Abstract
The discriminative value of CSF total protein (CSF-TP) in subtypes of Guillain–Barré syndrome has not been well documented in North-American patients. We reviewed 173 cases from a single institution, comprising the following clinical categories of neuropathy: 134 Sensorimotor (SM) GBS, 13 Motor (M) GBS, 8 Localized (L) GBS, and 18 Miller Fisher syndrome (MFS). We grouped the electrophysiological interpretation in primarily demyelinating, primarily axonal and normal / equivocal categories. Mean CSF-TP were substantially higher for SM and L-GBS, as well as cases classified as Acute-onset chronic inflammatory demyelinating polyneuropathy. They were lower for M-GBS and L-GBS. The most statistically significant correlation was found for elevated CSF-TP in GBS cases showing an electrophysiologic pattern classified as demyelinating (1.56 g/L) compared with axonal (0.68 g/L) or normal/ equivocal patterns (0.65 g/L). There was a correlation between CSF-TP and time interval between symptom onset and lumbar puncture. There was a weak correlation between CSF-TP and maximal overall-clinical severity grade, which was likely mostly determined by the electorphysiological pattern. Though CSF-TP is a sensitive test for GBS in the second week after onset, it may not be a reliable predictor of clinical severity. There is a robust association of CSF-TP elevation and a demyelinative electrophysiologic pattern and a suggestion that lower mean CSF-TP values can be expected in GBS-spectrum disorders thought to represent nodo-paranodopathies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term Guillain–Barré syndrome (GBS) encompasses a spectrum of acute, mostly symmetrical polyradiculoneuropathies with hyporeflexia or areflexia. The presumed immune pathogenesis may involve both humoral and cell-mediated pathways, with immune targets thought to be localized in the Schwann cell membrane or the nodal/paranodal region. The anatomical distribution of initial symptomatic involvement in the PNS is also quite varied and it frequently does not follow a distal to proximal gradient. Early manifestations may thus include facial and oculomotor neuropathy, regional or diffuse spinal polyradiculopathy as well as demyelination in distal nerve segments [1]. The diagnosis of GBS is suggested when defined clinical criteria are met, but it is also imperative to exclude alternative toxic, infectious, neoplastic, and structural etiologies. Treatment must commonly be initiated prior to confirmatory testing. Nerve conduction studies are not routinely available in some institutions and may be normal or show only mild non-specific abnormalities in the first days after clinical onset [2, 3]. Electrodiagnostic hallmarks of GBS also evolve in a very dynamic pattern in the first two weeks after onset, and they commonly show an asynchronous correlation with the degree of clinical disability.
Although lumbar puncture is more invasive than nerve conduction studies, confirmatory testing via basic CSF analysis (cell count and total protein) is more readily available in hospitals worldwide. The selective rise in CSF total protein (CSF-TP) historically labelled “albuminocytologic dissociation” is a time-dependent phenomenon. We have previously reported in a smaller cohort of 138 GBS cases that the application of updated CSF-TP upper reference limits results in a diagnostic sensitivity of only 45% in the first week after onset [4]. The main diagnostic contribution of an early LP may be to identify infectious or neoplastic GBS mimics which commonly have higher CSF-nucleated cell counts. The rise in CSF-TP may however provide insights into key factors in the pathophysiology of GBS subtypes, such as the extent of radicular involvement, degree of blood-nerve barrier disruption, and myelin dysruption versus axonal antibody binding. In the present study, we analyzed a broader spectrum of GBS disorders to see whether the CSF-TP may help predict maximal clinical severity and whether there is a correlation with GBS subtypes classified by clinical presentation. We also separately analyzed the correlation of CSF-TP and electrophysiological pattern.
Methods
The study was approved by the Ottawa Hospital Research Institute Ethics Board (protocol 20160863). We reviewed all cases for which the discharge diagnosis coding for the years 2001–2016 at the Ottawa hospital included the terms Guillain–Barré syndrome or Inflammatory Neuropathy. All charts were reviewed by the same neuromuscular specialist (PRB). All patients had to present a mostly symmetric pattern of limb and/or cranial-nerve weakness with a monophasic course peaking within 28 days.
