Abstract
Growth factors (GF) are important in several stages of the pathogenesis of age-related macular disease (AMD). In choroidal neovascularization (CNV) in exudative AMD, the GF involved are similar to those involved in wound healing of the skin. Like granulation tissue of skin, CNV is characterized by clotting, inflammation, angiogenesis and fibrosis, and like in skin wounds, members of the VEGF, angiopoietin, PDGF and TGF-β families of GF are expressed. However, several of these GF may also serve physiological functions in the normal eye, where the retinal pigment epithelium (RPE) employs them to provide trophic support to the neuroretina and choriocapillaris, in addition to maintaining an anti-angiogenic state. Derangement of these physiological functions may underlie the initiation of CNV in AMD. Basolateral secretion of VEGF-A by the RPE maintains the choriocapillaris, and is enhanced by hypoxia. Age-related changes in Bruch’s membrane lead to impairment of this trophic function and choriocapillaris atrophy, as well as to decreased diffusion of oxygen towards the neuroretina. The resulting outer retina hypoxia may be an important driving force of CNV formation, by stimulating VEGF overexpression by the RPE, in addition to the effects of increased oxidative stress and low-grade inflammation. RPE senescence and hypoxia may also decrease expression of angiogenesis inhibitors such as PEDF, further shifting the balance to a pro-angiogenic state in the aging eye.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Age-related macular disease (AMD) [8] often causes loss of vision in the elderly. A better understanding of the pathogenesis of this complex disease is needed in order to develop better preventive and interventional treatment strategies. Such strategies may be directed at the array of growth factors that have been shown to be involved in the development of AMD.
Growth factors, neurotrophic factors, chemokines and cytokines (GF) are cell-secreted mediators of autocrine and paracrine functions, involved in cell maintenance, survival, growth and death, as well as in angiogenesis, vascular permeability, inflammation and other processes [37, 69]. Most GF were originally thought to have single functions in one of these processes, but often, their functional potential has broadened. An example is vascular endothelial growth factor-A (VEGF-A), which was originally described as a vascular permeability factor, then identified as being important in angiogenesis, whilst recent work has highlighted the roles of VEGF as a mediator of leukocyte adhesion in vascular cells and as a neurotrophic factor in the central nervous system [11, 70].
Inhibition of VEGF in exudative AMD has recently been reported to benefit patients [63], confirming experimental evidence that GF cause choroidal neovascularization (CNV). However, angiogenesis inhibition alone will not be sufficient to restore the function of a macula affected by AMD, as in addition to CNV, the clinical and pathological spectrum of AMD shows a variety of changes. These range from drusen deposition and pigment epithelium detachments to scar formation [8]. Increased oxidative stress has been identified as a central mechanism in AMD pathogenesis [7].
Many GF have been implied in AMD, mainly based on experimental data obtained from studies in cultured retinal pigment epithelium (RPE) and from histopathological studies in surgically removed human CNV or in laser-induced CNV in transgenic rodent models [16, 21, 50]. These studies have identified the RPE not only as an important source of growth factors involved in tissue maintenance, homeostasis, inflammation and CNV formation, but also as the central cell type acting in and regulating these processes [7, 9, 21].
These considerations are especially relevant for the scientific field that tries to explore transplantation of the RPE as a therapeutic approach in AMD. The purpose of this review is to provide an overview of our present knowledge of the role of GF and the RPE in AMD.
Growth factors and wound healing: the angiogenic balance
Histological studies show that CNV represents wound healing tissue quite similar to the granulation tissue (GT) of skin wounds [19, 20]. The role of GF in wound healing has been most extensively studied in such skin wounds and genuine granulation tissue. The enormous number of GF shown to be involved in this process (Table 1) and their highly complex interactions have been excellently reviewed elsewhere [37, 69]. The wound healing response in skin is characterized by inflammation, angiogenesis and fibrosis and serves to restore the integrity of the tissue. Distinct phases and a number of key processes are recognized, including (blood) clotting, formation of a provisional fibrin matrix, infiltration by neutrophils and macrophages, angiogenesis, extracellular matrix formation, scarring and reepithelialization [69]. By histology, distinct zones can be recognized in human GT, consisting of an outer fibrin layer, a superficial layer with abundant vascular sprouting, an intermediate layer with vascular maturation and extensive matrix formation, and a deep layer characterized by fibrosis [56]. In addition to monocytes, circulating cells such as fibrocytes and endothelial progenitor cells may also contribute to the formation of granulation tissue [1, 58, 69]. Initially, these invading cells and platelets are a main source of growth factors, but later in GT development, GF production by macrophages, (myo)fibroblasts, endothelial cells, pericytes and keratinocytes becomes more important [69]. The exact temporal and spatial involvement of all these GF in GT formation has only been partly elucidated (Table 1) [69]. In GT angiogenesis, members of the VEGF family, released by macrophages and platelets are considered important in the initial migration and proliferation stages of vascular and lymphatic growth. PDGF-BB produced by endothelial cells helps to recruit pericytes, and angiopoietin-1 produced by pericytes acts on endothelial cells through its receptor Tie-2 to form stable mature vessels (Fig. 1) [37]. It has been suggested that in resting tissues many potent angiogenesis factors such as FGFs and VEGFs are present, but that these are counteracted by constitutive expression of angiogenesis inhibitors such as thrombospondins. This angiogenic balance would initially swing towards angiogenesis during GT formation and would be restored after termination of the wound healing response [15, 28, 69].
