Abstract
Background
Intracranial stenoses can cause TIA/ischaemic stroke. The purpose of this study was to assess vascular risk factors, clinical and imaging findings and outcome in Caucasians with intracranial stenosis under best prevention management.
Methods
In this prospective observational study (from 05/2012, to last follow-up 06/2017) we compared vascular risk factors, imaging findings and long-term outcome in Swiss patients with symptomatic versus asymptomatic intracranial atherosclerotic stenoses on best prevention management.
Results
62 patients were included [35.5% women, median age 68.3 years], 33 (53.2%) with symptomatic intracranial stenoses. Vascular risk factors (p = 0.635) and frequency of anterior circulation stenoses (66.7% vs. 55.2%; p = 0.354) did not differ between symptomatic and asymptomatic patients, but CT/MR-perfusion deficits in the territory of the stenosis (81.8% vs. 51.7%; p = 0.011) were more common in symptomatic patients. Outcome in symptomatic and asymptomatic patients at last follow-up was similar (mRS 0–1:66.7% vs. 75%;adjp = 0.937, mRS adjp-shift = 0.354, survival:100% vs. 96.4%;adjp = 0.979). However, during 59,417 patient follow-up days, symptomatic patients experienced more cerebrovascular events (ischaemic stroke or TIA) [37.5% vs. 7.1%;adjHR 7.58;adjp = 0.012], mainly in the territory of the stenosis [31.3% vs. 3.6%;adjHR 12.69;adjp = 0.019], more vascular events (i.e. ischaemic stroke/TIA/TNA and acute coronary/peripheral vascular events) [62.5% vs. 14.3%;adjHR 6.37;adjp = 0.001]) and more multiple vascular events (p-trend = 0.006; ≥ 2:37.5% vs. 10.7%;adj OR 5.37;adjp = 0.022) than asymptomatic patients.
Conclusions
Despite best prevention management, one in three patients with a symptomatic intracranial stenosis suffered a cerebrovascular event, three in five a vascular event and two in five ≥ 2 vascular events. There is an unmet need for more rigorous and effective preventive strategies in patients with symptomatic intracranial stenoses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intracranial atherosclerotic stenoses frequently cause cerebrovascular events (CVE), most common among Asians (up to 50%), less among Hispanics and Blacks, least among Caucasians (around 10%) [1]. The difference between ethnic groups has various causes. Genetic factors, but also differences in lifestyle and vascular risk factors (VRF) play a role. Globally, intracranial stenoses might be one of the most common aetiologies of CVE [2]. Moreover, intracranial stenoses are becoming more frequent, as often their cause is atherosclerosis. Atherosclerosis is driving mortality/morbidity worldwide and is age-related. People are getting increasingly older [3].
Rarer causes of intracranial stenoses are a partially occlusive thrombus, vasospasm, vasculitis, arterial dissection, moyamoya disease, radiation-induced arteriopathy, etc. [4]. Antiplatelets, antihypertensives and statins are effective in reducing vascular events (VE) in atherosclerosis [5,6,7,8].
In this prospective observational study we assessed VRF, imaging findings and 3 years outcome in a Swiss cohort with intracranial atherosclerotic stenosis under best prevention management and compared symptomatic and asymptomatic patients.
Methods
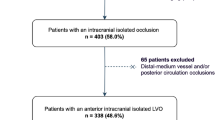
From 05/2012 to 06/2014 we prospectively included 62 patients with symptomatic (SISP) and asymptomatic intracranial atherosclerotic stenosis (AISP) in this observational study. Patients were randomly selected in case of intracranial atherosclerotic stenosis whilst on clinically indicated visits (online resource material Methods. S1) in our neurovascular sonography laboratory at the Bernese Stroke Centre (reference centre for cerebrovascular disease) by transcranial colour-coded duplex (TCCD) sonography performed by neurologists certified for cerebrovascular disease and sonography.
Number of included patients (in average 2.5 patients per month) was determined by logistics such as availability of CT- and/or MR-angiography for research purposes and by availability of time-slots for study visits.