A successful lumbar puncture contemporaneous to the monophasic illness was required. Cases with a CSF white blood cell-count greater than 50 were excluded. The interval between onset of GBS symptoms and lumbar puncture was measured in days. Clinical onset of GBS was defined as the earliest documentation of sustained new paresthesia, sustained symmetrical muscular paresis, cranial neuropathy or definite ataxia. Spinal or appendicular pain were not considered a reliable initial symptom to date the clinical onset.
Based on purely clinical information, we classified 173 patients into subtypes defined by the GBS Classification Group [5]: classic GBS, localized-GBS (L-GBS), and Miller Fisher syndrome (MFS). We chose to subdivide classic GBS into cases of pure motor (M-GBS) and sensorimotor (SM-GBS) clinical presentation, based on the occurrence of sensory symptoms or signs, following the distinction proposed in an older consensus report [6]. We did not attempt to separate subtypes of localized-GBS (e.g., bifacial with paresthesia, pharyngeal-cervical-brachial, paraparetic) or distinguish subtypes of MFS (e.g., acute ophthalmoparesis, acute ataxic neuropathy, acute ptosis).We however excluded from the MFS category all cases where electrophysiologic studies showed clear demyelinating or axonal abnormalities on motor nerve conduction studies. Note that Anti-GQ1b antibodies were not part of routine testing for MFS in our institution during the study period.
We identified a separate group of Acute-onset CIDP (A-CIDP) patients where the initial historical diagnosis was AIDP but the progressive phase exceeded 8 weeks, or more than 1 relapse requiring further immunotherapy occurred in the first year. A-CIDP cases were required to have a primarily demyelinating pattern and were included only if there was a lumbar puncture contemporaneous with the acute symptomatic presentation.
The sum of the available NCS and EMG data were interpreted to allocate each case in one of the following categories: normal, mild/equivocal changes, primarily demyelinating, primarily axonal (motor), and primarily axonal (motor and sensory). Most patients had a single study with quite variable NCS protocols. The categories chosen were based on the modified criteria of Rajabally [7], adding the distinction of purely motor and sensorimotor axonal patterns.
Severity of involvement was categorized as the highest Hughes modified GBS disability scale level incurred [8, 9]. This a 7-item scale (0—healthy, 1—minor symptoms, able to run, 2—able to walk without stick, 3—able to walk with stick, 4—confined to wheelchair or bed, 5—requiring assisted ventilation, 6—deceased). It was chosen for its simplicity, and applicability to all forms of GBS. To achieve a clinically meaningful and numerically more powerful analysis, we compared ambulatory (grades 1–3) and non-ambulatory (grades 4–6) groups.
Statistical analysis
All statistical calculations and graphs were generated using R version 3.3.3 (The R Foundation, Vienna, Austria). QR decomposition was used to ascertain Ordinary Least Squares (OLS) estimates of parameters describing the linear relationships between the time to lumbar puncture and CSF-TP [10]. The 95% prediction interval was subsequently computed and plotted [11]. To assess the relationship of electrophysiologic pattern and CSF-TP, we grouped the NCS patterns in 3 broader categories: normal or mild/equivocal, primarily demyelinating, and primarily axonal (motor or sensorimotor). We excluded the A-CIDP patients from this analysis.
An ANOVA was applied to investigate for significant mean differences in protein levels when factoring in the clinical subtype of GBS, the electrophysiologic category and disease severity along as well as covariation with time-to-LP. Age and Sex were also included in the model as they have previously been shown to impact CSF-TP values. Tukey’s honestly significant difference (HSD) technique was subsequently used to interrogate the differences between groups when the null hypothesis was rejected for a given factor. The Akaike information criterion (AIC) was used to compare candidate models on which the ANOVA were based to ascertain the superior approach. A Chi-squared test was used when investigating the association between two categorical variables.
