of a 96-well plate coated with a monoclonal antibody. After incubation, the plate was washed, and an enzyme-labeled antibody was added. After further incubation, the plate was washed again, and the substrate was added. The reaction was arrested by adding the stop solution after color had developed, and the optical density was determined at 450 nm and 620 nm using an absorption spectrophotometer (Titertek Multiscan MCC/340; ICN. Tokyo, Japan). A standard curve was plotted from measurements made with the standard solution (from 15.6 to 1,000 pg/ml for VEGF and from 0.156 to 100 pg/ml for IL-6) and was used to determine the concentration of VEGF or IL-6 in each sample. The levels of these substances in vitreous fluid, aqueous humor, and plasma were within the detection range of the relevant assay, with the minimum detectable concentration being 15.6 pg/ml for VEGF (the intra-assay coefficient of variation (CV) was 5.5% and the inter-assay CV was 6.8%) and 0.156 pg/ml for IL-6 (intra-assay CV of 5.6% and inter-assay CV of 6.9%).
Statistical analysis
All analyses were performed with SAS System software (ver. 8.2; SAS Institute Inc., Cary, North Carolina, USA) [22]. Data are presented as frequencies or as the mean ± SD. Data with a skewed distribution were initially transformed to a logarithmic scale, and the geometric mean was calculated together with the 1-SD range on either side of the mean. To examine correlations, Spearman’s rank correlation coefficients were calculated by linear regression analysis. The Mann–Whitney U-test was used to compare VEGF and IL-6 levels between active and quiescent PDR. A two-tailed p-value of less than 0.05 was considered to indicate statistical significance.
Results
Aqueous and vitreous levels of VEGF and IL-6
The aqueous humor level of VEGF (243.3 pg/ml [28.2–1,088.4]) was significantly correlated with the vitreous fluid level of VEGF (986.3 pg/ml [58.1–3,684.6]) (ρ=0.793, p<0.0001) (Fig. 1a). The aqueous level of IL-6 (78.4 pg/ml [11.2–382.4]) was also significantly correlated with the vitreous level of IL-6 (203.0 pg/ml [23.6–592.4]) (ρ=0.737, p<0.0001) (Fig. 1b). Aqueous levels of VEGF were significantly correlated with those of IL-6 (ρ=0.631, p<0.0001), and vitreous levels of VEGF were also significantly correlated with those of IL-6 (ρ=0.687, p<0.0001).
Aqueous, vitreous, and plasma levels of VEGF and IL-6
The aqueous humor level of VEGF was significantly higher than the plasma level (46.8 pg/ml [15.6–285.6]) (p<0.0001) and the aqueous level of IL-6 was also significantly higher than its plasma level (13.9 pg/ml [3.8–41.8]) (p=0.0098). The vitreous fluid level of VEGF was significantly higher than its plasma level (p<0.0001), as was the vitreous fluid level of IL-6 (p=0.0178). There was no significant relationship between HbA1c (7.6% [4.8–12.3]) and the vitreous levels of VEGF or IL-6 (ρ=0.220, p=0.1712 and ρ=0.253, p=0.0626, respectively).
Relationship with the activity of retinopathy and cytokines
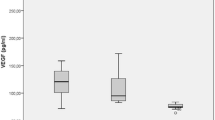
The aqueous humor level of VEGF was significantly correlated with the severity of diabetic retinopathy (ρ=0.659, p<0.0001), and the vitreous fluid level of VEGF was also significantly correlated with the severity of retinopathy (ρ=0.771, p<0.0001) (Fig. 2a). Furthermore, the aqueous level of IL-6 was significantly correlated with the severity of diabetic retinopathy (ρ=0.744, p<0.0001), as was the vitreous level of IL-6 (ρ=0.746, p<0.0001) (Fig. 2b).
