Abstract
Background
The ANO5 gene encodes for anoctamin-5, a chloride channel involved in muscle cell membrane repair. Recessive mutations in ANO5 are associated with muscular diseases termed anoctaminopathies, which are characterized by proximal or distal weakness, or isolated hyperCKemia. We present the largest series of patients with asymptomatic/paucisymptomatic anoctaminopathy reported so far, highlighting their clinical and radiological characteristics.
Methods
Twenty subjects were recruited retrospectively from the Neuromuscular Disorders Units database of two national reference centers. All had a confirmed genetic diagnosis (mean age of diagnosis was 48 years) established between 2015 and 2019. Clinical and complementary data were evaluated through clinical records.
Results
None of the patients complained about weakness or showed abnormal muscular balance. Among paucisymptomatic patients, the main complaints or findings were generalized myalgia, exercise intolerance and calf hypertrophy, occasionally associated with calf pain. All patients showed persistent hyperCKemia, ranging from mild-moderate to severe. Muscle biopsy revealed inflammatory changes in three cases. Muscle magnetic resonance imaging revealed typical signs (preferential involvement of adductor and gastrocnemius muscles) in all but one patient. In two cases, abnormal findings were detectable only in STIR sequences (not in T1). Three patients showed radiological progression despite remaining asymptomatic. Twelve different mutations in ANO5 were detected, of which seven are novel.
Conclusions
Recessive mutations in ANO5 are a frequent cause of undiagnosed asymptomatic/paucisymptomatic hyperCKemia. Patients with an apparent indolent phenotype may show muscle involvement in complementary tests (muscle biopsy and imaging), which may progress over time. Awareness of anoctaminopathy as the cause of nonspecific muscular complaints or of isolated hyperCKemia is essential to correctly diagnose affected patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ANO5 gene encodes for anoctamin-5, a calcium-activated chloride channel involved in muscle cell membrane fusion and repair processes [1]. Dominant mutations in ANO5 are associated with gnathodiaphyseal dysplasia, whereas recessive mutations have been described in several muscular diseases, termed anoctaminopathies, presenting with predominantly proximal or distal weakness (limb-girdle muscular dystrophy 12 [LGMDR12] or Miyoshi-like muscular dystrophy 3 [MMD3], respectively) [2]. Recent progress in next-generation sequencing (NGS) techniques has uncovered that mutations in ANO5 known to cause progressive muscular dystrophy can also cause isolated hyperCKemia (elevated levels of creatine kinase [CK]), which is occasionally associated with mild symptoms such as exercise intolerance or myalgia [1, 3]. It is not yet known, however, whether this is an early stage of the muscular dystrophy phenotype or whether it represents the mildest end of the spectrum of anoctaminopathies [1].
No clear genotype–phenotype correlations have so far been described for ANO5 mutations. Indeed, patients with different phenotypes have similar biopsy and magnetic resonance imaging (MRI) features, with medial gastrocnemius involvement in different radiological examinations being an outstanding characteristic of these disorders [1, 4, 5]. MRI can, nevertheless, be potentially useful in the initial differential diagnosis to distinguish ANO5-related muscular diseases from other genetic myopathies [5].
In the present study, we summarize the clinical, pathological and radiological features of 20 adult patients with recessive mutations in ANO5 and with hyperCKemia without overt clinical weakness, despite a long period of disease evolution. We also include a radiological follow-up of five patients and describe seven novel ANO5 mutations related to this disease.
Methods
Patients and data
We report a series of 20 adult patients with asymptomatic or mildly symptomatic hyperCKemia with pathogenic mutations in ANO5 (NM_213599.2). The study subjects were recruited retrospectively from the Neuromuscular Disorders Unit database of two tertiary hospitals (Hospital Universitario 12 de Octubre, Madrid and Hospital Universitari I Politècnic La Fe, Valencia), which act as National Reference Centers of rare neuromuscular diseases in Spain. The centers followed 14 and 13 ANO5 patients (irrespective of clinical phenotype) with genetic diagnosis established between 2015 and 2019. Of the 27 ANO5 patients, 20 were evaluated because of asymptomatic or mildly symptomatic hyperCKemia without fixed weakness and were included in the present study. According to the Ethics Committee requirements, written informed consent was obtained from all patients allowing clinical data publication for scientific purposes. Clinical and complementary data were assessed through clinical records and are shown in Table 1.