Results
392 cases were coded as GBS or inflammatory neuropathy. 48 cases were excluded because of lack of contemporaneous CSF analysis. 152 cases were excluded because there was insufficient clinical documentation, database coding errors, or a more likely diagnosis was reached at follow-up, such as neoplastic meningitis, spinal compression, or diabetic polyneuropathy. Only 6 cases (3 SM-GBS and 3 MFS) did not have EMG studies but were deemed to otherwise have had a typical clinical picture and evolution for their respective syndromes. In 19 cases coded in the hospital database as GBS or inflammatory neuropathy, a diagnosis of CIDP was eventually reached. 15 of these met our criteria for A-CIDP, but only 13 had a CSF study at the time of the acute presentation. These 13 cases were analyzed separately from the main GBS-spectrum cohort.
For the clinical classification, 173 patients were divided into 134 SM-GBS, 13 M-GBS, 8 L-GBS, and 18 MFS (Table 1). Mean CSF-TP was highest for SM-GBS (1.30 g/L), with much lower values for M-GBS (0.60 g/L) and MFS (0.73 g/L). These differences were significant with the ANOVA (p = 0.0484) but the significance was lost when adding factors of age, sex, and time-to-LP.
Mean WBC values were within normal limits (range 1.5–3.2), the highest individual value being 31. There was no significant correlation of CSF-TP with patient’s age or sex. A-CIDP cases had a significantly longer mean interval between symptom onset at LP (mean of 19.8 days), compared to the other GBS-spectrum categories. This likely reflected a more gradual or less distinct onset for patients in the A-CIDP category. The mean CSF-TP value did not differ significantly between A-CIDP and SM-GBS, even with correction for different time-to-LP.
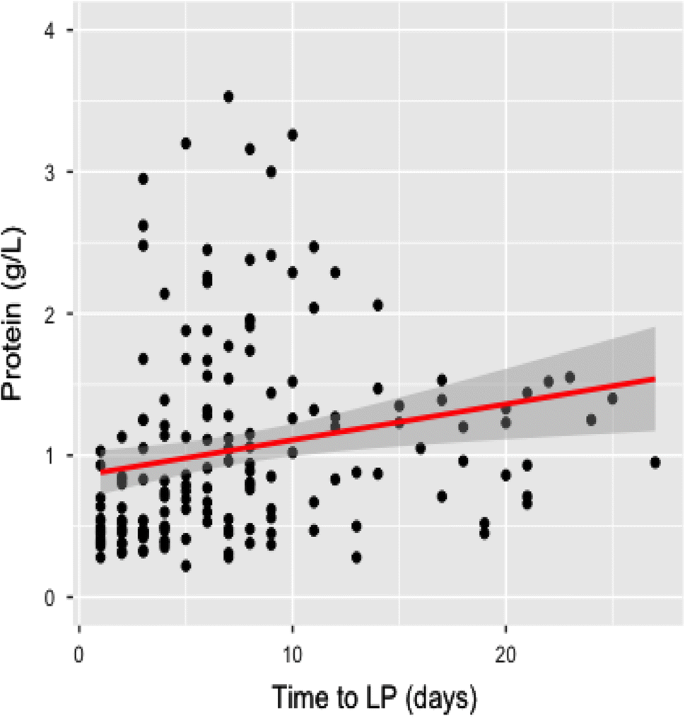
For the 173 cases of acute immune neuropathy, Fig. 1 shows a plot of CSF-TP against time-to-LP. Longer time-to-LP was correlated with higher CSF-TP values (adjusted R-squared value of 0.064).