Experimental models for AMD research
How does CNV in AMD compare to skin wound healing? AMD research typically lacks adequate models allowing investigation of the different stages of the disease. Cultures of human RPE cells have been used extensively. In interpreting results of these studies, it is important to realize that RPE cells have the potential to transdifferentiate into a wound healing phenotype, expressing functions completely different from the highly differentiated non-dividing RPE cells within their monolayer in the normal eye [25, 74]. Tissue culture conditions are likely to provide an environment inducing this wound healing phenotype. By specific measures, RPE cells in vitro can be made to differentiate into a phenotype resembling RPE in vivo, displaying polarity, a columnar morphology, the presence of gap or even tight junctions, and the presence of microvilli at their apical surface [9, 46, 74]. Unfortunately, many publications fail to describe the differentiation state of the studied RPE cells, rendering the findings of these studies often useless. RPE cells may be cultured on filter systems, allowing evaluation of polarized GF secretion, or in co-culture systems with choriocapillaris (CC) endothelial cells or neuroretinal explants [9]. Exposing the cells to substances relevant to the pathogenesis of AMD, such as rod outer segments (ROS) or advanced glycation end products (AGE), provides ways to investigate mechanisms involved in AMD, such as lipofuscin formation and oxidative stress [7].
Recent work has identified transgenic mouse models with retinal changes such as basal linear deposits, reminiscent of human non-exudative age-related maculopathy, and these models may teach us more about the contribution to AMD of mechanisms like oxidative stress [4, 51]. Transgenic mice which lack or overexpress a specific GF gene, in particular in a specific tissue or under a conditional control system, are also useful in investigating which GF are involved in CNV formation. Such models can be combined with the laser CNV model, which has also been applied in rats and monkeys, where local destruction of the RPE and Bruch’s membrane by laser causes a CNV-like response [50, 65]. This response can be semi-quantified and be studied by immunohistochemistry, by in situ hybridization, or by PCR mRNA analysis of the CNV tissue isolated with laser capture dissection [50]. Finally, several studies have investigated GF expression and cellular content of surgically removed human CNV.
The RPE in embryonic development
What can we learn in AMD research from the normal eye and its development? In ocular development, the choroid forms from two embryonic tissues, the mesoderm and the cranial neural crest cells. All cells in the choroid derive from neural crest cells except for the endothelial cells. The pattern of development suggests that interactions between the primordial RPE and the periocular mesenchyme are important, and in line with this notion it was shown that in the absence of an RPE layer, the choroid does not develop [73]. High expression of VEGF in the embryonic RPE, and of its receptors VEGFR-1 and -2 in the periocular mesenchyme, in particular in a layer of cells adjacent to the RPE, has been demonstrated [71, 73]. In human eyes as wells as in rats and mice, VEGF mRNA levels in RPE cells in vivo have their peak expression during the embryonic stage of development of the choroid, but expression persists into adulthood [71, 72, 73]. This suggests that VEGF is one of the factors involved in choroidal development driven by the embryonic RPE, a paracrine relation that may persist throughout life to maintain the CC. In vitro, RPE cells are particularly sensitive for hypoxia-induced VEGF overexpression [2, 60]. Choroidal development via VEGF expression in embryonic RPE may therefore be driven by hypoxia, resulting from retinal thickening and the high oxygen demand of the developing photoreceptors.
Growth factors and the RPE in the normal eye
Clinical and experimental observations suggest that also in the normal adult eye, the RPE cell layer is crucial for maintenance and survival of both the neuroretina and the choroid (reviewed in [70]). Destruction of the RPE by laser invariably leads to atrophy of the CC and photoreceptors. This is also supported by the finding that experimental destruction of RPE cells causes atrophy of the CC, which is preceded by loss of fenestrations of the CC endothelium [69, 70]. Experimental data show that GF are involved in this physiological function of the RPE and its interactions with the retinal cells and CC. One function of the RPE may be to lend trophic support to the retina by production of neurotrophic GF such as nerve growth factor (NGF), brain-derived growth factor (BDNF) [29] and pigment epithelium-derived factor (PEDF) [29, 30]. BDNF may also promote differentiation of the RPE itself in an autocrine manner [22]. PEDF, a 50-kDa secreted glycoprotein, is an important neurotrophic factor for retinal cells [30] produced by the resting RPE. In vitro, PEDF is mainly produced by highly differentiated RPE cells [45]. In addition to its neurotrophic properties, PEDF is a potent inhibitor of angiogenesis [13]. PEDF may contribute to maintaining the angiogenic balance in ocular tissues, as it is downregulated in human and experimental conditions with ocular neovascularization, such as proliferative retinopathy and exudative AMD [26, 45, 54]. Thrombospondin-1 (TSP-1) is another potent angiogenesis inhibitor, produced by RPE cells in vitro and demonstrated by immunohistochemistry in resting RPE in vivo [43], that the RPE employs to maintain an anti-angiogenic state in the resting choroid. A similar role has been suggested for members of the TGF-β family [42].