Screened patients were not included in this study in case of the following predefined conditions: CT- and/or MR-angiographically not confirmed intracranial stenosis at baseline or at 3 months follow-up (two patients), intracranial stenosis of other than atherosclerotic aetiology (eleven patients), pregnancy (none), severe systemic disease with life expectancy < 1 year (e.g. cancer, severe heart failure) (one patient), severe renal insufficiency (four patients) and in case of patients’ rejection to participate (seven patients).
Intracranial stenoses in the middle cerebral (MCA), anterior cerebral (ACA), posterior cerebral (PCA), basilar (BA) and vertebral artery (VA) were graded in < 50%/ ≥ 50% using previously reported criteria [9]. Intracranial stenoses in the internal carotid artery (ICA) were graded in < 50% if flow velocity was locally increased and in ≥ 50% if pre-/poststenotic flow changes were present. Patients were assigned to the symptomatic group in case of transient ischaemic attack (TIA) and/or ischaemic stroke in the territory of the involved stenotic artery at baseline (within 30 days; time-frame chosen in order to be easier comparable with the previous studies SAMMPRIS and VISSIT and to account for relatively early recurrent CVE). TIA and stroke were defined according to the tissue-based definition (AHA/ASA guidelines) [10].
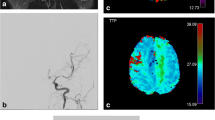
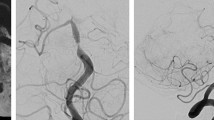
All neuroradiological images were reviewed by two neuroradiologists blinded to TCCD sonography and clinical data. Diagnosis of intracranial stenosis was confirmed by CT- and/or MR-angiography and if clinically indicated, by digital subtraction angiography and if a visually focal narrowing of the artery identified angiographically correlated with the precise location of the increased flow-velocity in neurosonography. CT/MR-perfusion deficits were defined as visually confirmed reduced perfusion. In case of multiple intracranial stenoses per patient, the main stenosis was selected as follows: First, a symptomatic stenosis was chosen over an asymptomatic one. Second, a ≥ 50% stenosis was chosen over a < 50% one; third, a single stenosis over a tandem one and fourth, a stenosis easily measureable with neurovascular sonography over one which was not. Severity of atherosclerosis at the carotid bifurcation was classified by neurovascular sonography in the presence and absence of plaques and stenosis of < 50%/ ≥ 50%.
Atherosclerotic aetiology of stenosis was identified by the combination of VRF, extracranial atherosclerosis in neurovascular sonography, appropriate findings in vessel wall high-resolution MRA and CTA and no other evident cause of intracranial stenosis (i.e. vasculitis, arterial dissection, etc.).
Atherosclerotic plaques were graded according to their size and degree of stenosis according to NASCET criteria [11]. Extracranial stenoses at vertebral artery origins were divided into stenoses of < 50%/ ≥ 50% according to the neurovascular sonography criteria defined by Hua and co-workers [12].
Baseline characteristics, demographic data and VRF were recorded. Clinical evaluation was performed by a certified stroke neurologist using the 15-item version of the NIHSS score [13]. Patients’ involvement in the study did not influence any decision made by the treating physicians. In all patients, best prevention management was continued or started on day 1. It consisted of antiplatelets (dual for 90 days if symptomatic), antihypertensive drugs (target blood pressure < 140/90 mmHg; in diabetics < 130/80 mmHg; in severe CT/MR-perfusion deficits in the stenosis territory 140/90 mmHg), high-intensity statin therapy (target LDL values < 1.8 mmol/L) and recommendations for lifestyle modification (including smoking cessation, regular physical activity, achieving normal body weight and healthy diet). The exact long-term drug regime was managed by the patient’s primary care physician, who is primarily responsible for long-term care of patients in the Swiss healthcare system. Rescue endovascular therapy (EVT) was performed if deemed necessary by the treating physicians. Reasons for rescue EVT were early recurrent ischaemic strokes, multiple recurrent ischaemic strokes despite best prevention management or patients with acute vessel occlusion.