Regarding complementary studies, CK levels were determined on several occasions from the first presentation, and the range of values was recorded for each patient. Seventeen of the 20 patients were investigated with electromyography. Also, a muscle MRI protocol using a 1.5 T MRI system, including T1-weighted and short tau inversion recovery (STIR) sequences, was performed in all but one patient. Details of the STIR sequence were available for nine patients, and five patients had sequential MRI assessments performed after an interval of 3–5 years. Muscle biopsies were obtained from all but one patient and were processed for routine histochemical and immunohistochemical analyses.
NGS was performed at both participating hospitals: the first reference center used a custom amplicon-based targeted gene panel covering 59 genes known to be associated with muscular dystrophies and myopathies (Ion-PGM Platform; Thermo Fisher Scientific, Carlsbad, CA, USA) [6]; the second reference center used a custom amplicon-based targeted gene panel covering 40 genes known to be associated with muscular dystrophies and myopathies (Ion-Torrent Platform). All variants detected were confirmed by Sanger Sequencing. The pathogenicity of novel variants was assessed following the American College of Medical Genetics and Genomics (ACGM) consensus criteria for the interpretation of sequence variants [7].
Results
Clinical features
Twenty patients were analyzed retrospectively (12 men, 8 women) (Table 1). The mean age at first detection of hyperCKemia was 39 years (range 13–66) and the mean age at genetic diagnosis of anoctaminopathy was 48 years (range 27–69). None of the cases had evidence of previously normal CK levels. The average time from the first detection of high CK levels to data analysis was 8.85 years (range 0–24). Only three patients reported a history of statin intake.
All 20 patients showed elevated levels of liver aspartate and alanine aminotransferase. Details of the liver enzyme alterations were available for all but one patient. Ten of the 20 patients (50%) showed increases in the hepatic aminotransferases without evidence of a liver disorder for many years before the detection of hyperCKemia.
None of the patients complained of weakness and all had a normal muscular balance on examination. Of the patients presenting with mildly symptomatic hyperCKemia (13/20), five complained of generalized myalgia (25%), five of exercise-induced myalgia (25%), one of nonspecific fatigue (5%), and two of calf pain (10%) with concomitant moderate calf hypertrophy (Fig. 1). Six other patients had calf hypertrophy without calf pain, giving a total of eight patients with this sign in our cohort (40%). Those patients with exercise intolerance were initially evaluated for suspected metabolic myopathy.
All patients showed some degree of hyperCKemia, ranging from mild–moderate to severe (range 250–15,000 UI/l). Electromyography was performed in 17 patients. Electromyography was normal in ten patients (10/17, 59%), whereas six patients (6/17, 35%) had a myopathic pattern and one patient had a neurogenic pattern (1/17, 6%). Results of muscle biopsy, obtained from all but one patient, were normal in four patients (4/19, 21%), whereas six patients had nonspecific myopathic signs (6/19, 31%), four patients had minimum regenerative and/or necrotic changes (4/19, 21%), two patients had mitochondrial or dystrophic signs (2/19, 11%), and three patients had inflammatory changes (3/19, 16%). Of the latter three patients, two had only slight signs of inflammation (isolated inflammatory focus) whereas the other patient had a prominent inflammatory infiltrate in the muscle biopsy with positivity for HLA class I (MHC-I) immunostaining (Fig. 2), which was initially interpreted as polymyositis.