In addition to these angiogenesis inhibitors, the resting RPE has been convincingly shown to produce the pro-angiogenic VEGF-A, both in vivo and in vitro. In vitro, VEGF production is considerably higher in differentiated than in undifferentiated RPE cells, a finding that supports a physiological role of VEGF-A [9, 45]. In vitro, VEGF secretion by highly differentiated RPE cells was shown to be directed preferentially towards the basal side of the cells [9], whilst in vivo in the adult human choroid, the VEGF receptors 1, 2 and 3 are expressed by the CC endothelium on its side facing the RPE cells [9]. As VEGF can act as a survival factor for endothelial cells [3], and as it induces a fenestrated permeable endothelial phenotype [14], these findings indicate that VEGF-A is involved in the physiological maintenance function of the resting RPE on the choroid [9]. Expression of VEGFR-3, a ligand for VEGF-C and -D but not for VEGF-A, in the human CC in vivo [9, 70], together with the recently demonstrated constitutive expression of placenta growth factor (PlGF) in mouse choroid [50], suggests involvement of other members of the VEGF family in this function as well. In addition to this role of GF, it was shown in an in vitro model that the extracellular matrix deposited by cultured RPE cells, and the presence of basic fibroblast growth factor (bFGF) within this matrix, may also contribute to CC survival by inhibition of endothelial apoptosis [38]. The presence in the choroid of potent angiogenesis inhibitors such as PEDF and TSP-1 may counteract the angiogenic effects of VEGFs and bFGF on the CC.
In differentiated RPE cells in vitro, VEGF-A upregulates PEDF expression via VEGFR-1 in an autocrine manner [46]. Although this observation suggests complex interactions between these pro- and anti-angiogenic factors to maintain tissue homeostasis in the normal human retina, expression of VEGF receptors by human RPE in vivo has not yet been convincingly demonstrated [9, 73]. Finally, RPE cells in vitro also secrete angiopoietin (Ang)-1 and -2 [23]. These GF have been implied in the later stages of angiogenesis, acting in stabilizing and remodeling of newly formed vessels (Fig. 1) [64]. Ang-1 is produced by perivascular cells and the receptor for Ang-1 and -2, Tie2, is constitutively expressed by endothelial cells, suggesting a role of angiopoietins in normal vascular function such as regulation of permeability (reviewed in [64]). In cultured RPE cells, Ang-1 and -2 were found to be expressed and VEGF-A was shown to upregulate Ang-1 secretion by these cells in an autocrine manner [23]. As these cultured RPE cells were of unspecified differentiation it remains unknown whether Ang-1/Tie2 interactions are involved in CC homeostasis in the resting eye.
Taking the published findings together, in the normal eye complex GF networks are employed by the RPE to play a central role in supporting the surrounding tissues and maintaining an anti-angiogenic state.
Pathology of CNV and cell types involved
CNV in conditions other than AMD is usually of the classic type as seen by fluorescein angiography (FA), anatomically corresponding to fibrovascular tissue growing between the retina and RPE (Figs. 2, 3 and 5). In AMD, several types of CNV are recognized [18], and their pathogenesis may be different. By FA, most cases have occult CNV, a situation where the neovascular activity is primarily located between the RPE and Bruch’s membrane [35, 36]. In the course of time, the overlying RPE cells migrate into these lesions or degenerate, and the membrane may proceed in growing directly under the neuroretina. Other cases initially only have classical membranes or demonstrate both types of CNV in an early stage of the disease. In AMD, the arrest of growth of CNV, by the RPE or by other mechanisms, seems to fail. This leads to continuing growth of the lesion, far beyond meaningful wound healing, and the eventual scar may take up a large portion of the posterior pole. In addition, there are specific age-related subtypes of CNV such as polypoidal choroidal vasculopathy and retinal angiomatous proliferations (RAP). Whether different GF are involved in these various types of CNV is unknown. It is likely, however, that once CNV is developing, an array of GF expression and function occurs that is shared by wound healing elsewhere [17,20]. The histological key components of the wound healing and GT response, i.e., inflammation, angiogenesis (Fig. 2) and fibrosis, and the corresponding cell types, i.e., macrophages, newly formed vessels and (myo)fibroblasts, have all been demonstrated in human and rodent CNV in histopathological studies [17,21]. In experimental rodent CNV, systemic macrophage depletion reduced the size of the lesions, indicating the important role of these cells in CNV formation [55]. The clinical heterogeneity and variable degree of eventual subretinal fibrosis in human CNV are likely to reflect a variable contribution of the histological key components of GT to the evolution of CNV. By histology, some authors distinguish inflammatory from non-inflammatory CNV [21], differences that probably reflect the stage of evolution of the wound healing response. Some CNV membranes are associated with hemorrhage, and this will not only introduce GF derived from platelets and leukocytes, but will also expand the provisional fibrin matrix, which may in itself stimulate further vascular growth. In the absence of hemorrhage, human CNV in its classic form is also associated with a front of fibrin [36], visible on fluorescein angiography (FA) as a hypofluorescent rim around the hyperfluorescent leaky membrane (Figs. 2 and 3). Behind this fibrin layer, FA often shows a front of actively growing, highly leaky vascular sprouts (Figs. 2 and 3), developing into less leaky vessels in the center of the lesion (Fig. 3). These characteristics are reminiscent of the layered structure and growth patterns of GT in skin wounds.