a Correlation between the severity of diabetic retinopathy and the aqueous and vitreous levels of VEGF. The VEGF levels in aqueous humor and vitreous fluid were both significantly correlated with the severity of diabetic retinopathy (ρ=0.659, p<0.0001; ρ=0.771, p<0.0001, respectively). Open circle, aqueous levels of VEGF; filled circle, vitreous level of VEGF. b Correlation between the severity of diabetic retinopathy and the aqueous and vitreous levels of IL-6. The IL-6 levels in aqueous humor and vitreous fluid were also both significantly correlated with the severity of diabetic retinopathy (ρ=0.744, p<0.0001; ρ=0.746, p<0.0001, respectively). Open circle, aqueous level of IL-6; closed circle, vitreous level of VEGF IL-6
In the patients with active PDR, aqueous levels of both VEGF and IL-6 (VEGF: 376.5 pg/ml (182.7–1,072.6)); IL-6: 277.8 pg/ml (76.6–492.3)) were significantly higher (p=0.0298 and p=0.0475, respectively) than in the patients with quiescent PDR (VEGF: 212.2 pg/ml (128.3–692.5)); IL-6: 154.3 pg/ml (62.4–412.6)) (Table 1). In the patients with active PDR, vitreous levels of both VEGF and IL-6 (VEGF: 1849.5 pg/ml (845.3–3,042.6)); IL-6: 617.2 pg/ml (271.7–918.1)) were also significantly higher (p=0.0089 and p=0.0134, respectively) than in the patients with quiescent PDR (VEGF: 1,234.8 pg/ml (784.4–2,087.3)); IL-6: 415.9 pg ml (169.6–823.5)).
Discussion
In the present study, we obtained the aqueous humor and vitreous fluid samples from the same patients at their operations and measured the levels of VEGF (which induces an increase of vascular permeability and angiogenesis) and IL-6 (a proinflammatory cytokine) in patients with diabetes. We hypothesized that the aqueous levels of both VEGF and IL-6 might be correlated with their vitreous levels and with the severity or activity of diabetic retinopathy. Our present findings and previous results showed that not only the vitreous levels of VEGF and IL-6, but also the aqueous levels of these two substances, were correlated with the severity of diabetic retinopathy, the grade of fundus findings, and the severity of DME [1, 2, 13–15]. Aiello et al. [2] reported that a vitreous-to-aqueous gradient promotes the anterior diffusion of VEGF, potentially accounting for the occurrence of anterior segment neovascularization in association with retinal ischemia. However, it has been unclear whether the aqueous levels of VEGF and IL-6 reflect their vitreous levels. In the present study, we simultaneously measured cytokine levels in the aqueous humor and vitreous fluid, and we excluded patients with rubeosis iridis and rubeotic glaucoma, because the aqueous levels of VEGF and IL-6 are markedly elevated in these conditions. We also excluded patients who had the complications such as intraoperative capsule breaks and dialysis during cataract surgery and long duration (over 20 min) of cataract surgery, because the complications and long period of cataract surgery has the possible of influence for the vitreous levels of VEGF and IL-6. It is easier and less risky to obtain aqueous samples, and our findings suggested that there is gradient-driven diffusion of angiogenic factors from the posterior to the anterior segment of the eye, since VEGF and IL-6 levels were always higher in the vitreous fluid than in the aqueous humor. This gradient may be due to the rapid clearance of VEGF and IL-6 from the anterior chamber or their more rapid degradation in that chamber [2]. Our results suggested that the VEGF and IL-6 levels in aqueous humor reflect those in vitreous fluid, but further investigation will be needed to confirm this, because the number of samples tested in the present study was not large enough.
We found that the aqueous and vitreous levels of VEGF and IL-6 were correlated with each other. In addition, the aqueous and vitreous levels of VEGF and IL-6 were higher than the plasma levels of both substances. Numerous cytokines and other factors have been suggested to have a role in the pathogenesis and progression of diabetic retinopathy, and it has been postulated that cytokines in the ocular fluid may also be involved in diabetic retinopathy [1, 2, 13–15]. Lip et al. reported that raised plasma level of VEGF was related to PDR and there was significant reduction in plasma levels at 4 months’ follow-up after pan-retinal photocoagulation [16]. However, they did not compare between the vitreous and/or aqueous levels of VEGF and plasma level of that. It was reported that the high vitreous levels of VEGF observed in diabetic patients with PDR cannot be attributed to serum diffusion across the blood-retinal barrier [4]. Our results and previous reports [2, 4, 13–15] suggest that the vitreous and/or aqueous levels of VEGF have more influence than plasma levels of that. Further investigation is needed to be clear whether plasma levels of VEGF or IL-6 affect the progression of diabetic retinopathy.