Muscle biopsy. Hematoxylin and eosin (H&E) staining of muscle biopsies from patient 1 (a) and 20 (d) showing slight regenerative changes and an isolated necrotic fiber. H&E staining of muscle biopsy from patient 7 showing a small inflammatory focus (b) and a negative staining for HLA class I (MHC-I) (e). Muscle biopsy of patient 2 showing prominent inflammation in H&E staining (c) and a positive HLA staining (f)
Imaging results
Typical muscle MRI findings associated with ANO5 mutations include an asymmetric and preferential involvement of adductor muscles in the thigh and/or gastrocnemius muscles in the leg. Of the 19 patients subjected to MRI, all but one patient (95%) showed these typical changes at some point along the follow-up. For the one patient with no evidence of radiological muscle changes, only a thigh MRI was available; thus, an involvement of lower leg muscles could not be ruled out.
A detailed analysis of STIR MRI sequences was available for nine patients (data summarized in Table 2). Pathological imaging findings were observed in eight of these patients; of them, abnormal changes were detectable in the T1 sequence in six cases (75%), but in the other two cases (patients 3 and 5) pathological changes were detectable only in STIR sequences (Fig. 3a, d). Furthermore, evidence of muscular involvement was generally more apparent and extensive in STIR sequences than in T1 sequences (Fig. 3b, e). Finally, five patients had a control muscle MRI after an interval of 3–5 years, a period during which they kept showing normal motor balance. Three of these five patients showed a progression of radiological alterations (Fig. 3c, f) and one patient with a previously normal MRI showed new signs of edema in the medial gastrocnemius muscle (detected only in STIR sequences) (Fig. 3a, d).
Muscle MRI. Muscle MRI at calf level (patient 3) showing incipient pathological changes in medial gastrocnemius muscles bilaterally (right > left), absent in T1 sequences (a) and detectable only in STIR sequences (d). Muscle MRI at thigh level (patient 2) showing more apparent and extensive muscular involvement in STIR (e) compared with T1 sequences (b); there is an asymmetric involvement of both adductors and semimembranous muscles (right > left) in T1 sequences, and a more extensive involvement of the posterior compartment of the right thigh in STIR sequences, preserving only gracilis and sartorius muscles. Control muscle MRI at thigh level (patient 2) after a period of three years showing progression of the radiological involvement of the posterior compartment of the thighs asymmetrically, appreciable in T1 sequences (c) and more apparent in STIR sequences (f); gracilis and sartorius muscles remain intact
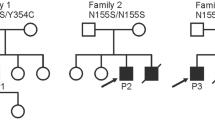
Genetic results
NGS analysis of ANO5 revealed a total of 12 different homozygous or compound heterozygous mutations, all with a recessive inheritance pattern. The most frequent mutations detected in our series were the missense variants c.692G > T (p.Gly231Val) in exon 8 and c.191dupA (p.Asn64LysfsX15) in exon 5. Both variants have been described as the most common mutations associated with LGMDR12 and MMD3 phenotypes [8], whereas asymptomatic hyperCKemia has only been associated with the latter [9]. Half of all the patients (10/20) harbored the c.191dupA variant: patients 6, 7, 10, 12 and 15 were homozygous, and patients 2, 4, 8, 17 and 18 were compound heterozygous. By contrast, the c.692G > T variant was detected in homozygosity in five patients (patients 3, 5, 9, 11 and 20), whereas patients 2, 14 and 19 had this variant in compound heterozygosity. One patient (patient 8) had the previously described nonsense mutation c.220C > T (p.Arg74X) in exon 5, which has been reported to cause LGMDR12 [10] but not asymptomatic hyperCKemia.
Seven mutations in our study have not been previously reported. In patient 1, we identified two previously unreported compound heterozygous mutations in ANO5: a missense variant on one allele in exon 8 (c.653A > G, p.Tyr218Cys), classified as of uncertain significance, and a second variant on the other allele in exon 11 (c.1088G > A, p.Trp363Ter). This latter sequence change creates a premature translational stop signal and is expected to result in a loss or truncation of the protein product.
Patient 4 was compound heterozygous for the already reported genetic duplication c.191dup and a second new variant, c.1982 T > C, p.Leu661Pro. Patient 13 was compound heterozygous for two novel missense variants: c.2317A > G and c.2222C > G, in exons 20 and 19, respectively. Patient 14 was compound heterozygous for the relatively frequent c.692G > T variant and a new missense variant c.950C > A. All of these newly described missense variants are classified as of uncertain significance by AGCM classification criteria and are predicted as deleterious by the likelihood ratio test.
