Abstract
Background and aims
Due to common pathophysiological findings of Alzheimer’s disease (AD) with diabetes mellitus (DM), insulin has been suggested as a possible treatment of AD or mild cognitive impairment (MCI). A safe alternative of IV insulin is intranasal (IN) insulin. The aim of this systematic review is to investigate the effects of IN insulin on cognitive function of patients with either AD or MCI.
Methods
A literature search of the electronic databases Medline, Scopus and CENTRAL was performed to identify RCTs investigating the effect of IN insulin administration on cognitive tasks, in patients with AD or MCI.
Results
Seven studies (293 patients) met our inclusion criteria. Most studies showed that verbal memory and especially story recall was improved after IN insulin administration. Sometimes the effect was restricted for apoe4 (−) patients. Intranasal insulin did not affect other cognitive functions. However, there were some positive results in functional status and daily activity. Data suggested that different insulin types and doses may have different effects on different apoe4 groups. In addition, the effects of treatment on Αβ levels differed from study to study. Finally, IN insulin resulted in minor adverse effects.
Conclusions
Intranasal insulin improved story recall performance of apoe4 (−) patients with AD or MCI. Other cognitive functions were not affected, but there were some positive results in functional status and daily activity. Since IN insulin is a safe intervention, future studies should be conducted with larger doses and after proper selection of patients and insulin types.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alois Alzheimer described the first case of what would be defined as Alzheimer’s Disease (AD) over 100 years ago [1]. Recent studies have shown that the overall point prevalence of dementia due to AD among individuals older than 60 years is over 40 per 1000 persons [2]. The disease affects society both in terms of economy and of quality of life [3]. Despite the use of many different treatments, there is currently no effective way to halt the progression of the disease [4,5,6,7,8].
Diabetes mellitus (DM) is a risk factor for vascular dementia, as well as AD [9]. Moreover, the incidence of any type of dementia, including that of AD, is higher among people with DM [10, 11]. AD shares common pathophysiological abnormalities with DM, among which is insulin resistance and amyloidogenesis [12]. Due to these neuroendocrine abnormalities, AD has been characterized as “type 3 diabetes” [13]. Beta-amyloid, which is the hallmark pathologic characteristic of AD has been implicated in synapse toxicity and hippocampal neuronal damage and consequently in cognitive and memory impairment; intravenous administration of insulin alleviates these pathophysiologic effects [14, 15]. It has also previously been shown, that intravenous (IV) insulin administration improves memory in AD [16, 17]. However, the systemic side effects of IV insulin, mainly hypoglycemia, limit the safety and feasibility of this administration route. Intranasal (IN) insulin administration is a non-invasive method which delivers insulin to the brain parenchyma very rapidly and effectively, reaching cerebral concentrations 100-fold higher than intravenous delivery, bypassing the blood–brain barrier via paracellular transport [18,19,20]. IN insulin has negligible risk of systemic hypoglycemia and its potential as treatment agent in AD has been explored in clinical studies [19, 21, 22]. Furthermore, MCI is a condition that many times evolves to AD [23]. In addition, there is no current treatment for MCI, so treatment with IN insulin can involve this group of patients, too [23].
We undertook the present systematic review of randomized clinical trials, evaluating the potential beneficial effects of IN insulin on patients with either AD or mild cognitive impairment (MCI) [23]. Our primary goal was to investigate whether existing data support the use of IN insulin as a treatment option in MCI or Alzheimer’s dementia.
Methods
Protocol and registration
The protocol of our systematic review was prospectively registered on PROSPERO and can be accessed at http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016051385. We adopted the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines [24].
Eligibility criteria
We included studies according to the following eligibility criteria: (a) Double blind randomized control trials or double blind randomized cross-over studies. (b) Published in the English language up to 10/14/2017. (c) Reporting findings in humans. (d) Patients with diagnosis of either MCI or AD. (e) Patients were treated with intranasal insulin or placebo. (f) Patients were tested on memory or other cognitive domains with the use of various different assessment tools.
Information sources
Medline, Scopus and Cochrane Central Register of Controlled trials were searched for relevant published studies up to 10/14/2017.
Search
In the above databases we used the following search query: “(Intranasal insulin OR nasal insulin) AND (Alzheimer’s dementia OR Alzheimer’s disease OR Alzheimer’s OR neurodegenerative disease OR cognitive impairment OR neuroprotective OR memory OR cognition)”.
Study selection
For identification of eligible studies, two reviewers (GK, AM) searched independently, based on the inclusion criteria. Any disagreement was solved with the contribution of a third reviewer (PM) and consensus.
Data collection process and data items
Data were extracted by two reviewers (GK, AM) independently and included the following fields: Title, first author, ID, year of publication, journal, country of origin, study type, study duration, total number of participants, number of patients that assigned IN insulin and placebo, type of IN insulin administered, baseline characteristics of participants, apoe4 gene carriage status, CSF and plasma Αβ amyloid levels, primary outcomes (verbal memory, attention, executive function, response inhibition, visuospatial function, functional status, daily activity and general cognition after treatment) and secondary outcomes (adverse effects and levels of insulin, glucose and plasma Αβ amyloid after treatment).
