Abstract
Objective
Chronic inflammatory demyelinating polyneuropathy (CIDP) is a rare, autoimmune-inflammatory disease of the peripheral nervous system. Recently, various immunoglobulin G4 (IgG4) type auto-antibodies have been described in patients with CIDP which can effectively be removed by immunoadsorption (IA). Therefore, we prospectively evaluated the therapeutic effect of IA in 17 patients with progressive CIDP not responding to other treatment.
Methods
We prospectively evaluated the course of disease of 17 patients with CIDP who had insufficiently responded to steroids and/or IVIg previously and who received at least one cycle of IA. As clinical outcome parameter, we used a combined CIDP score of three validated scales comprising disability, motor score, and sensitivity. Seven patients received repeated treatments in regular intervals over a prolonged period up to 46 months.
Results
We observed a small, but significant improvement of the overall score after 2 weeks that mainly reflected an improvement of muscle strength. The median value of the combined CIDP score was 308.0 (266.0–374.5) points before IA and 330.0 (290.0–393.5) points 2 weeks after IA (p = 0.019). More importantly, all but one of seven progressive patients who received long-term immunoadsorption in regular intervals stabilized almost completely. Before IA, these patients lost 6.7 (3.0–13.1) points of combined CIDP score per month. During IA, they lost − 0.1 (0.0–0.8) points per month (p < 0.0001).
Interpretation
Our results suggest that IA might constitute a promising and well-tolerated therapeutic alternative in CIDP for short-term and long-term treatment. We showed that long-term treatment with IA in regular intervals can stabilize the course of disease at least in a subgroup of patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic inflammatory demyelinating polyneuropathy (CIDP) is a rare autoimmune-inflammatory disease which mainly affects the myelin sheaths of peripheral nerves, leading to paresis and sensory deficits. Clinical presentation varies greatly among patients. While the typical clinical phenotype shows the symmetrical distribution of motor and (in > 50%) sensory symptoms, about half of the patients display variants with pure motor or pure sensory deficits as well as asymmetric manifestations. The course of disease is chronically progressive in most cases, but can rarely be relapsing, as well.
Therapy of CIDP includes treatment with steroids (evidence class Ib), intravenous immunoglobulines (IVIg, Ia), plasma exchange (PE, Ib), and a variety of immunosuppressive drugs (IV), most notably azathioprine and rituximab. Since the individual response to different options varies greatly among patients, no unanimously accepted guidelines or therapeutic schemes exist. The European Federation of Neurological Societies (EFNS) guidelines suggest to begin with steroids or IVIg as non-invasive options which are easy to apply, and to use plasma exchange in case of insufficient therapeutic response [1]. Long-term immunosuppressive agents are used if a long-lasting effect cannot be achieved with the above-mentioned therapies or to lower steroid dosages. Therefore, therapy of CIDP is rather pragmatic than specific, and in many cases, different therapeutic schemes have to be tried before an effective approach is found for the individual patient.
Considering the great variety regarding clinical presentation and response to different immune-modulating therapies, many experts consider CIDP as a syndrome or a group of diseases rather than a specific disease entity. This hypothesis gained further acceptance when various specific auto-antibodies against proteins of the node of Ranvier and the paranodal region were identified in about 15–20% of patients with CIDP [2], defining a new subcategory of “nodo-/paranodopathies” within CIDP. Importantly, all recently identified antibodies against nodal and paranodal proteins belong to the IgG4 isotype which have distinct immunological characteristics resulting in important therapeutic implications. IgG4 antibodies do not bind complement which might explain the uniformly reported observation that CIDP patients with paranodal antibodies respond poorly to IVIg [3], since the effect of IVIg in autoimmune diseases is at least partly complement-mediated [4]. Following this hypothesis, therapies which prevent antibody generation and/or effectively remove those antibodies from the blood should have a great positive therapeutic effect. Accordingly, previous case series consistently report a beneficial effect of rituximab and PE [3].