Finally, Patient 18 was compound heterozygous for the known c.191dup variant and a novel frameshift mutation, c.108_109delGA, p.Glu36AspfsTer7, classified as pathogenic by AGCM classification criteria.
Discussion
Here we describe 20 adult patients with long-standing asymptomatic/paucisymptomatic anoctaminopathy, highlighting their clinical and radiological characteristics.
Clinical aspects
Anoctaminopathy is recently viewed as a relatively common cause of muscular diseases, presenting either as proximal (LGMDR12) or distal (MMD3) weakness, or as paucisymptomatic hyperCKemia. Indeed, Penttilä et al. reported that up to 25% of previously undiagnosed cases associated with one of the aforementioned clinical presentations were found to have pathogenic recessive mutations in ANO5 [11].
Isolated asymptomatic or mildly symptomatic hyperCKemia is increasingly recognized as a frequent presentation of anoctaminopathy. In the aforementioned study by Penttilä et al., 36% of patients with ANO5 mutations presented with hyperCKemia without muscle weakness [11]. Likewise, in a very recent study of 66 patients with isolated hyperCKemia, pathogenic or likely pathogenic ANO5 variants were found to be the underlying cause of 6% of the total cases, representing 30% of all the pathogenic mutations (excluding likely pathogenic variants) found in the cohort [12]. Accordingly, mutations in ANO5 should be considered as part of the differential diagnosis when encountering persistently high CK levels of unknown origin, ranging from mild to severe (200–40,000 IU/l), as previously reported by Papadopoulos et al. [1]. In these cases, genetic testing is the only way to achieve a definitive diagnosis.
In our cohort, calf hypertrophy was the only relevant finding on neuromuscular examination, and was present in eight of 20 patients (40%). This feature has been previously described in patients presenting with paucisymptomatic anoctaminopathy [1, 2, 11, 13] and is not rarely reported in symptomatic patients harboring ANO5 mutations [13]. Because calf hypertrophy is the most common neuromuscular feature associated with all clinical forms of dystrophinopathies [14], these disorders should be suspected first. However, we would recommend that, once deletions/duplications in the Duchenne muscular dystrophy (DMD) gene are ruled out, the SGC, FKRP, CAPN3 and ANO5 genes should be studied simultaneous to the sequencing of the entire DMD gene through NGS approaches [2], as they are all candidates for mutations that manifest a similar phenotype.
Exercise intolerance, encountered in five patients, has also been previously described as the sole clinical manifestation in patients with mutations in ANO5 [1, 11, 13, 15]. In these cases, metabolic myopathies should also be considered in the differential diagnosis, as well as other muscular dystrophies that can present with a pseudometabolic phenotype, such as those associated with dystrophin, dysferlin, sarcoglycans, fukutin-related protein and calpain-3, and caveolin-related disorders [16,17,18,19].
It has been proposed that anoctaminopathy with isolated hyperCKemia and presenting with overt weakness might constitute a continuum of the same pathological process, although no genotype–phenotype correlation has been found [1]. The age at the detection of hyperCKemia does not seem to predict the evolution of the disease [1], and additional genetic factors should be studied to explain the differences found in the severity of the phenotypes. Indeed, the proportion of this mild phenotype among anoctaminopathies is highly discordant in the literature. Considering series of anoctaminopathies comprising at least ten patients, the proportion of asymptomatic ANO5 patients ranged from 10 to 52% [1, 11, 13, 20,21,22]. In our series, asymptomatic/paucisymptomatic patients represented 74% of all patients with ANO5 mutations followed in the two reference centers participating in the study.