A stroke study nurse followed up patients via telephone at 1 month. At 3 months, at 1, 2 and at 3 years, a clinical follow-up was done face-to-face by a stroke neurologist and a stroke study nurse (including monitoring of best prevention management and of neurovascular sonography). At 3 months, at 1 and at 2 years, also CT- and/or MR-imaging including CT-/MR-angiography was performed. VE were defined as new ischaemic strokes, TIA, transient neurological attack (TNA; in this study, defined as any of the following transient nonfocal symptoms: disturbed consciousness, confusion, amnesia, unsteadiness, nonrotatory dizziness, positive visual phenomena, paraesthesias, cardiac or vegetative signs, bilateral weakness or unwell feeling [14]) or acute coronary/peripheral VE; CVE were defined as new ischaemic strokes or TIA. New events were identified by patient history, checking patient records, clinical and imaging findings. Clinical outcome was measured with the modified Rankin scale (mRS), National Institutes of Health Scale (NIHSS) score and with an additional measure of health, the standardized descriptive EQ-5D-3L [13, 15, 16].
Statistical analysis
Predefined analyses were used to compare SISP and AISP. Baseline characteristics, demographic data, VRF and imaging findings were analysed using χ2 test for categorical variables and Fisher exact test if appropriate and Mann–Whitney-U-test for continuous and ordinal variables. We used Kaplan–Meier survival analysis to calculate the 3-year risks of events during follow-up. We studied the following outcomes using Cox regression analysis adjusted for age and sex: death, clinical outcome [according to modified Rankin scale (mRS)], quality of life (measured with the standardized descriptive EQ-5D-3L), CVE overall and attributable to the territory of the intracranial stenosis, silent ischaemic stroke during follow-up, TNA, VE, acute coronary/peripheral VE, symptomatic intracerebral haemorrhage (sICH: PROACT II criteria) [17], progression of intracranial stenosis (according to bimodal follow-up imaging) and rescue EVT. For mRS, adjusted shift analysis was performed additionally with ordinal regression analysis.
For the Kaplan–Meier survival and Cox regression analyses, data for patients who did not reach the end-point were censored at the end of the 3-year follow-up period or at the last known follow-up, whichever was earlier. We calculated the variance of frequency of events in both groups and the odds ratio in binary logistic regression of SISP over AISP for frequency (≥ 1/ ≥ 2/ ≥ 3/ ≥ 4) of CVE and VE. For analysis SPSS version 25 was applied.
Results
Among 62 patients [35.5% women, median age 68.3 (range 41.7–83.9) years] 33 (53.2%) were SISP. Their CVE at baseline were vastly mild. SISP had a higher degree of stenoses and of CT/MR-perfusion deficits in the territory of the stenosis than AISP (Table 1). Furthermore, number of VRF did not differ between both groups (p-trend = 0.635) (online resource material Fig. S1). Overall, 69.4% of patients had arterial hypertension and 79% hypercholesterolaemia. Baseline median LDL value was 3.69 (1.18–5.60) mmol/L in SISP and 2.80 (1.10–5.61) mmol/L in AISP, despite 46.9% and 79.3% (p = 0.009), respectively, being on statins. The rates of atherosclerosis of the extracranial vessels leading to the brain, a history of symptomatic coronary heart/peripheral vascular disease and/or of CVE in the territory of the stenosis are presented in Table 1. AISP were more likely to be on (primary or secondary) preventive medication for vascular disease such as antiplatelets, statins and antihypertensives (trend) prior to baseline (Table 1). The proportion of patients on preventive medication increased until last follow-up and reached similar proportions in both groups. At last follow-up, 28 (93.3%) of SISP were on antiplatelets, two (6.7%) on anticoagulants, 22 (73.3%) on antihypertensives and 29 (96.7%) on statins (Table 2). SISP were more frequently on high-intensity statins with atorvastatin or rosuvastatin at last follow-up (62.5% vs. 20.7%; p = 0.001) than AISP.