Immunoadsorption (IA) is a highly effective and well-tolerated alternative to remove IgG4 auto-antibodies from the blood. Like in plasma exchange (PE), the patient’s blood is separated into cells and plasma. While, in PE, the plasma is replaced by a substitution fluid, in IA, the plasma runs through adsorber systems which selectively bind human immunoglobulines before it is returned to the patient. Therefore, in contrast to PE, all other plasma proteins like coagulation factors are largely preserved [5] which allows higher treating frequencies and higher plasma volumes to be processed, resulting in a greater share of removed immunoglobulines. For the same reason, adverse events in PE which are based on the loss of plasma proteins (like bleeding complications due to the loss of coagulation factors) are extremely rare in IA; therefore, IA is generally considered as a low-risk therapy. Furthermore, in contrast to PE, no substitution solutions like human albumin solutions or fresh frozen plasma are needed in IA; therefore, the risk of allergic reactions is reduced. Susceptibility to infections due to the almost complete removal of immunoglobulins is regarded as the main risk of IA, although it is rarely seen in practice. In summary, a better tolerability of IA compared to PE is regarded as one of the main advantages of IA and has been demonstrated in clinical studies of other autoimmune neurological diseases like myasthenic crisis [6], albeit not in CIDP [7]. On the other hand, a possible disadvantage of IA compared to PE is that other pro-inflammatory proteins like interleukin-1 (IL1), interleukin-6 (IL6), tumor necrosis factor alpha (TNFα), and many others are also preserved in IA. However, as outlined above, this might not be critical in IVIg-refractory CIDP as the pathogenic effect might largely depend on the IgG4 antibodies themselves. Of note, just like IVIg and PE, IA does not offer long-lasting therapeutic effects in chronic autoimmune diseases, since the respective auto-antibodies will reappear eventually. Besides the direct therapeutic effect via the removal of auto-antibodies, further proposed mechanisms of action of IA include induction of auto-antibody redistribution and subsequent immunomodulatory changes [8].
Considering these aspects, IA constitutes a logical therapeutic option for steroid- and IVIg-refractory CIDP patients. However, evidence for the use of IA in CIDP is extremely low, especially since there are no studies at all which investigate the long-term effects of repeated IA. Therefore, in this study, we aimed at evaluating short- and long-term effects of IA in CIDP in a prospective and standardized manner by performing well-elaborated clinical scores at predefined time points.
Methods
Study design and participants
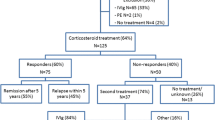
The study was conducted at the Department of Neurology of the University Hospital of Ulm. Over a time period of 4 years (December 2013 until January 2018), 17 patients [13 males, 4 females, and age 64.0 (58.0–66.0)] were included in the study. Patient’s characteristics are outlined in Table 1. All patients fulfilled the EFNS criteria for possible, probable, or definite CIDP, had a continuously progressive course of disease, and had previously received several cycles of steroids (n = 5), IVIg (n = 2) or both (n = 10) with insufficient response. Twelve patients who had previously received IVIg had shown further disease progression under IVIg therapy; therefore, we opted for a new therapeutic approach with IA. In 5 patients who had never received IVIg, we chose IA instead of IVIg based on our favorable clinical experience with IA in CIDP. Two patients had never been treated with prednisolone because of severe diabetes mellitus. Further treatments included azathioprine (n = 4), cyclophosphamide (n = 1), mycophenolatmofetil (n = 2), and methotrexate (n = 1).
Importantly, the disease duration varied greatly [68.0 (47.5–96.0) months]; only one patient had a disease duration < 2 years, and only two patients had a disease duration < 3 years.