Muscle biopsy
Regarding muscle biopsy, we would like to highlight the three asymptomatic patients whose muscle biopsy showed inflammatory changes. Occasional lymphocytic infiltrations (as observed in patients 7 and 13) but not prominent (as observed in patient 2) have previously been reported in the muscle biopsy of patients with ANO5 mutations [11], leading to the misdiagnosis as myositis. In these cases, MHC-I immunostaining may help to differentiate genuine inflammatory myopathies from dystrophies associated with inflammatory foci. Nevertheless, in our series, patient 2 showed a false-positive MHC-I immunostaining (Fig. 2) and was initially diagnosed with polymyositis. Other described findings that contribute to a misdiagnosis of inflammatory myopathies are the presence of necrotic fibers on biopsy, signs of edema on MRI, and pathological spontaneous activity on electromyography [13]. However, the lack of a reduction in CK levels or clinical response to immunosuppressive therapy argues against this diagnosis [13].
Lymphocytic infiltrations have increasingly been reported in other genetic myopathies, for example, facioscapulohumeral muscular dystrophy [23, 24], dysferlinopathies [18] and titinopathy [25], among others. While the discussion of these histologic findings goes beyond the scope of this study, we would nevertheless underscore the importance of reading and interpreting complementary results always within the clinical framework.
Genetic studies
Most patients in our cohort carried two of the most common variants of ANO5 gene in Europe [13], c.191dupA and c.692G > T, either showing homozygosity or compound heterozygosity with other less common variants. Accordingly, similar to the muscular dystrophy phenotype, exons 5 and 8 are also hot spots for mutations in ANO5 that cause only hyperCKemia.
We also report seven novel variants in heterozygosis, six missense variants classified as of uncertain significance by the AGCM and predicted as deleterious by the likelihood ratio test, and one nonsense mutation classified as pathogenic with the same criteria.
Muscle MRI
Muscle MRI plays an increasingly important role in the diagnostic workup of muscular diseases [26]. In this sense, previous studies have revealed that muscle MRI of ANO5 patients shows characteristic and homogeneous—although non-specific—patterns irrespective of the clinical phenotype. At the level of the thigh, the most frequent and severely affected muscles are the adductors, followed by semimembranosus and semitendinosus muscles. By contrast, gracilis, sartorius and the short head of the biceps femoris are rarely affected and only then at later stages of the disease [3, 4, 13]. At the calf level, involvement of the medial gastrocnemius and soleus muscles is the most typical finding [3, 4, 13]. Interestingly, muscle involvement in anoctaminopathies is typically asymmetrical [11, 13], and anterior compartments are usually spared or only slightly affected in later stages [4]. Our study is in consonance with these findings, and also highlights that the medial gastrocnemius muscle seems to be the earliest and most severely affected muscle in ANO5 patients, as all patients with abnormal muscle MRI in our study showed some degree of medial gastrocnemius muscle involvement.
Eighteen of the 19 patients in our series with available muscle MRI showed some degree of radiological involvement. In this sense, our study also draws attention to the fact that typical radiological abnormalities may be present even in the absence of overt weakness [1]. Moreover, these changes can evolve over time [1, 2], as demonstrated by the presence of radiological progression in four of five patients with sequential MRI assessments. In addition, and as previously demonstrated in other dystrophies [27, 28], STIR sequences are more sensitive than T1 sequences in detecting incipient changes [4]. Indeed, it is remarkable that two patients showed pathological changes detectable solely in STIR sequences (patients 3 and 5). With all these considerations in mind, we strongly believe that muscular MRI is a powerful tool to aid in the differential diagnosis and guide genetic tests in patients with asymptomatic hyperCKemia.
High CK levels were the sole manifestation of the disease during our patients’ follow-up (several years in some cases), without the appearance of any other symptom despite the pathological changes in muscle MRI. The mean age at diagnosis of these patients is rather high (48 years) compared with the age of patients diagnosed with other dystrophies. This raises the question as to whether asymptomatic hyperCKemia is actually a mild phenotype in a wide clinical spectrum of anoctaminopathies rather than always a prodromal sign. In this sense, more studies are needed to predict its progression.