VEGF has been localized in numerous retinal cells including Müller cells, astrocytes, pericytes, vascular endothelial cells, and retinal pigment epithelial cells [18]. IL-6 is synthesized by a variety of cells, such as macrophages, fibroblasts, epidermal cells, vascular endothelial cells, and vascular smooth muscles [17]. Within the eye, the sources of IL-6 include the retinal pigment epithelial cells, corneal epithelial cells, keratocytes, iris, and ciliary body [8, 12]. Hyperglycemia has been established as the primary factor in the development and progression of diabetic retinopathy. Several interacting and mutually perpetuating abnormal biochemical pathways may lead to the promotion of VEGF and IL-6 expression [5, 6]. Our previous studies have suggested that expression of VEGF and IL-6 is increased in the eyes of patients with diabetes [13, 14]. Recently, Cohen and associates reported that IL-6 might induce angiogenesis indirectly via the induction of VEGF expression [7]. Because the production of both VEGF and IL-6 is known to be upregulated by ischemia, advanced glycation end-products, protein kinase Cβ, and insulin-like growth factor-1 (IGF-1) [3, 20, 21, 24], it seems likely that changes of other cytokines might also promote the expression of VEGF and IL-6. These cytokines are presumed to form a network that influences the progression and activity of diabetic retinopathy.
It seems reasonable for the vitreous fluid levels of VEGF and IL-6 to vary with the severity of PDR [1, 2, 15]. In fact, we found that not only the vitreous levels of both VEGF and IL-6, but also their aqueous levels were significantly higher in patients with active PDR than in patients with quiescent PDR. The levels of both VEGF and IL-6 in the aqueous and vitreous appear to increase during active neovascularization, because we classified PDR as active or quiescent according to the activity of neovascularization. It was previously reported that the vitreous level of VEGF was higher in active PDR than in quiescent PDR and that VEGF plays a major role in mediating intraocular neovascularization in diabetic retinopathy [2, 15]. Also, the vitreous levels of IL-6 were positively correlated with the clinical grade of ocular disease in patients with PDR [1]. However, to our knowledge, the present study has provided the first evidence that aqueous humor levels of VEGF and IL-6 are elevated in the active stage of PDR. Although our results suggested that the measurement of VEGF or IL-6 levels in aqueous samples may be clinically useful to predict the progression of diabetic retinopathy because the aqueous levels of these substances reflect the activity of PDR, further investigation will be needed to confirm this.
The underlying biochemical cause of diabetic retinopathy appears to be chronic hyperglycemia. Therefore, we suspected that the HbA1c level might show a correlation with the VEGF level in the aqueous humor and/or vitreous fluid, but no significant relationship was found. Likewise, IL-6 levels in the aqueous humor and/or vitreous fluid showed no significant relationship with HbA1c. Because some patients underwent tightening of glycemic control before surgery, the HbA1c level at the time of operation may not necessarily have indicated their long-term glycemic control, making it difficult to assess the relationship between hyperglycemia and VEGF or IL-6.
In conclusion, we found that both the VEGF and IL-6 levels in aqueous humor were significantly correlated with the levels of these substances in vitreous fluid. In addition, the aqueous levels of VEGF and IL-6 were significantly correlated with the severity of diabetic retinopathy and with the activity of PDR. These findings suggest that the levels of cytokine or other factors in aqueous humor may reflect those in vitreous fluid, so that measurement of the aqueous levels of these substances may be useful to predict the activity of PDR and the outcome of vitreous surgery.