Seven of 17 patients received several cycles of IA. We applied the concept of repeated IA only to patients with therapy-refractory courses of disease and reasonable short-term results after the first IA cycle. Of this subgroup, one patient received nine cycles of immunoadsorption, one patient received five cycles, one patient received four cycles, three patients received three cycles, and one patient received two cycles. The interval between two cycles was chosen individually, based on the time when improvement stagnated and symptoms began to worsen again. Accordingly, intervals between IA cycles varied between 6 weeks and 6 months.
Procedures
One cycle of IA consisted of five treatments on 5 consecutive days. The total plasma volume of each patient was calculated using body weight, height, and hematocrit. The twofold total plasma volume was processed during the first treatment, and the 2.5-fold total plasma volumes were processed during all the subsequent treatments. The Adsorber system (ADAsorb, medicap clinic GmbH, Ulrichstein, Germany) contained two regenerating protein A columns (Immunosorba, Fresenius Medical Care, Bad Homburg, Germany). In contrast to single-use adsorbers (e.g., tryptophan adsorbers), regenerating adsorbers allow multiple uses of each column, resulting in greater blood volumes which can be processed during each treatment. In regenerating systems, two columns undergo alternating loading and regeneration cycles to save time. Protein A is a cell wall protein of staphylococcus aureus which highly selectively binds human immunoglobulins.
Since IA requires high blood flow volumes to achieve the desired blood volumes to be treated, we opted for a Shaldon catheter which was placed in the jugular vein. Although more invasive compared to a peripheral venous access, a Shaldon catheter offers higher blood flow volumes which lead to shorter treatment durations, greater stability, less technical complications, and greater freedom for the patients during and between IA sessions. Heparin and citrate were used as anticoagulants. We did not use prophylactic antibiotics and did not substitute immunoglobulins after the therapy. Potassium and protein were substituted, since hypokalemia and hypoproteinemia are common phenomena in IA practice.
Since there is a little evidence about the use of IA in CIDP, patients were monitored carefully before, during, and after IA. Laboratory data (blood count, coagulation factors, electrolytes, and C-reactive protein) were collected before and daily during IA to control for infections, coagulation disorders, and electrolyte disturbances. Urinary tract infection was ruled out before IA by urinary status, and ACE inhibitors were paused, since severe, bradykinine-mediated fluctuations of blood pressure have been reported for patients with ACE inhibitors. During IA, heart rate, blood pressure, respiratory frequency, and oxygen saturation were continuously monitored. All IA sessions were performed in the apheresis center of the Neurological Department of Ulm University and all patients were hospitalized during the IA therapy.
Outcome parameters
The baseline investigation was performed 3 days before the first IA. At baseline and 2 weeks after IA, three standardized clinical scales were performed: The Inflammatory Neuropathy Cause and Treatment (INCAT) disability score [9] constitutes the standard clinical score for CIDP and consists of two items (arm and leg function). The score of each item ranges from 0 to 5 points, resulting in a maximum sum score of 10. Although the INCAT is widely accepted and applied easily, it only allows a rather rough quantification of the disability status and does not detect smaller clinical changes which might still be relevant for the patient’s well-being [10].
Since paresis constitutes the most common symptom in CIDP, we also applied the Oxford muscle strength grading scale (Medical Research Council, MRC) which is a standard scale for the quantification of muscle strength in neurological examination and has been used as a validated tool in a wide variety of clinical studies. Muscle strength is evaluated on a scale between 0/5 (no movement) and 5/5 (full strength). In this study, eight predefined muscles (one proximal and one distal muscle at each extremity) were tested, resulting in a maximum sum score of 40. The MRC score allows a finer graduation of motoric symptoms compared to the INCAT, although, amongst others, it has been criticized for its poor discrimination between grades 4 and 5. INCAT and MRC (together with grip strength) were the strongest explanatory variables of disability in a randomized-controlled trial which investigated the efficacy of IVIgs in CIDP [11].