Clinicopathological correlation of idiopathic CNV. Note in A the hypofluorescent rim surrounding the hyperfluorescence of the leaking membrane which probably represents a front of fibrin. The arrow points at a complex of neovascular sprouts which can also be recognized in the histological specimen (B). Note in B the numerous small endothelial extensions typical of actively sprouting capillaries invading the fibrin matrix (asterisks)
Stages in development of CNV, reminiscent of the layered structure of granulation tissue in skin wound healing. Note from top to bottom the hypofluorescent peripheral rim of fibrin (Fi), the actively leaking front of growing vessels (L), the central part of the lesion characterized by less leaky, maturing vessels (asterisk), and an area with fibrosis (Fibr). H indicates hemorrhage
Growth factors in human and experimental CNV
It is not surprising that within established CNV membranes, many of the GF known to be involved in skin GT have been demonstrated (Table 1) [5, 21, 53]. How these GF contribute to the different stages of evolution of CNV is largely unknown. A specific characteristic differentiating CNV from wound healing elsewhere is the presence of RPE cells in various degrees of transdifferentiation [17, 19]. In patients with a retinal detachment, such transdifferentiated RPE cells are known to cause proliferative vitreoretinopathy (PVR), another ocular wound healing condition. In PVR, involvement of a number of GF has been implied, including hepatocyte growth factor/scatter factor (HGF), PDGF-B, TNF, TGF-β and connective tissue growth factor (CTGF) [25]. The involvement and relative contribution of these factors to CNV formation needs to be determined. RPE cells within CNV membranes were shown to express, among other things, monocyte chemotactic protein (MCP) [21], a molecule involved in macrophage recruitment, and members of the VEGF and angiopoietin families of GF [23, 34, 39]. The VEGF family consists of several GF acting on three types of receptors. VEGFs have important and varying roles in vascular permeability, angiogenesis and lymphangiogenesis and have neurotrophic and pro-inflammatory functions (reviewed in [70]). In migrating RPE cells and macrophages in human and experimental CNV membranes, VEGF-A, -B, -C and -D, PlGF and VEGFR-1 (Flt1) and -2 (Flk1) have been demonstrated at the protein and mRNA levels [16, 34, 39, 48, 50, 68]. In murine CNV, the smallest isoform of VEGF-A, VEGF-A120, was the main type of VEGF-A expressed [50]. These observations have led to (pre)clinical studies of VEGF-A inhibition in patients with CNV [63]. In some of these patients and in preclinical models partial regression of CNV lesions was observed, and this has confirmed that VEGF-A has an important role in CNV growth [33, 63]. Experimental studies in rodents have thrown some light on the relative contribution of VEGFs to this process. Overexpression of VEGF-A in the RPE or in photoreceptors by viral transfection leads to CNV formation, but only if some form of local trauma is induced [57, 62]. In the absence of trauma, VEGF-A overexpression in the RPE causes increased choroidal vascular permeability and leukocyte adhesion [57]. Studies in VEGF-A knockout mice are not possible, as these animals are not viable. However, PlGF knockout mice develop normally, but the loss of PlGF inhibits pathologically increased permeability and angiogenesis in cancer and retinal ischemia in these mice [40]. It has been suggested that PlGF, through interaction with its receptor VEGFR-1, specifically enables survival of newly formed vessels [59]. This mechanism may operate in CNV development, as experimental CNV lesions induced by laser in PlGF knockout mice were smaller than in wild-type controls [50]. In addition to VEGFs, the two main members of the angiopoietin family of GF, Ang-1 and Ang-2, were also demonstrated at the protein level in human CNV tissue in migrating RPE cells, suggesting involvement of these GF in vascular maturation, stabilization and remodeling in CNV [23, 47]. Recently, expression of CTGF in human CNV was reported [24]. CTGF is a pro-fibrotic factor also capable of inducing angiogenesis [61]. Which of these functions is important in CNV development needs to be determined.
Role of the RPE in the pathogenesis of CNV
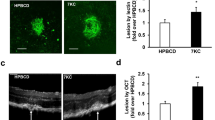
Ascertaining why CNV starts growing in AMD is one of the main challenges in this field of research. CNV can occur in a large number of ocular conditions. In most of these, there is some kind of defect in Bruch’s membrane in the presence of a viable retina, accompanied by a variable degree of inflammation [49]. The defect in Bruch’s membrane may be clinically visible, as in pigmentary changes and atrophy in AMD, chorioretinal scars, traumatic choroidal ruptures, angioid streaks or myopic lacquer cracks. Increased oxidative stress is an important mechanism in the pathogenesis of AMD [7], reviewed elsewhere in the January 2004 issue of this journal. Increased oxidative stress is likely to lead to overexpression of GF by the RPE and a pro-inflammatory state, causing invasion of macrophages resulting in local destruction of Bruch’s membrane [7, 49]. Indeed, macrophages have been demonstrated along the outer side of Bruch’s membrane in eyes with drusen [21], possibly attracted by RPE-derived MCP [21]. However, hypoxia may play a role in the development of CNV as well [12]. Based on our findings in the normal eye we have suggested a possible scenario for the pathogenesis of CNV in AMD (Fig. 4) [9]. As previously discussed, RPE cells in the normal eye predominantly secrete VEGF-A at their basolateral side, towards the CC, maintaining the CC and inducing its fenestrated permeable phenotype. In vitro, hypoxia markedly increases VEGF-A secretion by RPE cells at their basolateral side [9]. Thus, the maintenance function of the RPE on the CC may be characterized by a hypoxia-driven feedback mechanism. It is tempting to speculate that in aging, but in AMD in particular, this paracrine relation is disturbed by a thickened Bruch’s membrane, which is less permeable to water-soluble compounds such as VEGFs due to the accumulation of lipids (reviewed in [8]). Because of these changes in Bruch’s membrane, VEGF-A may not be able to reach the CC in order to support it. This would result in CC atrophy, which has indeed been observed in aging eyes [41, 52], and hypoxia of the outer retina. Outer retina hypoxia may be further enhanced by decreased diffusion of oxygen from the choroid to the RPE and retina, caused by the age-related changes in Bruch’s membrane [8, 10, 27]. This is supported by recent studies indicating decreased diffusion of ethanol, a molecule only slightly larger than oxygen, through Bruch’s membrane in eyes with AMD [6].