Correlation of CSF-TP value with Time-to-Lumbar Puncture. Tukey’s rule was used to exclude 4 outlier values. The Ordinary Least Squares estimate of the relationship between time-to-LP is plotted in red and the 95% prediction interval is shown in grey. There is a statistically significant positive correlation (adjusted R-squared 0.064, p value 0.0004) but the linear model fails to describe most of the CSF-TP variability
The correlation between CSF-TP and maximal Hughes modified GBS disability scale for all 173 cases of GBS and MFS is described in Table 2. There were 102 cases in categories 1–3 and 71 cases in categories 4–6. There was a significantly higher mean CSF-TP for categories 4–6 (with correction for age and sex), while the time-to-LP was not statistically different between these two groups. An electrophysiological pattern of demyelination was found in 57% of Hughes categories 1–3 (ambulatory) compared to 76% of Hughes categories 4–6 (non-ambulatory).
In the correlation of CSF-TP and EMG pattern, there were 97 GBS cases classified as primarily demyelination (CSF-TP mean 1.56 g/L, SD 1.41), 20 cases classified as primarily axonal motor or sensorimotor (CSF-TP 0.68 g/L SD 0.28) and 49 cases classified as normal/mild equivocal (CSF-TP 0.65 g/L, SD 0.44). The ANOVA did reveal a high degree of significance after adjusting the model to compare demyelinating to either the axonal or normal/mild non-specific groups (p = 0.0000006). Overall this model using purely electrographic classification (AIC = 506) was superior to the clinical classification model (AIC = 540). Notably, disease severity did not clearly aid in explaining CSF-TP discrepancies using this model (p = 0.25). An association was then drawn between greatest disease severity measured and electrographic demyelination (p = 0.009).
Discussion
In this study, we sought to determine whether there is a relationship between the degree of rise in CSF-TP and the subtype of acute immune neuropathy.
The purely clinical classification suggests that MFS and predominant motor forms of GBS have lower mean CSF-TP in the range of 0.6–0.73 g/L compared to sensorimotor or localized onset forms of GBS, with CSF-TP in the range of 1.14–1.30 g/L.
The most conclusive distinction was however reached when comparing acute neuropathy based on electrophysiology alone, with a highly statistically significant and more than two-fold elevation of CSF-TP for the primarily demyelinating group compared to both the primarily axonal and the normal/equivocal groups. The overall trends appear to parallel the current hypotheses about pathophysiology of GBS-spectrum disorders, whereby demyelinating GBS (acute inflammatory demyelinating polyneuropathy) can be distinguished from subtypes featuring early axonal degeneration (AMSAN) or selective targeting of the nodal/paranodal region (AMAN, MFS). Higher CSF-TP in GBS with demyelination could result from several mechanisms: disruption and release of myelin proteins from spinal root axons, greater intrathecal antibody synthesis, or a more prominent disruption of the blood-nerve barrier at the level of the spinal roots. More specific CSF protein analyses would be required to make this distinction.
In the case of MFS, a review of the literature up to 1992 identified albuminocytologic dissociation in 64.4% of cases [12]. In a population from Taiwan, Lyu found a similar proportion of 58% of MFS having raised CSF-TP compared with a higher rate of 81%in GBS [13]. A very large study grouping data from four Asian centers also showed CSF-TP more frequently elevated in GBS cases (56%) compared to MFS (38%) [14]. In a study from Japan with a mean age of 50 years, CSF-TP was raised in 25% and 71% in first and second weeks in MFS, compared to 44% and 67% for GBS [15]. Thus, the limited literature does not provide rigorous statistical data to conclude that CSF-TP is significantly lower in MFS compared to AIDP.