Finally, sensory symptoms are present in > 50% of patients with CIDP, although generally incriminating, they are not adequately incorporated in the INCAT score. Therefore, we used the vibration sensitivity testing with a 256-Hz Ryder-Seiffel tuning fork which also constitutes a standard evaluation tool in neurological examination. The testing allows to determine the individual perception threshold for vibration sensations on a scale between 0/8 (no perception) and 8/8 (normal perception). Vibration sensitivity testing (VIB) was performed at four predefined spots (processus styloideus and malleolus lateralis on each side), resulting in a maximum sum score or 32.
We subsequently calculated an overall CIDP score ranging from 0 to 480 including all three aforementioned scales. To weigh all three subscores equally, we multiplied the MRC score by 4, the INCAT score by 16, and the vibration score by 5, so that every subscore had a maximum of 160 points. For patients who received two or more IA cycles, we calculated the progression rate per month by dividing their total loss of CIDP score until baseline by their disease duration in months. Under regular IA therapy, we recorded the CIDP score before and 2 weeks after each cycle and calculated the progression rate by dividing the loss of CIDP score between the first and last visit divided by the months between them.
Statistical analysis
Standardized outcome parameters were collected in hospital 3 days before the first and 14 days after the last IA treatment of each cycle. Adverse events were recorded by anamnesis, clinical examination, and monitoring data as described above.
To compare outcome parameters (change of CIDP score and subscores) before and after IA, the non-parametric Wilcoxon signed-rank test for dependent variables was used. All data are given as median and interquartile range. To test for normality, the D’Agostino–Pearson test was applied. The level of significance was set at p = 0.05. For statistical analyses, SPSS Statistics 21 (IBM) was used.
Role of the funding source
There was no funding for this study. JD had access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Tolerability
In total, n = 39 cycles (= 195 treatment sessions) were performed. One pneumothorax occurred after Shaldon placement. The same patient later developed a thrombosis of the jugular vein. Since this patient responded very well to immunoadsorption and received multiple cycles over several years, we later opted for a permanent solution via a cubital arteriovenous shunt. One further thrombosis of the jugular vein occurred in another patient, and one patient developed a febrile infect.
Minor side effects included mild edema (n = 2), dislocation of catheter (n = 1), bradycardia (n = 1), tachycardia (n = 1) hypotonia (n = 2), urinary tract infection (n = 1), gastrointestinal infection (n = 1), and exanthema of the face (n = 1), the latter most likely related to a mild heparin allergy. Hypotonia, bradycardia, and tachycardia are frequently seen during apheresis due to changes in blood pressure which are caused by volume shifts and/or vasovagal reactions caused by Shaldon catheter placement.
Common subclinical laboratory changes included mild anemia, thrombocytopenia, hypokalemia, hypocalcemia, hypoproteinemia, and increase of CRP.
Short-term effects
Two weeks after the first cycle (= five treatments) of IA, we found an improvement of the combined CIDP score on group level from 308.0 (266.0–374.5) to 330.0 (290.0-393.5), which was statistically significant (p = 0.019, Fig. 1). Overall, 11/17 patients improved. The median MRC improved significantly from 33.0 (28.5–37.5) to 37.0 (30.0–38.0; p = 0.029, Fig. 2). The median vibration score improved, as well, but not significantly. Although five patients improved in the INCAT, the median INCAT did not change significantly. Medians, interquartile ranges, and p values for each score are given in Table 2.
Short-term effect of IA on combined CIDP score. Boxplots show the combined CIDP score (COM, comprising INCAT disability score, MRC, and vibration sensitivity) before and 2 weeks after IA (n = 17). The combined CIDP score improved from 308.0 (266.0–374.5) before IA to 330.0 (290.0–393.5) 2 weeks after IA (p = 0.019). Numbers (outliers) correspond to respective patient’s IDs of Table 1
Two patients showed particularly great improvements of 130 and 85 points in the combined score, respectively. These two patients showed different phenotypes: The first patient (#8 in Table 1), a 60-year-old male, had a classical CIDP syndrome with symmetrical and proximal pronounced paresis of arms and legs with sensory involvement, but no additional symptoms. He showed an aggressive course of disease, considerable axonal involvement in electrophysiology. He had not been treated with prednisolone due to severe diabetes mellitus, and did not respond to IVIg. He improved considerably after IA and was able to walk without walking stick which was not possible before IA.