Schematic representation of the possible role of VEGF and hypoxia in the pathogenesis of CNV in AMD. In the normal retina, VEGF secreted by the RPE to its basal side maintains the choriocapillaris (A). In aging, thickening of Bruch’s membrane inhibits diffusion of VEGF and oxygen, leading to choriocapillaris atrophy and outer retina hypoxia (B). Hypoxia causes VEGF upregulation and accumulation, leading eventually to neovascularization through localized defects in Bruch’s membrane (C)
Thus, the aging changes in Bruch’s membrane may cause hypoxia in the outer retina from CC atrophy and decreased oxygen diffusion [8]. The RPE will respond with increased basal secretion of VEGF [9], which will accumulate due to the barrier properties of the thickened, lipid-laden Bruch’s membrane [27]. In the presence of localized defects in Bruch’s membrane, caused by atrophy or activity of macrophages [49], CNV may be initiated by these accumulations of high amounts of VEGF (Fig. 4). Histopathological and experimental observations support this concept: immunostaining of VEGF-A is increased in and around the RPE in the macula of patients with age-related maculopathy, a condition with a high risk of developing CNV [32]. Experimental overexpression of VEGF-A by the RPE, in the presence of a surgical trauma, induces CNV [12, 62]. Based on this scheme of events, CNV may have some functional significance in AMD, as it provides the hypoxic tissues with a new blood supply. Selective therapeutic destruction of CNV, as is done with photodynamic therapy (PDT), may therefore increase the stimulus for neovascularization, a pattern indeed suggested by the clinical course of some PDT-treated patients.
As described above, VEGF-A is secreted by the resting RPE. In addition, VEGF-A, PlGF and all three VEGF receptors were demonstrated in the normal choroid and neuroretina, suggesting not only (possibly neurotrophic) physiological functions of VEGFs in the eye, but also the necessary presence of mechanisms counteracting the pro-angiogenic and permeability effects of these GF. Thus, other biochemical factors, such as oxidative stress or a decrease in angiogenesis inhibitors, and anatomical factors, such as damage to Bruch’s membrane, must occur to allow the development of CNV. In this respect a role of PEDF in CNV pathogenesis has been suggested [44, 45]. In the vitreous of patients with neovascular AMD, PEDF is decreased [26]. In the rat model of laser-induced CNV, where VEGF-A protein is strongly upregulated, it was shown that expression of PEDF is decreased in cells within CNV tissue [54]. In contrast, in a later stage, PEDF was strongly expressed in RPE cells sealing the CNV, suggesting that PEDF secreted by the RPE cells is involved in regression of CNV.
Thus, the RPE probably initiates the CNV response, but may also be involved in its arrest. Encapsulation of the fibrovascular membrane by a monolayer of RPE cells, comparable to reepithelialization in skin wounds, is observed in histopathological studies [66] and can often be seen clinically in young patients with CNV (Fig. 5). In CNV tissue, FasL, an apoptotic molecule, is expressed in the RPE cells and may control angiogenesis beneath the retina. The growing vascular endothelial cells in CNV express the apoptosis-signaling receptor Fas and are sensitive to Fas-mediated cell death [31]. Therefore, in addition to a role of PEDF, FasL expression from the RPE may attenuate CNV by killing the Fas-sensitive vascular endothelial cells in the vicinity [31].
Growth factors and RPE transplantation
The goal of RPE transplantation is to restore sight in patients with AMD. It is intended to lead to a new monolayer of highly differentiated, fully functional RPE cells, resting on a (provisional) Bruch’s membrane, and a CC. Experimental approaches in RPE transplantation have ranged from applying cell suspensions to using autologous sheets of RPE with the underlying Bruch’s membrane [67]. Considering the potential of RPE cells to change rapidly into a wound healing cell, the latter approach seems desirable. RPE cells in a suspension, detached from their basement membrane, are likely to produce unwanted GF at the site of transplantation, a wound bed by itself, and decrease their anti-angiogenic and trophic functions. In contrast, autologous RPE sheets with the Bruch’s membrane still intact may allow the cells to maintain their differentiation and physiological functions and preserve the associated anti-angiogenic state.
Conclusions
Growth factors are crucial in AMD. This role of GF may start as early as in embryonic development, when the choroid develops in the vicinity of the fetal RPE [73]. The mechanisms by which the RPE induces choroid formation, and the factors that attract the massive number of capillaries developing into the CC, may have a related role in adult life [9]. In aging, these mechanisms may fail or become deranged and contribute to the development of disease. An additional role of the RPE lies in control of local inflammation, and inflammation is likely to play a role in the sequence of events leading to CNV [19, 20]. The main physiological function of CNV may be to rapidly restore the integrity of the ocular wall, rather than preserve sight, and this may be the reason for the significant collateral damage to visual function inflicted by CNV. Once established, CNV formation runs an independent course, like GT formation in skin wounds. In AMD, this course is expanded by failure of inhibitory mechanisms. Several of the main GF involved in CNV formation also have important functions in the normal healthy eye, and this may have implications for therapeutic approaches aimed at CNV.