References
Abu El Asrar AM, Maimone D, Morse PH et al (1992) Cytokines in the vitreous of patients with proliferative diabetic retinopathy. Am J Ophthalmol 114:731–736
Aiello LP, Avery RL, Arrigg PG et al (1994) Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med 331:1480–1487
Aiello LP, Bursell SE, Clermont A et al (1997) Vascular endothelial growth factor-induced retinal permeability is mediated by protein kinase C in vivo and suppressed by an orally effective B-isoform-selective inhibitor. Diabetes 46:1473–1480
Burgos R, Simo R, Audi L et al (1997) Vitreous levels of vascular endothelial growth factor are not influenced by its serum concentrations in diabetic retinopathy. Diabetologia 40:1107–1109
Cai J, Boulton M (2002) The pathogenesis of diabetic retinopathy. Old concepts and new questions. Eye 16:242–260
Chakrbarti S, Cukiernik M, Hleeto D et al (2002) Role of vasoactive factors in the pathogenesis of early changes in diabetic retinopathy. Diabetes Metab Res Rev 16:393–407
Cohen T, Nahari D, Cerem LW et al (1996) Interleukin 6 induces the expression of vascular endothelial growth factor. J Biol Chem 271:736–741
Cubitt CL, Lausch RN, Oakes JE (1995) Differences in interleukin-6 gene expression between cultured human corneal epithelial cells and keratocytes. Invest Ophthalmol Vis Sci 36:330–336
Early Treatment Diabetic Retinopathy Study Research Group (1985) Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report 1. Arch Ophthalmol 103:1796–1806
Early Treatment Diabetic Retinopathy Study Research Group (1991) Grading diabetic retinopathy from stereoscopic color fundus photographs. An extension of the modified Airlie House classification. ETDRS Report Number 10. Ophthalmology 98:786–806
Early Treatment Diabetic Retinopathy Study Research Group (1991) Fundus photographic risk factors for progression of diabetic retinopathy. ETDRS Report Number 12. Ophthalmology 98:823–833
Elner VM, Scales W, Elner SG et al (1992) Interleukin-6 (IL-6) gene expression and secretion by cytokine-stimulated human retinal epithelium cells. Exp Eye Res 54:361–368
Funatsu H, Yamashita H, Shimizu E et al (2001) Relationship between vascular endothelial growth factor and interleukin-6 in diabetic retinopathy. Retina 21:469–477
Funatsu H, Yamashita H, Noma H et al (2002) Increased levels of vascular endothelial growth factor and interleukin-6 in the aqueous humor of diabetic macular edema. Am J Ophthalmol 133:70–77
Katsura Y, Okano T, Noritake M et al (1998) Hepatocyte growth factor in vitreous fluid of patients with proliferative diabetic retinopathy and other retinal disorders. Diabetes Care 21:1759–1763
Lip PL, Belgore F, Blann AD et al (2000) Plasma VEGF and soluble VEGF receptor Flt-1 in proliferative retinopathy: Relationship to endothelial dysfunction and laser treatment. Invest Ophthalmol Vis Sci 41:2115–2119
Lotz M (1995) Interleukin-6. A comprehensive review. Cancer Treat Res 80:209–233
Lutty GA, McLeod S, Merges C et al (1996) Localization of vascular endothelial growth factor in human retina and choroid. Arch Ophthalmol 114:971–977
Maruo N, Morita I, Shirao M, Murota S (1992) IL-6 increases endothelial permeability in vitro. Endocrinology 131:710–714
Morohoshi M, Fujisawa K, Uchimura I, Numano F (1996) Glucose-dependent interleukin 6 and tumor necrosis factor production by human peripheral blood monocytes in vitro. Diabetes 45:954–959
Punglia RS, Lu M, Hsu J et al (1997) Regulation of vascular endothelial growth factor expression by insulin-like growth factor. Diabetes 46:1619–1626
SAS Institute Inc (1997) SAS/STAT Software. Changes and Enhancements through. Release 6.12., Cary, NC, USA, 1–1167
Scheiki D, Itin A, Soffer D, Keshet E (1992) Vascular endothelial growth factor induced by hypoxia may mediate hypoxia-initiated angiogenesis. Nature 359:843–845
Yan SF, Tritto I, Pinsky D et al (1995) Induction of interleukin-6 (IL-6) by hypoxia in vascular cells. J Biol Chem 270:11463–11471
Acknowledgments
We thank Drs Shigehiko Kitano, Erika Shimizu, Yuichiro Nakanishi, Koji Makita, and Kensuke Haruyama for their assistance in collecting the vitreous and plasma samples and in performing the ophthalmological examinations. We also thank Drs Yasuhiko Iwamoto and Naoko Iwasaki for their assistance in performing the internal medical examinations. Finally, we would like to thank Katsunori Shimada (Department of Biostatistics, STATZ Institute, Co., Ltd) for his assistance in conducting the statistical analysis. Supported by a Health Science Research Grant (#10060101 to Drs Funatsu, Hori, and Yamashita) from the Japanese Ministry of Health, Labor and Welfare (Tokyo, Japan).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Funatsu, H., Yamashita, H., Noma, H. et al. Aqueous humor levels of cytokines are related to vitreous levels and progression of diabetic retinopathy in diabetic patients. Graefe's Arch Clin Exp Ophthalmol 243, 3–8 (2005). https://doi.org/10.1007/s00417-004-0950-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-004-0950-7