The second patient, a 58-year-old male (#14), suffered from asymmetric, proximal and distal paresis of arms and legs, severe sensory symptoms (hypesthesia, dysesthesia, pain), and tremor. After IA, this patient showed considerable improvement of function of arms and legs, resulting in significantly reduced demands of care during daily life activities.
Both phenotypes have recently been associated with distinct paranodal IgG4 auto-antibodies, the former with anti-Contactin-1, the latter with anti-NF155 [2].
Two other patients (#2 and #7) showed an improvement of walking and a significant reduction of neuropathic pain with the reduced demands of analgesic drugs, respectively.
Long-term effects
Out of the 17 patients, 7 patients received two or more IA cycles, up to a maximum of 9 cycles in one patient. Treatment periods and frequencies varied among these patients. Usually, they showed an improvement after IA, and the next IA cycle was performed when symptoms began to worsen again. Time intervals between two IA cycles ranged between 6 weeks and 6 months, and the largest overall treatment period was 46 months.
All 7 patients had previously shown a rapidly progressive disease and had been treated with steroids, IVIg, and in some cases with additional immunosuppressive agents like azathioprine, methotrexate, mycophenolatmofetil, or cyclophosphamide without sufficient response.
On group level, the progression rate decreased from 6.7 (3.0–13.1) points of CIDP score per month to 0.1 (0.0–0.8) points per month which was highly significant (p < 0.0001, Fig. 3). On an individual level (Fig. 4), only one patient remained at a progression rate > 1 point/month. Because 6/7 patients stabilized almost completely, we terminated the immunosuppressive therapy which was present in 3 of these patients (2× azathioprine, 1× cyclophosphamide); so far, we still did not see any further signs of disease progression.
Long-term effect of IA on group level. Boxplots show the progression rates (loss of combined CIDP score per month) before and during regular IA treatment in patients who received at least two cycles of IA (n = 7). The progression rate improved from 6.7 (3.0–13.1) per month before IA to 0.1 (0.0–0.8) per month during IA (p < 0.0001). Numbers (outliers) correspond to respective patient’s IDs of Table 1
Long-term effect of IA on individual levels. Colored lines represent the development of the combined CIDP scores in all seven individual patients over time. The patient’s number corresponds to the patient’s ID of Table 1. Colored dots represent the points of time when the CIDP score was measured. The black vertical line marks the beginning of IA. Before regular IA was established, all patients had shown a significant disease progression (left half of diagram). Because the CIDP score had not been measured before the beginning of IA, we assumed a simplified linear decline of the combined CIDP score. During regular IA treatment (right half of diagram), all but one patient (#12) showed an almost complete stabilization without any disease progression, although clinical fluctuations occurred as depicted
One patient remained stable under regular IA therapy, but symptoms began to worsen sooner after each therapy, leading to increasingly shorter treatment intervals. Based on the hypothesis of a primarily antibody-mediated pathomechanism, we, therefore, started a B-cell depleting therapy with rituximab, under which we were able to extend the treatment intervals again.
IgG reduction
Total serum IgG levels were measured immediately before the first and after the last IA treatments of each cycle. On group level, IgG serum levels were reduced from 7885.0 mg/l (6712.5–10325.0 mg/l) to 385.0 mg/l (300.3–462.3 mg/l), equaling a median reduction of 95.2%, which was highly significant (p < 0.0001, Fig. 5). On an individual level, IgG reduction ranged from 92.8 to 96.8%.