In our 173 patients representing all categories of GBS (including MFS), the magnitude of the CSF-TP rise was a significant but weak predictor of subsequent peak disability measured by the modified Hughes GBS disability scale. There was a small but statistically significant relative elevation when comparing the 102 patients who remained ambulatory (Hughes 1–3, mean CSF-TP 1.01 g/L) to the 71 patients who were non-ambulatory or required mechanical ventilation (Hughes 4–6, mean CSF-TP 1.43 g/L). The statistical analysis however suggests that demyelinating electrophysiology may be the dominant factor in this distinction.The lack of correlation of CSF-TP with age and sex in this study likely reflects the small size of our cohort (173 samples) compared to much larger normative reference studies [16, 17]
The rise in CSF-TP in acute immune polyradiculoneuropathy is due to a combination of increased capillary permeability at the level of the blood-nerve barrier and intrathecal immunoglobulin production. The historical term “albuminocytologic dissociation” is misleading as it does not reflect the rich proteomic repertoire captured under the single laboratory measure of “total protein”. In addition, the rise in CSF-TP is a dynamic process, with a sensitivity of 50% or less in the first week of GBS, particularly if modern age-dependent reference values are applied [4]. The effect of the time interval to lumbar puncture is likely to have a greater impact on the CSF-TP value than the potential effect of disease severity we documented. Many practical and poorly controllable clinical factors influence the timing of lumbar puncture in relation to the onset and clinical progression of GBS. This may negate the potential usefulness of CSF-TP as a predictor of GBS disability grade.
We did not find that the rise in CSF-TP at the time of initial presentation was helpful in predicting patients destined to subsequently be categorized as CIDP. A previous study focussing on distinguishing A-CIDP from patients with GBS with treatment-related fluctuations had relatively small numbers in both groups [18]. Increased CSF-TP (defined as > 0.55 g/L) was found in10/16 (63%, mean value 0.9 g/L) of patients with fluctuating GBS, compared to 4/8 (57%, mean value 0.7 g/L) of patients with A-CIDP. In the study of Alessandro, there was no statistically significant difference in the frequency of ACD in AIDP (93%, mean CSF-TP 0.80 g/L) and A-CIDP (72%, mean 1.14 g/L) [19]. The average interval between symptom onset and lumbar puncture was much longer in A-CIDP (28 days) compared to AIDP (9 days), a factor that by itself might tend to favor higher CSF-TP values for the A-CIDP group. Similarly, in a retrospective study from Canada, there was no difference in CSF-TP mean values between 20 patients with A-CIDP (1.36 g/L) and 28 patients with AIDP (1.39 g/L) [20].
Several limitations must be acknowledged in our study. Consistent with clinical practice, there is variation in the time between symptom onset and lumbar puncture. We chose a broader range of clinical symptoms (including prominent paresthesia) to determine the time of GBS onset, whereas the literature has typically limited this definition to the occurrence of clinical weakness. Our onset criteria appeared more practical for a retrospective chart review, but could lead to an earlier onset timepoint. Our adjudication of clinical GBS categories can only be considered a “most likely category”. Retrospective data acquisition is rarely uniform, both from the point of view of clinical documentation and timing/detail of electrophysiologic studies.The main laboratory measure analyzed is CSF-TP, which may be only a crude and non-specific measure of abnormal blood-nerve barrier permeability or intrathecal antibody production. More targeted assessments could include the CSF/Serum Albumin ratio (QAlb), the presence of oligoclonal bands, or specific titers, such as anti-ganglioside antibodies.
A raised CSF-TP remains a useful laboratory diagnostic criterion for GBS, with sensitivity exceeding 80% by the second week. Our series shows trends for higher absolute CSF-TP values in the classical SM-GBS and L-GBS compared to MFS and M-GBS. The weak correlation of CSF-TP and GBS peak disability may be of pathophysiological relevance, but it could not be used to alter management plans in this very dynamic and potentially life-threatening clinical syndrome.The strongest association with higher CSF-TP was a demyelinating electrophysiological pattern. This finding may bolster the rationale of progressing from a purely clinical characterization of GBS to a classification algorithm that may include not only electrophysiological results, but eventually also CSF proteomics and specific markers of the immunological response.