References
Abe R, Donnelly SC, Peng T, Bucala R, Metz CN (2001) Peripheral blood fibrocytes: differentiation pathway and migration to wound sites. J Immunol 166:7556–7562
Aiello LP, Northrup JM, Keyt BA, Takagi H, Iwamoto MA (1995) Hypoxic regulation of vascular endothelial growth factor in retinal cells. Arch Ophthalmol 113:1538–1544
Alon T, Hemo I, Itin A, Pe’er J, Stone J, Keshet E (1995) Vascular endothelial growth factor acts as a survival factor for newly formed retinal vessels and has implications for retinopathy of prematurity. Nat Med 1:1024–1028
Ambati J, Anand A, Fernandez S, Sakurai E, Lynn BC, Kuziel WA, Rollins BJ, Ambati BK (2003) An animal model of age-related macular degeneration in senescent Ccl-2- or Ccr-2-deficient mice. Nat Med 9:1390–1397
Amin R, Puklin JE, Frank RN (1994) Growth factor localization in choroidal neovascular membranes of age-related macular degeneration. Invest Ophthalmol Vis Sci 35:3178–3188
Arden GB, Wolf JE (2003) Differential effects of light and alcohol on the electro-oculographic responses of patients with age-related macular disease. Invest Ophthalmol Vis Sci 44:3226–3232
Beatty S, Koh H, Phil M, Henson D, Boulton M (2000) The role of oxidative stress in the pathogenesis of age-related macular degeneration. Surv Ophthalmol 45:115–134
Bird AC (2003) The Bowman lecture. Towards an understanding of age-related macular disease. Eye 17:457–466
Blaauwgeers HG, Holtkamp GM, Rutten H, Witmer AN, Koolwijk P, Partanen TA, Alitalo K, Kroon ME, Kijlstra A, van Hinsbergh VW, Schlingemann RO (1999) Polarized vascular endothelial growth factor secretion by human retinal pigment epithelium and localization of vascular endothelial growth factor receptors on the inner choriocapillaris. Evidence for a trophic paracrine relation. Am J Pathol 155:421–428
Campochiaro PA (2000) Retinal and choroidal neovascularization. J Cell Physiol 184:301–310
Carmeliet P, Storkebaum E (2002) Vascular and neuronal effects of VEGF in the nervous system: implications for neurological disorders. Semin Cell Dev Biol 13:39–53
D’Amore PA (1994) Mechanisms of retinal and choroidal neovascularization. Invest Ophthalmol Vis Sci 35:3974–3979
Dawson DW, Volpert OV, Gillis P, Crawford SE, Xu H, Benedict W, Bouck NP (9–7-1999) Pigment epithelium-derived factor: a potent inhibitor of angiogenesis. Science 285:245–248
Esser S, Wolburg K, Wolburg H, Breier G, Kurzchalia T, Risau W (1998) Vascular endothelial growth factor induces endothelial fenestrations in vitro. J Cell Biol 140:947–959
Folkman J (1997) Angiogenesis and angiogenesis inhibition: an overview. EXS 79:1-8
Frank RN (1997) Growth factors in age-related macular degeneration: pathogenic and therapeutic implications. Ophthalmic Res 29:341–353
Green WR (1991) Clinicopathologic studies of treated choroidal neovascular membranes. A review and report of two cases. Retina 11:328–356
Green WR, Enger C (1993) Age-related macular degeneration histopathologic studies. The 1992 Lorenz E. Zimmerman Lecture. Ophthalmology 100:1519–1535
Grossniklaus HE, Green WR (1998) Histopathologic and ultrastructural findings of surgically excised choroidal neovascularization. Submacular Surgery Trials Research Group. Arch Ophthalmol 116:745–749
Grossniklaus HE, Martinez JA, Brown VB, Lambert HM, Sternberg P, Jr., Capone A, Jr., Aaberg TM, Lopez PF (1992) Immunohistochemical and histochemical properties of surgically excised subretinal neovascular membranes in age-related macular degeneration. Am J Ophthalmol 114:464–472
Grossniklaus HE, Ling JX, Wallace TM, Dithmar S, Lawson DH, Cohen C, Elner VM, Elner SG, Sternberg P, Jr. (2002) Macrophage and retinal pigment epithelium expression of angiogenic cytokines in choroidal neovascularization. Mol Vis 8:119–126
Hackett SF, Friedman Z, Freund J, Schoenfeld C, Curtis R, DiStefano PS, Campochiaro PA (1998) A splice variant of trkB and brain-derived neurotrophic factor are co-expressed in retinal pigmented epithelial cells and promote differentiated characteristics. Brain Res 789:201–212
Hangai M, Murata T, Miyawaki N, Spee C, Lim JI, He S, Hinton DR, Ryan SJ (2001) Angiopoietin-1 upregulation by vascular endothelial growth factor in human retinal pigment epithelial cells. Invest Ophthalmol Vis Sci 42:1617–1625
He S, Jin ML, Worpel V, Hinton DR (2003) A role for connective tissue growth factor in the pathogenesis of choroidal neovascularization. Arch Ophthalmol 121:1283–1288
Hinton DR, He S, Jin ML, Barron E, Ryan SJ (2002) Novel growth factors involved in the pathogenesis of proliferative vitreoretinopathy. Eye 16:422–428
Holekamp NM, Bouck N, Volpert O (2002) Pigment epithelium-derived factor is deficient in the vitreous of patients with choroidal neovascularization due to age-related macular degeneration. Am J Ophthalmol 134:220–227
Holz FG, Sheraidah G, Pauleikhoff D, Bird AC (1994) Analysis of lipid deposits extracted from human macular and peripheral Bruch’s membrane. Arch Ophthalmol 112:402–406