Conclusions
Recessive mutations in ANO5 are a frequent cause of asymptomatic or mildly symptomatic hyperCKemia. There is no genotype–phenotype correlation, and the same frequent mutations responsible for muscular dystrophy can also cause isolated persistent high CK levels. There is no known factor that serves to predict clinical progression: neither the age of detection nor the radiological findings are useful. In addition, we would underscore that patients with an apparent indolent phenotype may show evident muscle involvement in complementary tests (muscle biopsy and imaging), which may even progress over time. Finally, additional studies are warranted to further define remaining uncertainties about the clinical evolution of ANO5 patients, which may allow more reliable prognostic predictions to be made at the moment of diagnosis.
References
Papadopoulos C, LaforÊt P, Nectoux J et al (2017) Hyperckemia and myalgia are common presentations of anoctamin-5-related myopathy in French patients: HyperCKemia and Myalgia in ANO5-Related Myopathy. Muscle Nerve 56:1096–1100. https://doi.org/10.1002/mus.25608
Wicklund MP, Kissel JT (2014) The Limb-Girdle muscular dystrophies. Neurol Clin 32:729–749. https://doi.org/10.1016/j.ncl.2014.04.005
Cai S, Gao M, Xi J et al (2019) Clinical spectrum and gene mutations in a Chinese cohort with anoctaminopathy. Neuromuscul Disord 29:628–633. https://doi.org/10.1016/j.nmd.2019.06.005
Sarkozy A, Deschauer M, Carlier R-Y et al (2012) Muscle MRI findings in limb girdle muscular dystrophy type 2L. Neuromuscul Disord 22:S122–S129. https://doi.org/10.1016/j.nmd.2012.05.012
Mahjneh I, Bashir R, Kiuru-Enari S et al (2012) Selective pattern of muscle involvement seen in distal muscular dystrophy associated with anoctamin 5 mutations: a follow-up muscle MRI study. Neuromuscul Disord 22:S130–S136. https://doi.org/10.1016/j.nmd.2012.02.007
Panadés-de Oliveira L, Rodríguez-López C, Cantero Montenegro D et al (2019) Bethlem myopathy: a series of 16 patients and description of seven new associated mutations. J Neurol 266:934–941. https://doi.org/10.1007/s00415-019-09217-z
Richards S, Aziz N, Bale S et al (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 17:405–423. https://doi.org/10.1038/gim.2015.30
Bolduc V, Marlow G, Boycott KM et al (2010) Recessive mutations in the putative calcium-activated chloride channel anoctamin 5 cause proximal LGMD2L and distal MMD3 muscular dystrophies. Am J Hum Genet 86:213–221. https://doi.org/10.1016/j.ajhg.2009.12.013
Schessl J, Kress W, Schoser B (2012) Novel ANO5 mutations causing hyperCKemia, limb girdle muscular weakness and Miyoshi type of muscular dystrophy: short reports. Muscle Nerve 45:740–742. https://doi.org/10.1002/mus.23281
Magri F, Bo RD, D’Angelo MG et al (2012) Frequency and characterisation of anoctamin 5 mutations in a cohort of Italian limb-girdle muscular dystrophy patients. Neuromuscul Disord 22:934–943. https://doi.org/10.1016/j.nmd.2012.05.001
Penttilä S, Palmio J, Suominen T et al (2012) Eight new mutations and the expanding phenotype variability in muscular dystrophy caused by ANO5. Neurology 78:897–903. https://doi.org/10.1212/WNL.0b013e31824c4682
Rubegni A, Malandrini A, Dosi C et al (2019) Next-generation sequencing approach to hyperCKemia: a 2-year cohort study. Neurol Genet 5:e352. https://doi.org/10.1212/NXG.0000000000000352
Silva AMS, Coimbra-Neto AR, Souza PVS et al (2019) Clinical and molecular findings in a cohort of ANO5 -related myopathy. Ann Clin Trans Neurol 6:1225–1238. https://doi.org/10.1002/acn3.50801