During 59,417 patient-days of follow-up, there were one non-vascular death, 14 CVE overall, eleven CVE in the territory of the stenosis, 15 TNA, 24 VE, three acute coronary or peripheral VE, but no intracranial haemorrhage (Table 3). 85.7% of CVE occurred in patients with a stenosis of ≥ 50%, two of which occurred within the first 3 months after baseline. More events were observed in patients with multiple intracranial stenoses (64.3%) and within the territory of the stenosis (85.7%). Only two CVE occurred outside the territory of the stenosis in SISP and one in AISP (Table 3). SISP had more CVE overall [37.5% vs. 7.1%;adjHR 7.58;adjp = 0.012], in the territory of the stenosis [31.3% vs. 3.6%;adjHR 12.69;adjp = 0.019] and more VE overall [62.5% vs.14.3%;adjHR 6.37;adjp = 0.001]. SISP had higher overall risk of CVE (log-rank-p = 0.010), in the territory of the stenosis (log-rank-p = 0.008), of VE overall (log-rank-p < 0.0001) and of TNA (log-rank-p = 0.005) than AISP (Fig. 1 and online resource material Fig. S2). Number of CVE (p-trend = 0.012) and VE (p-trend = 0.005) were significantly higher in SISP (Fig. 2). Neither more progressive intracranial stenoses (15.6% vs. 16%;adjp = 0.800) nor more rescue EVT (6.3% vs. 0%;adjp = 0.980) happened in SISP (details are presented in Table 4). Clinical outcome of SISP vs. AISP measured with the mRS at last follow-up did not differ: mRS 0:30% vs. 39.3%;adjp = 0.146, mRS 0–1:66.7% vs. 75%;adjp = 0.937, mRS shift analysis:adjp-shift = 0.354, mortality:0% vs. 3.6%;adjp = 0.979. Problems of health measured with the standardized descriptive EQ-5D-3L did not differ between the two groups and there was no difference in median NIHSS score at last follow-up which was low [0 (0–3) in both groups; p = 0.986] (Table 3).
Discussion
In this prospective single-centre 3-years’ follow-up study, we report on first and multiple recurrent VE and CVE, on TNA, on AISP besides SISP and on rescue EVT. Despite best medical treatment, recommendations for lifestyle modification and additional rescue EVT, one in three SISP versus one in 28 AISP suffered a CVE in the territory of the stenosis during 3-year follow-up. VE occurred in three of five SISP and in every seventh AISP. This despite recommendations having stressed the importance of best prevention management in SISP since SAMMPRIS (Stenting and Aggressive Medical Management for the Prevention of stroke in Intracranial Stenosis) and VISSIT (Vitesse Intracranial Stent Study for Ischemic Therapy) [18, 19].
Recurrence rates of CVE in the territory of the stenosis in patients treated with best preventive management have been reported previously: In WASID (Warfarin Aspirin Symptomatic Intracranial Disease), 13.5% ischaemic strokes occurred during a mean 1.8-year follow-up; in GESICA (Groupe d’Etude des Sténoses Intra-Crâniennes Athéromateuses symptomatiques) 13.7% ischaemic strokes and 24.5% TIA within 2 years, in SAMMPRIS 10.1% ischaemic strokes within a mean 12-month follow-up and in VISSIT 9.4% ischaemic strokes and 5.7% TIA by 1 year [18,19,20,21]. Of note, only SISP have been included in these studies. Despite higher degrees (≥ 70%) of stenoses in SAMMPRIS and VISSIT (vs. ≥ 50% in WASID and GESICA) and more recent symptoms (in SAMMPRIS and VISSIT < 30 days vs. in WASID < 90 days and in GESICA < 6 months prior to inclusion), recurrence rates were lower in SAMMPRIS and VISSIT than in WASID and GESICA. This has mainly been explained by a stricter control of VRF including antihypertensives, statins and lifestyle modification recommendations and dual antiplatelets for 3 months followed by long-term antiplatelets [18,19,20,21,22,23].
Compared to the just mentioned previous studies, the rate of recurrent CVE in our cohort was lower [18,19,20,21]. This may partly be explained by the inclusion of patients with a lower degree of stenosis (< 50%). Furthermore, we aimed for a timely [usually initiated on day 1 in SISP in clinical routine at our Bernese Stroke Centre, latest at study baseline (latter showing a median of 6 days after event in this study)] strict management of VRF in our cohort, which might also have contributed to the lower event rate than previously reported, especially in the early post-event time period. However, optimal control of VRF and healthy lifestyle was not fully achieved (only partly optimal patient adherence, smoking cessation and target blood pressure levels reached) during follow-up. At last follow-up one in four patients was still smoking and median blood pressure value was 142/81 mmHg. Rates of recurrent CVE in our cohort probably would have been lower with even better best prevention management. Also, PCSK-9 inhibitors, which have been shown to further reduce recurrent VE rates in recent RCTs in patients with vascular disease, were not yet available for our patients. Especially in high-risk patients, these drugs might be of future additional benefit [24,25,26].