Iruela-Arispe ML, Dvorak HF (1997) Angiogenesis: a dynamic balance of stimulators and inhibitors. [Review]. Thromb Haemost 78:672–677
Ishida K, Yoshimura N, Yoshida M, Honda Y, Murase K, Hayashi K (1997) Expression of neurotrophic factors in cultured human retinal pigment epithelial cells. Curr Eye Res 16:96–101
Jablonski MM, Tombran-Tink J, Mrazek DA, Iannaccone A (2000) Pigment epithelium-derived factor supports normal development of photoreceptor neurons and opsin expression after retinal pigment epithelium removal. J Neurosci 20:7149–7157
Kaplan HJ, Leibole MA, Tezel T, Ferguson TA (1999) Fas ligand (CD95 ligand) controls angiogenesis beneath the retina. Nat Med 5:292–297
Kliffen M, Sharma HS, Mooy CM, Kerkvliet S, de Jong PT (1997) Increased expression of angiogenic growth factors in age-related maculopathy. Br J Ophthalmol 81:154–162
Krzystolik MG, Afshari MA, Adamis AP, Gaudreault J, Gragoudas ES, Michaud NA, Li W, Connolly E, O’Neill CA, Miller JW (2002) Prevention of experimental choroidal neovascularization with intravitreal anti-vascular endothelial growth factor antibody fragment. Arch Ophthalmol 120:338–346
Kvanta A, Algvere PV, Berglin L, Seregard S (1996) Subfoveal fibrovascular membranes in age-related macular degeneration express vascular endothelial growth factor. Invest Ophthalmol Vis Sci 37:1929–1934
Lafaut BA (2000) Clinicopathologic correlation of surgically removed submacular tissue. Bull Soc Belge Ophtalmol 278: 49–53
Lafaut BA, Bartz-Schmidt KU, Vanden Broecke C, Aisenbrey S, De Laey JJ, Heimann K (2000) Clinicopathological correlation in exudative age related macular degeneration: histological differentiation between classic and occult choroidal neovascularisation. Br J Ophthalmol 84:239–243
Li J, Zhang YP, Kirsner RS (2003) Angiogenesis in wound repair: angiogenic growth factors and the extracellular matrix. Microsc Res Tech 60:107–114
Liu X, Ye X, Yanoff M, Li W (1997) Extracellular matrix of retinal pigment epithelium regulates choriocapillaris endothelial survival in vitro. Exp Eye Res 65:117–126
Lopez PF, Sippy BD, Lambert HM, Thach AB, Hinton DR (1996) Transdifferentiated retinal pigment epithelial cells are immunoreactive for vascular endothelial growth factor in surgically excised age-related macular degeneration-related choroidal neovascular membranes. Invest Ophthalmol Vis Sci 37:855–868
Luttun A, Tjwa M, Carmeliet P (2002) Placental growth factor (PlGF) and its receptor Flt-1 (VEGFR-1): novel therapeutic targets for angiogenic disorders. Ann N Y Acad Sci 979:80–93
Lutty G, Grunwald J, Majji AB, Uyama M, Yoneya S (1999) Changes in choriocapillaris and retinal pigment epithelium in age-related macular degeneration. Mol Vis 5:35
Mathura JR, Jr., Jafari N, Chang JT, Hackett SF, Wahlin KJ, Della NG, Okamoto N, Zack DJ, Campochiaro PA (2000) Bone morphogenetic proteins-2 and −4: negative growth regulators in adult retinal pigmented epithelium. Invest Ophthalmol Vis Sci 41:592–600
Miyajima-Uchida H, Hayashi H, Beppu R, Kuroki M, Fukami M, Arakawa F, Tomita Y, Kuroki M, Oshima K (2000) Production and accumulation of thrombospondin-1 in human retinal pigment epithelial cells. Invest Ophthalmol Vis Sci 41:561–567
Ogata N, Wada M, Otsuji T, Jo N, Tombran-Tink J, Matsumura M (2002) Expression of pigment epithelium-derived factor in normal adult rat eye and experimental choroidal neovascularization. Invest Ophthalmol Vis Sci 43:1168–1175
Ohno-Matsui K, Morita I, Tombran-Tink J, Mrazek D, Onodera M, Uetama T, Hayano M, Murota SI, Mochizuki M (2001) Novel mechanism for age-related macular degeneration: an equilibrium shift between the angiogenesis factors VEGF and PEDF. J Cell Physiol 189:323–333
Ohno-Matsui K, Yoshida T, Uetama T, Mochizuki M, Morita I (2003) Vascular endothelial growth factor upregulates pigment epithelium-derived factor expression via VEGFR-1 in human retinal pigment epithelial cells. Biochem Biophys Res Commun 303:962–967
Otani A, Takagi H, Oh H, Koyama S, Matsumura M, Honda Y (1999) Expressions of angiopoietins and Tie2 in human choroidal neovascular membranes. Invest Ophthalmol Vis Sci 40:1912–1920
Otani A, Takagi H, Oh H, Koyama S, Ogura Y, Matumura M, Honda Y (2002) Vascular endothelial growth factor family and receptor expression in human choroidal neovascular membranes. Microvasc Res 64:162–169
Penfold PL, Madigan MC, Gillies MC, Provis JM (2001) Immunological and aetiological aspects of macular degeneration. Prog Retin Eye Res 20:385–414
Rakic JM, Lambert V, Devy L, Luttun A, Carmeliet P, Claes C, Nguyen L, Foidart JM, Noel A, Munaut C (2003) Placental growth factor, a member of the VEGF family, contributes to the development of choroidal neovascularization. Invest Ophthalmol Vis Sci 44:3186–3193