Serum IgG levels. Boxplots show serum levels of IgG immediately before the first and after the last IA treatments of each cycle (n = 39). Serum IgG levels decreased from 7885.0 mg/l (6712.5–10325.0 mg/l) before the first treatment to 385.0 mg/l (300.3–462.3 mg/l) after the last treatment, equaling a median reduction of 95.2% (p < 0.0001). Numbers (outliers) correspond to respective patient’s IDs of Table 1
Discussion
In this study, we investigated a new therapeutic approach by treating refractory CIDP patients with repeated IA. Although the IA procedure itself was not associated with any significant side effects, two patients suffered from complications related to Shaldon catheter placement. Because of its invasive nature and its limited evidence level, IA is currently regarded as a second-line alternative for most of the neurological autoimmune-inflammatory diseases with the exception of autoimmune encephalitis, in which it is generally regarded as a first-line therapy option. However, since a subgroup of CIDP patients do not respond sufficiently to steroids and IVIgs and since the crucial importance of autoimmune antibodies has recently been demonstrated at least in a subgroup of CIDP patients [2], IA can be considered as a low-risk therapeutic alternative to PE.
Our data show that serum IgG levels were effectively reduced by IA. However, clinical short-term responses vary greatly among patients. While 2 of 17 patients improved greatly, most patients only showed a small positive effect, and 6 patients did not improve at all. The improvement of the combined CIDP score can mainly be attributed to the improvement of muscle strength (MRC) which increased significantly after IA. However, the effect was not large enough to induce a significant improvement of disability status (INCAT).
When interpreting this result, the following aspects have to be considered:
First, as outlined above, CIDP is currently regarded as a syndrome which most likely contains several distinct disease entities deriving from different autoimmune pathomechanisms. This hypothesis has recently been supported by the detection of specific auto-antibodies in a subgroup of patients which are linked to very specific clinical phenotypes as well as specific responses to different immune-modulating therapies. Therefore, the existence or non-existence of a specific immunological subtype may have influenced the response to IA. As outlined above, the patients with best clinical response represent clinical phenotypes which have been connected to paranodal IgG4-auto-antibodies which can effectively be removed by IA.
Second, since CIDP is a heterogenous disease, the natural course of disease varies greatly among patients, from rather stable to the extent of rapid-progressive courses. Therefore, the therapeutic benefit has to be judged on an individual basis. For example, a stabilization of symptoms for several weeks or months can be regarded as a success in some patients.
Third, the majority of our patients had been diagnosed several years ago, had responded insufficiently to a variety of different immune-modulating and immunosuppressive agents, and had acquired irreversible axonal damage over time. Therefore, we can assume that a selection bias is present in our sample and that the therapeutic effect might be considerably better at an early stage of the disease. However, this hypothesis has to confirmed by an appropriate randomized-controlled trial (RCT).
To date, there are very few clinical studies which investigated the efficacy of IA in CIDP. One recent RCT [7] compared the effect of IA and PE in 20 patients with CIDP. Similar to our study, the clinical response was measured by INCAT disability score and MRC score. The authors found that, after 4 weeks, 6/9 patients (66.7%) had improved clinically with IA, but only 4/9 (44.4%) with PE and concluded that IA was at least equally effective compared to PE. Therefore, the short-term response rate was similar to the response rate in our study (11/17, 64.7%). Another case series in therapy-refractory CIDP patients found an even higher response rate of IA (13/14, 92.9%) [12]. As outlined above, the use of different adsorber systems as well as the heterogeneity of patients regarding immunological subgroups, natural progression rates, and time since onset can sufficiently explain the diverging results. In particular, both aforementioned studies used tryptophan one-time adsorbers instead of regenerating protein A adsorbers, and none of the studies performed specific antibody diagnostics. Most importantly, the patients in this study had a much longer disease duration (mean 6.3 ± 3.0 years) compared to both other studies (3.1 ± 2.3 years [7]). To date, there are no studies comparing IA with steroids or IVIg.
Our study is the first to prospectively investigate the long-term effects of regular IA in CIDP up to several years of observation. To evaluate the therapeutic effect, we compared the clinical progression rates as described above, with a simplified assumption of a linear decline of the combined CIDP score before baseline.