In our study, CVE at baseline were vastly mild (39.4% TIA, 51.5% minor strokes) and similar as in previous prospective studies (TIA rates of 33–48.5%). Also, the majority of recurrent CVE during follow-up were not disabling and overall clinical outcome was favourable (last follow-up: median NIHSS score 0, excellent outcome in the majority of patients, one non-vascular death). In SAMMPRIS, rates of fatal or disabling ischaemic strokes in the territory of the stenosis during a mean follow-up of 12 months was 3.1%, whereas in VISSIT no patient died due to a recurrent ischaemic stroke in the stenosis territory; disabling strokes occurred in 7.1% of patients and median 12-month NIHSS score was 0 [18,19,20,21]. Ischaemic strokes due to intracranial stenoses are typically non-lacunar, can be disabling in some patients and should be prevented [27]. However, comparison with previous studies is undermined by different inclusion/exclusion criteria.
Additionally, we also assessed CVE rates in AISP. The CVE rates in the stenosis territory of AISP turned out to be ten times lower than in SISP, possibly considerably influenced by their asymptomatic status, selection in routine clinical practice, milder degree of stenosis and more intensive pre-existing intake of (primary or secondary) preventive drugs and trend towards lower LDL values at baseline. Our findings are in line with the recent population-based Barcelona-AsIA (Asymptomatic Intracranial Atherosclerosis) study [28]. However, this study also demonstrated that AISP were having increased CVE risk compared to patients without intracranial stenoses.
Several studies have failed to show a benefit of EVT over intensive VRF management in patients with intracranial stenoses [18, 19, 29, 30]. In SAMMPRIS, the recurrence rate of ischaemic strokes in the stenosis territory was 16.1% in the endovascular (vs. 10.1% in the medical) group within a mean 12-month follow-up. Moreover, ten symptomatic intracranial haemorrhages occurred, whereas only one sICH occurred in the medical group. Overall, outcomes were largely driven by haemorrhages at 30 days, showing no long-term benefit from EVT [18]. In VISSIT, 1-year rates of CVE in the territory of the stenosis and 30 days’ primary safety outcome (composite of any stroke, death or sICH) was 36% and 24.1%, respectively, in the endovascular (vs. 15.1% and 9.4% in the medical) group [19]. However, CVE in intracranial stenoses occur due to different mechanisms [31]. Subgroups might benefit from EVT or maybe also from surgical therapy. For example, haemodynamic impairment might not respond to antithrombotics and statins, and antihypertensives are potentially harmful. Also, patients with unstable plaques might not sufficiently benefit from non-interventional management. Finally, EVT might be performed in case of acute large vessel occlusion [32]. In our cohort, two patients received rescue EVT during follow-up (Table 4).
In our study, three CVE occurred in a non-stenosis territory and three acute coronary/peripheral VE. In WASID, 5.1% recurrent ischaemic strokes happened in non-stenosis territory and 3.3% myocardial infarctions, in GESICA (in the medical group), two CVE in a non-stenosis territory, 13.7% acute coronary and 4.9% peripheral VE and in SAMMPRIS (in the medical group), during a mean 12-month follow-up, 2.2% ischaemic strokes in a non-stenosis territory and 3.1% myocardial infarctions. In AsIA, within 7.17 years of follow-up, part of the recurrent CVE occurred outside the stenosis-territory and 18.8% coronary VE. Our findings of recurrent VE in different arterial beds as well as of VRF and concomitant atherosclerosis at baseline are supporting the previously shown systemic nature of atherosclerosis and increased vascular risk [18,19,20,21, 28, 33].
Limitations
Our study has limitations. First, our sample size is limited as is the power of some analyses. Our study remains largely descriptive. Second, we may have underestimated the burden of atherosclerosis, as we did not routinely screen patients for asymptomatic coronary/peripheral vascular disease. Third, best prevention management could have been even better. Not all targets were reached and for example, statins varied between patients, despite the majority being on statins during follow-up. Also, we did not routinely measure lipid or blood sugar levels and only partly present lifestyle measures (smoking status) during follow-up. Fourth, patients were recruited randomly. This approach bears the risk of selection bias. Fifth, patients defined as asymptomatic, selected in routine clinical practice, were likely to have a lower CVE and VE risk. Finally, two patients declined to be followed-up.