Reimers CD, Schlotter B, Eicke BM, Witt TN (1996) Calf enlargement in neuromuscular diseases: a quantitative ultrasound study in 350 patients and review of the literature. J Neurol Sci 143:46–56. https://doi.org/10.1016/S0022-510X(96)00037-8
Milone M, Liewluck T, Winder TL, Pianosi PT (2012) Amyloidosis and exercise intolerance in ANO5 muscular dystrophy. Neuromuscul Disord 22:13–15. https://doi.org/10.1016/j.nmd.2011.07.005
Quinlivan R, Jungbluth H (2012) Myopathic causes of exercise intolerance with rhabdomyolysis: review. Dev Med Child Neurol 54:886–891. https://doi.org/10.1111/j.1469-8749.2012.04320.x
Scalco RS, Gardiner AR, Pitceathly RDS et al (2016) CAV3 mutations causing exercise intolerance, myalgia and rhabdomyolysis: expanding the phenotypic spectrum of caveolinopathies. Neuromuscul Disord 26:504–510. https://doi.org/10.1016/j.nmd.2016.05.006
Gallardo E, Saenz A, Illa I (2011) Limb-girdle muscular dystrophy 2A. In: Handbook of clinical neurology. Elsevier, Amsterdam, pp 97–110
Krahn M, Beroud C, Xi J et al (2014) Clinical heterogeneity and a high proportion of novel mutations in a Chinese cohort of patients with dysferlinopathy. Neurol India 62:635. https://doi.org/10.4103/0028-3886.149386
Sarkozy A, Hicks D, Hudson J et al (2013) ANO5 gene analysis in a large cohort of patients with anoctaminopathy: confirmation of male prevalence and high occurrence of the common exon 5 gene mutation. Hum Mutat 34:1111–1118. https://doi.org/10.1002/humu.22342
Witting N, Duno M, Petri H et al (2013) Anoctamin 5 muscular dystrophy in Denmark: prevalence, genotypes, phenotypes, cardiac findings, and muscle protein expression. J Neurol 260:2084–2093. https://doi.org/10.1007/s00415-013-6934-y
Savarese M, Di Fruscio G, Tasca G et al (2015) Next generation sequencing on patients with LGMD and nonspecific myopathies: findings associated with ANO5 mutations. Neuromuscul Disord 25:533–541. https://doi.org/10.1016/j.nmd.2015.03.011
Frisullo G, Frusciante R, Nociti V et al (2011) CD8+ T cells in facioscapulohumeral muscular dystrophy patients with inflammatory features at muscle MRI. J Clin Immunol 31:155–166. https://doi.org/10.1007/s10875-010-9474-6
Fitzsimons RB (1994) Facioscapulohumeral dystrophy: the role of inflammation. Lancet 344:902–903. https://doi.org/10.1016/s0140-6736(94)92263-2
Dabby R, Sadeh M, Hilton-Jones D et al (2015) Adult onset limb-girdle muscular dystrophy—a recessive titinopathy masquerading as myositis. J Neurol Sci 351:120–123. https://doi.org/10.1016/j.jns.2015.03.001
Warman Chardon J, Díaz-Manera J, Tasca G et al (2019) MYO-MRI diagnostic protocols in genetic myopathies. Neuromuscul Disord 29:827–841. https://doi.org/10.1016/j.nmd.2019.08.011
Dahlqvist JR, Andersen G, Khawajazada T et al (2019) Relationship between muscle inflammation and fat replacement assessed by MRI in facioscapulohumeral muscular dystrophy. J Neurol 266:1127–1135. https://doi.org/10.1007/s00415-019-09242-y
Angelini C, Peterle E, Gaiani A et al (2011) Dysferlinopathy course and sportive activity: clues for possible treatment. Acta Myol 30:127–132
Acknowledgements
This work was supported by grants from Fundación Mutua Madrileña (2018/0125), the Instituto de Salud Carlos III (ISCIII) (PI11/01330) and from Fundación Isabel Gemio.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Panadés-de Oliveira, L., Bermejo-Guerrero, L., de Fuenmayor-Fernández de la Hoz, C.P. et al. Persistent asymptomatic or mild symptomatic hyperCKemia due to mutations in ANO5: the mildest end of the anoctaminopathies spectrum. J Neurol 267, 2546–2555 (2020). https://doi.org/10.1007/s00415-020-09872-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-09872-7