Surprisingly, we found that 6/7 (85.7%) patients did not show any relevant disease progression anymore under regular IA. In these patients, this stabilization even persisted after the termination of immunosuppressive co-medication. The only other study which investigated the effect of multiple IAs over a prolonged time period [13] found a better response rates for regular IA compared to IVIg after 2 and 6 months. Therefore, we can assume that (comparable to the application of IVIg) IA can be used in regular individualized time intervals to continuously remove pathogenic auto-antibodies and prevent further axonal damage in a subgroup of patients with CIDP. However, due to its invasive nature, IA is likely to remain a second-line therapy option as long as a superiority to non-invasive therapies is not proven by an adequate RCT.
The following limitations of the study have to be mentioned: The data were derived from a standard clinical setting; therefore, evaluators were not blinded, and data cannot be supported by neurophysiology, since it was not routinely performed at every visit. Furthermore, nodal and paranodal antibodies were not tested; therefore, the pathophysiological concept for IA cannot be proven directly by this study. In addition, since five patients had not received either prednisolone or IVIgs prior to IA treatment, we cannot rule out that these patients would have responded to a first-line treatment option.
Summary
In summary, our results show that
-
1.
IA itself is well-tolerated, although a few complications may occur due to the need of Shaldon catheter placement.
-
2.
IgG antibodies can effectively be removed by IA.
-
3.
Most patients show only mild short-term improvements, but a specific small subgroup might receive a large benefit.
-
4.
Regular long-term IA might stabilize disease progression in a subgroup of therapy-refractory patients.
Overall, our data show that clinical response to IA may vary greatly among patients, supporting the view of different pathophysiological and immunological mechanisms currently subsumed within the diagnosis of CIDP. Future clinical studies must, therefore, focus on establishing a differential therapy for distinctive CIDP subforms. In particular, the following specific issues have to be addressed:
-
1.
how to identify patients who respond well to IA, i.e., whether or not this subgroup corresponds to patients with nodal/paranodal IgG4 auto-antibodies.
-
2.
to perform sufficiently powered RCTs to validate short- and long-term effects of IA, not only compared to PE but also to IVIg and steroids.
In conclusion, our data suggest that IA might offer a low-risk therapeutic option which may stabilize the course of disease in otherwise therapy-refractory CIDP patients. However, the sample size in this study was low, and the hypotheses generated by this pilot study have to be confirmed by a respective phase III RCT. Since prevalence of CIDP is low, national or international networks are likely required to recruit sufficient numbers of patients.
References
Van den Bergh PY, Hadden RD, Bouche P, Cornblath DR, Hahn A, Illa I, Koski CL, Leger JM, Nobile-Orazio E, Pollard J, Sommer C, van Doorn PA, van Schaik IN (2010) European Federation of Neurological Societies/Peripheral Nerve Society guideline on management of chronic inflammatory demyelinating polyradiculoneuropathy: report of a joint task force of the European Federation of Neurological Societies and the Peripheral Nerve Society—first revision. Eur J Neurol 17(3):356–363
Querol L, Devaux J, Rojas-Garcia R, Illa I (2017) Autoantibodies in chronic inflammatory neuropathies: diagnostic and therapeutic implications. Nat Rev Neurol 13(9):533–547
Illa I (2017) ARTHUR ASBURY LECTURE: Chronic inflammatory demyelinating polyradiculoneuropathy: clinical aspects and new animal models of auto-immunity to nodal components. J Peripher Nerv Syst 22(4):418–424
Jacob S, Rajabally YA (2009) Current proposed mechanisms of action of intravenous immunoglobulins in inflammatory neuropathies. Curr Neuropharmacol 7(4):337–342