Conclusions
In this prospective study of SISP and AISP, treated with best prevention management and rescue EVT in two patients, one in three SISP suffered a CVE in the territory of the stenosis, three in five a VE and two in five ≥ 2 VE. Despite a good clinical outcome in the majority of patients in our cohort, there is an unmet need for more effective prevention of CVE in patients with intracranial stenoses, especially in SISP with ≥ 50% stenosis, who showed highest event rates in our study. Patients with intracranial stenoses might benefit from more rigorous prevention management and from more effective novel therapies. They should be a focus in future population-based studies and clinical trials.
References
Battistella V, Elkind M (2014) Intracranial atherosclerotic disease. Eur J Neurol 21:956–962. https://doi.org/10.1111/ene.12385
Gorelick PB, Wong KS, Bae HJ, Pandey DK (2008) Large artery intracranial occlusive disease: a large worldwide burden but a relatively neglected frontier. Stroke 39:2396–2399. https://doi.org/10.1161/STROKEAHA.107.505776
GBD 2015 Mortality and Causes of Death Collaborators (2016) Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the global burden of disease study 2015. Lancet 388:1459–1544. https://doi.org/10.1016/S0140-6736(16)31012-1
Smith SC Jr, Milani RV, Arnett DK, Crouse JR 3rd, McDermott MM, Ridker PM, Rosenson RS, Taubert KA, Wilson PW, American Heart Association (2004) Atherosclerotic vascular disease conference: writing group ii: risk factors. Circulation 109:2613–2616. https://doi.org/10.1161/01.CIR.0000128519.60762.84
Amarenco P, Bogousslavsky J, Callahan A 3rd, Goldstein LB, Hennerici M, Rudolph AE, Sillesen H, Simunovic L, Szarek M, Welch KM, Zivin JA, Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Investigators (2006) High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med 355:549–559. https://doi.org/10.1056/NEJMoa061894
Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, Kirby A, Sourjina T, Peto R, Collins R, Simes R, Cholesterol, Trialists’ (CTT) Collaborators (2005) Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 366:1267–1278. https://doi.org/10.1016/S0140-6736(05)67394-1Treatment
Antithrombotic Trialists' (ATT) Collaboration, Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, Peto R, Buring J, Hennekens C, Kearney P, Meade T, Patrono C, Roncaglioni MC, Zanchetti A (2009) Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet 373:1849–1860. https://doi.org/10.1016/S0140-6736(09)60503-1
Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, Chalmers J, Rodgers A, Rahimi K (2016) Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 387:957–967. https://doi.org/10.1016/S0140-6736(15)01225-8
Baumgartner RW, Mattle HP, Schroth G (1999) Assessment of ≥50% and <50% intracranial stenoses by transcranial color-coded duplex sonography. Stroke 30:87–92. https://doi.org/10.1161/01.str.30.1.87
Easton JD, Saver JL, Albers GW, Alberts MJ, Chaturvedi S, Feldmann E, Hatsukami TS, Higashida RT, Johnston SC, Kidwell CS, Lutsep HL, Miller E, Sacco RL (2009) Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American heart association/American stroke association stroke council; council on cardiovascular surgery and anesthesia; council on cardiovascular radiology and intervention; council on cardiovascular nursing; and the interdisciplinary council on peripheral vascular disease. Stroke 40:2276–2293. https://doi.org/10.1161/STROKEAHA.108.192218
Hathout GM, Fink JR, Saden SM, Grand EG (2005) Sonographic NASCET index: a new doppler parameter for assessment of internal carotid artery stenosis. Am J Neuroradiol 26:68–75
Hua Y, Meng XF, Jia LY, Ling C, Miao ZR, Ling F, Liu JB (2009) Color doppler imaging evaluation of proximal vertebral artery stenosis. Am J Roentgenol 193:1434–1438. https://doi.org/10.2214/AJR.09.2624