References
van den Berg B et al (2014) Guillain-Barre syndrome: pathogenesis, diagnosis, treatment and prognosis. Nat Rev Neurol 10(8):469–482
Fokke C et al (2014) Diagnosis of Guillain-Barre syndrome and validation of Brighton criteria. Brain 137(Pt 1):33–43
Willison HJ, Jacobs BC, van Doorn PA (2016) Guillain-Barre syndrome. Lancet 388(10045):717–727
Bourque PR, Brooks J, McCudden CR, Warman-Chardon J, Breiner A (2019) Age matters: impact of data-driven CSF protein upper reference limits in Guillain-Barré syndrome. Neurol Neuroimmunol Neuroinflamm 6:e576 (In press)
Wakerley BR, Uncini A, Yuki N (2014) Guillain-Barre and Miller Fisher syndromes–new diagnostic classification. Nat Rev Neurol 10(9):537–544
Van der Meche FG et al (2001) Diagnostic and classification criteria for the Guillain-Barre syndrome. Eur Neurol 45(3):133–139
Rajabally YA et al (2015) Electrophysiological diagnosis of Guillain-Barre syndrome subtype: could a single study suffice? J Neurol Neurosurg Psychiatry 86(1):115–119
Hughes RA et al (1978) Controlled trial prednisolone in acute polyneuropathy. Lancet 2(8093):750–753
Group, P.E.S.G.-B.S.T (1997) Randomised trial of plasma exchange, intravenous immunoglobulin, and combined treatments in Guillain-Barre syndrome plasma exchange/sandoglobulin Guillain-Barre syndrome trial Group. Lancet 349(9047):225–230
Wilkinson GN, Rogers CE (1973) Symbolic description of factorial models for analysis of variance. J R Stat Soc Series C (Appl Stat) 22(3):392–399
Fox J, Weisberg S (2018) An R companion to applied regression. Sage, Los Angeles
Berlit P, Rakicky J (1992) The Miller Fisher syndrome review of the literature. J Clin Neuroophthalmol 12(1):57–63
Lyu RK et al (1997) Guillain-Barre syndrome in Taiwan: a clinical study of 167 patients. J Neurol Neurosurg Psychiatry 63(4):494–500
Wong AH et al (2015) Cytoalbuminologic dissociation in Asian patients with Guillain-Barre and Miller Fisher syndromes. J Peripher Nerv Syst 20(1):47–51
Nishimoto Y et al (2004) Usefulness of anti-GQ1b IgG antibody testing in Fisher syndrome compared with cerebrospinal fluid examination. J Neuroimmunol 148(1–2):200–205
Hegen H et al (2016) Upper reference limits for cerebrospinal fluid total protein and albumin quotient based on a large cohort of control patients: implications for increased clinical specificity. Clin Chem Lab Med 54(2):285–292
McCudden CR et al (2017) Cerebrospinal fluid total protein reference intervals derived from 20 years of patient data. Clin Chem 63(12):1856–1865
Ruts L, van Koningsveld R, van Doorn PA (2005) Distinguishing acute-onset CIDP from Guillain-Barre syndrome with treatment related fluctuations. Neurology 65(1):138–140
Alessandro L et al (2018) Differences between acute-onset chronic inflammatory demyelinating polyneuropathy and acute inflammatory demyelinating polyneuropathy in adult patients. J Peripher Nerv Syst 23(3):154–158
Dionne A, Nicolle MW, Hahn AF (2010) Clinical and electrophysiological parameters distinguishing acute-onset chronic inflammatory demyelinating polyneuropathy from acute inflammatory demyelinating polyneuropathy. Muscle Nerve 41(2):202–207
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors of this manuscript have no conflicts of interest to disclose.
Ethical standard
This study was approved by the Institutional Ethics (Medical Research) Committee.
Rights and permissions
About this article
Cite this article
Bourque, P.R., Brooks, J., Warman-Chardon, J. et al. Cerebrospinal fluid total protein in Guillain–Barré syndrome variants: correlations with clinical category, severity, and electrophysiology. J Neurol 267, 746–751 (2020). https://doi.org/10.1007/s00415-019-09634-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09634-0