Zollner S, Pablik E, Druml W, Derfler K, Rees A, Biesenbach P (2014) Fibrinogen reduction and bleeding complications in plasma exchange, immunoadsorption and a combination of the two. Blood Purif 38(2):160–166. https://doi.org/10.1159/000367682
Kohler W, Bucka C, Klingel R (2011) A randomized and controlled study comparing immunoadsorption and plasma exchange in myasthenic crisis. J Clin Apher 26(6):347–355. https://doi.org/10.1002/jca.20317
Lieker I, Slowinski T, Harms L, Hahn K, Klehmet J (2017) A prospective study comparing tryptophan immunoadsorption with therapeutic plasma exchange for the treatment of chronic inflammatory demyelinating polyneuropathy. J Clin Apher 32(6):486–493
Klingel R, Heibges A, Fassbender C (2009) Plasma exchange and immunoadsorption for autoimmune neurologic diseases—current guidelines and future perspectives. Atheroscler Suppl 10(5):129–132. https://doi.org/10.1016/s1567-5688(09)71827-6
Merkies IS, Schmitz PI, van der Meche FG, Samijn JP, van Doorn PA (2002) Clinimetric evaluation of a new overall disability scale in immune mediated polyneuropathies. J Neurol Neurosurg Psychiatry 72(5):596–601
Breiner A, Barnett C, Bril V (2014) INCAT disability score: a critical analysis of its measurement properties. Muscle Nerve 50(2):164–169
Merkies IS, Hughes RA, Donofrio P, Bril V, Dalakas MC, Hanna K, Hartung HP, Latov N, van Doorn PA, Deng C (2010) Understanding the consequences of chronic inflammatory demyelinating polyradiculoneuropathy from impairments to activity and participation restrictions and reduced quality of life: the ICE study. J Peripher Nerv Syst 15(3):208–215
Galldiks N, Burghaus L, Dohmen C, Teschner S, Pollok M, Leebmann J, Frischmuth N, Hollinger P, Nazli N, Fassbender C, Klingel R, Benzing T, Fink GR, Haupt WF (2011) Immunoadsorption in patients with chronic inflammatory demyelinating polyradiculoneuropathy with unsatisfactory response to first-line treatment. Eur Neurol 66(4):183–189. https://doi.org/10.1159/000331011
Zinman LH, Sutton D, Ng E, Nwe P, Ngo M, Bril V (2005) A pilot study to compare the use of the Excorim staphylococcal protein immunoadsorption system and IVIG in chronic inflammatory demyelinating polyneuropathy. Transfus Apher Sci 33(3):317–324. https://doi.org/10.1016/j.transci.2005.07.010
Author information
Authors and Affiliations
Contributions
JD did the scientific literature search, data collection, and analysis of data. JD, HT, and MS were involved in study conception and design. All authors participated in data interpretation. JD wrote the first draft of the manuscript, and all authors reviewed and critiqued the manuscript. HT and MS contributed equally to this work.
Corresponding author
Ethics declarations
Conflicts of interest
JD reports personal fees from Fresenius Medical Care GmbH and Fresenius Medical Care Deutschland GmbH, outside the submitted work. JD and HT report research and sponsoring grants from Fresenius Medical Care GmbH and Fresenius Medical Care Deutschland GmbH, outside the submitted work. MS has received honoraria for speaking and/or travel grants from Bayer, Biogen, and TEVA, and research funding from the Hertha-Nathorff-Program and University of Ulm; none related to this study. All other authors declare that they have no conflict of interest.
Ethical standards
The study has been approved by the local ethics committee and has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All patients were extensively informed about the procedure, its risks, and possible therapeutic alternatives, and gave their written informed consent.
Rights and permissions
About this article
Cite this article
Dorst, J., Ludolph, A.C., Senel, M. et al. Short-term and long-term effects of immunoadsorption in refractory chronic inflammatory demyelinating polyneuropathy: a prospective study in 17 patients. J Neurol 265, 2906–2915 (2018). https://doi.org/10.1007/s00415-018-9082-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-018-9082-6