Lyden P, Brott T, Tilley B, Welch KM, Mascha EJ, Levine S, Haley EC, Grotta J, Marler J (1994) Improved reliability of the NIH Stroke Scale using video training. Stroke 25:2220–2226. https://doi.org/10.1161/01.str.25.11.2220
Bos MJ, van Rijn MJ, Witteman JC, Hofman A, Koudstaal PJ, Breteler MM (2007) Incidence and prognosis of transient neurological attacks. JAMA 298:2877–2885. https://doi.org/10.1001/jama.298.24.2877
Van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19:604–607. https://doi.org/10.1161/01.str.19.5.604
The EuroQol Group (1990) EuroQol-a new facility for the measurement of health-related quality of life. Health Policy 16:199–208. https://doi.org/10.1016/0168-8510(90)90421-9
Furlan A, Higashida R, Wechsler L, Gent M, Rowley H, Kase C, Pessin M, Ahuja A, Callahan F, Clark WM, Silver F, Rivera F (1999) Intra-arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. JAMA 282:2003–2011. https://doi.org/10.1001/jama.282.21.2003
Chimowitz MI, Lynn MJ, Derdeyn CP, Turan TN, Fiorella D, Lane BF et al (2011) Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med 365:993–1003. https://doi.org/10.1056/NEJMoa1105335
Zaidat OO, Fitzsimmons BF, Woodward BK, Wang Z, Killer-Oberpfalzer M, Wakhloo A, Gupta R, Kirshner H, Megerian JT, Lesko J, Pitzer P, Ramos J, Castonguay AC, Barnwell S, Smith WS, Gress DR, for the VISSIT Trial Investigators (2015) Effect of a balloon expandable intracranial stent vs medical therapy on risk of stroke in patients with symptomatic intracranial stenosis: the VISSIT randomized clinical trial. JAMA 313:1240–1248. https://doi.org/10.1001/jama.2015.1693
Chimowitz MI, Lynn MJ, Howlett-Smith H, Stern BJ, Hertzberg VS, Frankel MR, Levine SR, Chaturvedi S, Kasner SE, Benesch CG, Sila CA, Jovin TG, Romano JG, for the Warfarin–Aspirin Symptomatic Intracranial Disease Trial Investigators (2005) Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med 352:1305–1316. https://doi.org/10.1056/NEJMoa043033
Mazighi M, Tanasescu R, Ducrocq X, Vicaut E, Bracard S, Houdart E, Woimant F (2006) Prospective study of symptomatic atherothrombotic intracranial stenoses: the GESICA study. Neurology 66:1187–1191. https://doi.org/10.1212/01.wnl.0000208404.94585.b2
Boekholdt SM, Hovingh GK, Mora S, Arsenault BJ, Amarenco P, Pedersen TR, LaRosa JC, Waters DD, DeMicco DA, Simes RJ, Keech AC, Colquhoun D, Hitman GA, Betteridge DJ, Clearfield MB, Downs JR, Colhoun HM, Gotto AM Jr, Ridker PM, Grundy SM, Kastelein JJ (2014) Very low levels of atherogenic lipoproteins and the risk for cardiovascular events: a meta-analysis of statin trials. J Am Coll Cardiol 64:485–494. https://doi.org/10.1016/j.jacc.2014.02.615
Amarenco P, Labreuche J (2009) Lipid management in the prevention of stroke: review and updated meta-analysis of statins for stroke prevention. Lancet Neurol 8:453–463. https://doi.org/10.1016/S1474-4422(09)70058-4
Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C et al (2017) Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med 377:1119–1131. https://doi.org/10.1056/NEJMoa1707914
Sabatine MS, Giugliano RP, Keech AC, Honarpour N, Wiviott SD, Murphy SA, Kuder JF, Wang H, Liu T, Wasserman SM, Sever PS, Pedersen TR, FOURIER Steering Committee and Investigators (2017) Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med 376:1713–1722. https://doi.org/10.1056/NEJMoa1615664
Bowman L, Hopewell JC, Chen F, Wallendszus K, Stevens W, Collins R, Wiviott SD, Cannon CP, Braunwald E, Sammons E, Landray MJ (2017) Effects of anacetrapib in patients with atherosclerotic vascular disease. N Engl J Med 377:1217–1227. https://doi.org/10.1056/NEJMoa1706444
Wardlaw JM, Doubal FN, Eadie E, Chappell F, Shuler K, Cvoro V (2011) Little association between intracranial arterial stenosis and lacunar stroke. Cerebrovasc Dis 31:12–18. https://doi.org/10.1159/000319773