Rakoczy PE, Zhang D, Robertson T, Barnett NL, Papadimitriou J, Constable IJ, Lai CM (2002) Progressive age-related changes similar to age-related macular degeneration in a transgenic mouse model. Am J Pathol 161:1515–1524
Ramrattan RS, van der Schaft TL, Mooy CM, de Bruijn WC, Mulder PG, de Jong PT (1994) Morphometric analysis of Bruch’s membrane, the choriocapillaris, and the choroid in aging. Invest Ophthalmol Vis Sci 35:2857–2864
Reddy VM, Zamora RL, Kaplan HJ (1995) Distribution of growth factors in subfoveal neovascular membranes in age-related macular degeneration and presumed ocular histoplasmosis syndrome. Am J Ophthalmol 120:291–301
Renno RZ, Youssri AI, Michaud N, Gragoudas ES, Miller JW (2002) Expression of pigment epithelium-derived factor in experimental choroidal neovascularization. Invest Ophthalmol Vis Sci 43:1574–1580
Sakurai E, Anand A, Ambati BK, van Rooijen N, Ambati J (2003) Macrophage depletion inhibits experimental choroidal neovascularization. Invest Ophthalmol Vis Sci 44:3578–3585
Schlingemann RO, Rietveld FJ, Kwaspen F, van de Kerkhof PC, et al (1991) Differential expression of markers for endothelial cells, pericytes, and basal lamina in the microvasculature of tumors and granulation tissue. Am J Pathol 138:1335–1347
Schwesinger C, Yee C, Rohan RM, Joussen AM, Fernandez A, Meyer TN, Poulaki V, Ma JJ, Redmond TM, Liu S, Adamis AP, D’Amato RJ (2001) Intrachoroidal neovascularization in transgenic mice overexpressing vascular endothelial growth factor in the retinal pigment epithelium. Am J Pathol 158:1161–1172
Sengupta N, Caballero S, Mames RN, Butler JM, Scott EW, Grant MB (2003) The role of adult bone marrow-derived stem cells in choroidal neovascularization. Invest Ophthalmol Vis Sci 44:4908–4913
Shih SC, Ju M, Liu N, Smith LE (2003) Selective stimulation of VEGFR-1 prevents oxygen-induced retinal vascular degeneration in retinopathy of prematurity. J Clin Invest 112:50–57
Shima DT, Adamis AP, Ferrara N, Yeo KT, Yeo TK, Allende R, Folkman J, D’Amore PA (1995) Hypoxic induction of endothelial cell growth factors in retinal cells: identification and characterization of vascular endothelial growth factor (VEGF) as the mitogen. Mol Med 1:182–193
Shimo T, Nakanishi T, Nishida T, Asano M, Kanyama M, Kuboki T, Tamatani T, Tezuka K, Takemura M, Matsumura T, Takigawa M (1999) Connective tissue growth factor induces the proliferation, migration, and tube formation of vascular endothelial cells in vitro, and angiogenesis in vivo. J Biochem (Tokyo) 126:137–145
Spilsbury K, Garrett KL, Shen WY, Constable IJ, Rakoczy PE (2000) Overexpression of vascular endothelial growth factor (VEGF) in the retinal pigment epithelium leads to the development of choroidal neovascularization. Am J Pathol 157:135–144
The Eyetech Study Group (2003) Anti-vascular endothelial growth factor therapy for subfoveal choroidal neovascularization secondary to age-related macular degeneration: phase II study results. Ophthalmology 110:979–986
Thurston G (2003) Role of angiopoietins and Tie receptor tyrosine kinases in angiogenesis and lymphangiogenesis. Cell Tissue Res (in press)
Tobe T, Takahashi K, Ohkuma H, Uyama M (1994) [Experimental choroidal neovascularization in the rat]. Nippon Ganka Gakkai Zasshi 98:837–845
Uyama M (1991) [Choroidal neovascularization, experimental and clinical study]. Nippon Ganka Gakkai Zasshi 95:1145–1180
van Meurs JC, Van Den Biesen PR (2003) Autologous retinal pigment epithelium and choroid translocation in patients with exudative age-related macular degeneration: short-term follow-up. Am J Ophthalmol 136:688–695
Wada M, Ogata N, Otsuji T, Uyama M (1999) Expression of vascular endothelial growth factor and its receptor (KDR/flk-1) mRNA in experimental choroidal neovascularization. Curr Eye Res 18:203–213
Werner S, Grose R (2003) Regulation of wound healing by growth factors and cytokines. Physiol Rev 83:835–870
Witmer AN, Vrensen GF, Van Noorden CJ, Schlingemann RO (2003) Vascular endothelial growth factors and angiogenesis in eye disease. Prog Retin Eye Res 22:1-29
Yi X, Mai LC, Uyama M, Yew DT (1998) Time-course expression of vascular endothelial growth factor as related to the development of the retinochoroidal vasculature in rats. Exp Brain Res 118:155–160
Zhao J, Song Y, Wang Y, Zhang X (2000) [Regulation effect of vascular endothelial growth factor on human fetal choroid vascularization]. Yan Ke Xue Bao 16:11–14
Zhao S, Overbeek PA (2001) Regulation of choroid development by the retinal pigment epithelium. Mol Vis 7:277–282
Zhao S, Rizzolo LJ, Barnstable CJ (1997) Differentiation and transdifferentiation of the retinal pigment epithelium. Int Rev Cytol 171:225–266
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schlingemann, R.O. Role of growth factors and the wound healing response in age-related macular degeneration. Graefe's Arch Clin Exp Ophthalmol 242, 91–101 (2004). https://doi.org/10.1007/s00417-003-0828-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-003-0828-0