Planas-Ballvé A, Crespo AM, Aguilar LM, Hernández-Pérez M, Canento T, Dorado L, Alzamora MT, Torán P, Pera G, Muñoz-Ortiz L, Arenillas JF, Castañón M, Dávalos A, Millán M, López-Cancio E (2019) The Barcelona-Asymptomatic Intracranial Atherosclerosis study: subclinical intracranial atherosclerosis as predictor of long-term vascular events. Atherosclerosis 282:132–136. https://doi.org/10.1016/j.atherosclerosis.2019.01.022
Maier IL, Karch A, Lipke C, Behme D, Mpotsaris A, Kabbasch C, Liebig T, Faymonville A, Reich A, Nikoubashman O, Buhk JH, von Schoenfeld P, Weber W, Mikolajczyk RT, Bähr M, Knauth M, Kallenberg K, Liman J (2018) Transluminal angioplasty and stenting versus conservative treatment in patients with symptomatic basilar artery stenosis: perspective for future clinical trials. Clin Neuroradiol 28:33–38. https://doi.org/10.1007/s00062-016-0528-x
Markus HS, Harshfield EL, Compter A, Kuker W, Kappelle LJ, Clifton A, van der Worp HB, Rothwell P, Algra A, Vertebral Stenosis Trialists' Collaboration (2019) Stenting for symptomatic vertebral artery stenosis: a preplanned pooled individual patient data analysis. Lancet Neurol 18:666–673. https://doi.org/10.1016/S1474-4422(19)30149-8
Bang OY (2014) Intracranial atherosclerosis: current understanding and perspectives. J Stroke 16:27–35. https://doi.org/10.5853/jos.2014.16.1.27
Jia B, Feng L, Liebeskind DS, Huo X, Gao F, Ma N, Mo D, Liao X, Wang C, Zhao X, Pan Y, Li H, Liu L, Wang Y, Wang Y, Miao ZR, EAST Study Group (2018) Mechanical thrombectomy and rescue therapy for intracranial large artery occlusion with underlying atherosclerosis. J Neurointerv Surg 10:746–750. https://doi.org/10.1136/neurintsurg-2017-013489
Heldner MR, Li L, Lovett N, Kubiak MM, Lyons S, Rothwell PM (2018) Long-term prognosis of patients with TIA and ischaemic stroke who have symptomatic vascular disease in multiple arterial beds: population-based cohort study. Stroke 49:1639–1646. https://doi.org/10.1161/STROKEAHA.118.020913
Data availabilty
Raw data of all patients included in this study can be made available upon request to the corresponding author and after clearance by the local ethics committee.
Acknowledgements
We are grateful to the whole Bernese stroke team; who also contributed to SAISS.
Funding
The study was supported by a Swiss Heart Foundation Grant.
Author information
Authors and Affiliations
Contributions
MRH and UF take responsibility for the integrity of the data and the accuracy of the data analysis. Access to all the data: all co-authors. Study concept, design and supervision: MRH and UF. Acquisition of data: Bernese Stroke Team. Extraction of data and statistical analysis: MRH. Analysis and interpretation: MRH. Drafting of the manuscript: MRH and UF. Critical revision of the manuscript for important intellectual content: all listed co-authors.
Corresponding author
Ethics declarations
Conflicts of interest
U. Fischer, P. Michel and J. Gralla were supported by a Swiss Heart Foundation grant directly related to this study. All other co-authors report no disclosures directly related to this manuscript.
Ethical approval
The study was approved by the local ethics committee of the canton of Bern/Switzerland (KEK number: 127/11) and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Written informed consent was obtained from all patients. We complied with the principles of the Declaration of Helsinki and with the STROBE checklist.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fischer, U., Hsieh-Meister, K., Kellner-Weldon, F. et al. Symptomatic and asymptomatic intracranial atherosclerotic stenosis: 3 years’ prospective study. J Neurol 267, 1687–1698 (2020). https://doi.org/10.1007/s00415-020-09750-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-09750-2