Risk of bias in individual studies
Risk of bias in randomized control trials was assessed by 2 reviewers (DK and PM) independently using the Cochrane Collaboration’s tool for assessing risk of bias (ROB) [25]. The evaluation was performed for every outcome within each study. Disagreements between authors were solved through consensus. The domains assessed were bias due to random sequence generation and allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias) and selective reporting (reporting bias). A study was characterized of high risk for overall ROB if at least one ROB domain was of high risk. All ROB domains had to be of low risk for a study to be characterized as of low risk. In any other case, the study was deemed to be at unclear overall risk. Regarding the Rosenbloom et al. study, due to the cross-over design, risk of bias was based on the instructions of Cochrane Handbook for Systematic Reviews of Interventions for cross-over trials.
Results
Search results
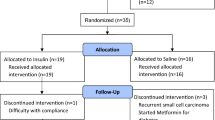
The search yielded 306 potentially eligible studies. After duplicates were removed, 186 articles were excluded based on their title and abstract. Eventually, 12 full-text articles were assessed for eligibility. Three articles were excluded because they were conference abstracts and contained incomplete information or potential duplicate results [26,27,28]. Another study was excluded as it was not an RCT [13]. Finally, one study was excluded because it did not provide enough statistical data [29]. The flowchart presenting the selection of studies is provided in Fig. 1.
Studies’ and patients’ characteristics
Seven articles were eventually deemed eligible, including a total of 293 patients [30,31,32,33,34,35,36]; 172 were diagnosed with MCI and 121 with AD. The patients were assigned either to IN insulin or placebo group. Four studies assessed the effect of IN regular insulin [31,32,33,34]. In two studies IN insulin glulisine and detemir were administrated, respectively [30, 35]. In another study, both IN regular and detemir were used [36]. Three studies examined the cognitive effects of IN insulin acutely after treatment [32, 33, 35]. In the rest of the studies, cognitive tasks were applied after a long period of treatment [30, 31, 34, 36]. The treatment doses varied from study to study. In addition, the patients’ apoe4 gene carriage status varied from study to study. The studies’ and patients’ characteristics are summarized in Tables 1 and 2, respectively.
Risk of bias
Regarding assessment of ROB, none of the randomized control trials (RCTs) was judged as of high risk. One study was deemed to be at low ROB [33]. Most studies were characterized of unclear ROB due to unclear risks in “allocation concealment” and/or “blinding of participants and personnel” and/or “blinding of outcome assessment” domains [30,31,32,33, 36]. Details about ROB assessment are presented in Figs. 2 and 3. Rosenbloom et al. cross-over study was judged as of low risk because the cross-over design was suitable for this trial (AD is a reasonably stable condition), the order of receiving treatments was randomized and there were no carry-over treatment effects.
Results of individual studies
Primary outcome (cognitive tasks)
Verbal memory and verbal working memory
Verbal memory was tested in all included studies with the assessment of the story recall task and the word list recall task [30,31,32,33,34,35,36]. Verbal working memory was tested only in one study, with the DOT counting N-back test [30].
Sometimes, response to treatment differed according to apoe4 status [32, 33]. One study showed that compared with placebo, various IN insulin doses (10, 20, 40 IU) improved immediate recall in apoe4 (−) and worsened it in apoe4 (+) patients, respectively [33]. Again, after administration of same insulin doses, delayed recall performance had a trend towards worsening among apoe4 (+), whereas it was unaffected among apoe4 (−) patients [33]. In another study, when compared with placebo, 20 and 40 IU of IN insulin significantly improved performance on the composite score of immediate and delayed story recall, in apoe4 (−) patients but no changes were observed for apoe4 (+) patients [32].
In two studies, story recall improved after administration of 20 and 40 IU of IN insulin, but patients were not stratified according to apoe4 status [31, 34]. In another study, in which 20 IU of IN insulin was given, performance on story recall was not affected but patients were solely apoe4 (+) [35].
Performance on immediate and delayed word list recall was either not affected or the results were conflicting [32, 33, 35]. One study assessed verbal memory as a composite score of immediate story recall, delayed story recall, immediate word list recall and delayed word list recall [30]. Score worsened for apoe4 (−) and improved for apoe4 (+) patients [30]. However, a long-acting form of insulin was used in this study (detemir) as opposed to regular insulin which is short-acting [30]. In another study, a composite score of delayed story recall and delayed word list recall was used [36]. This was the only study to implement two types of IN insulin (regular, detemir) for comparison with placebo [36]. Intranasal regular insulin was beneficial for apoe4 (−), while IN detemir improved performance in apoe4 (+) patients.
Verbal working memory was assessed only in one study [30]. Performance was improved after the 40 but not the 20 IU dose, regardless of apoe4 status [30]. The effects of IN insulin on verbal memory are presented in Table 3.
Attention, executive function and response inhibition
Attention, executive function and response inhibition were tested in five studies [30, 32,33,34,35]. In four of them, the assessment of attention and response inhibition was done with SCWT (Stroop Color Word Test) [30, 32,33,34]. In general, no significant effects were observed in SCWT after administration of different types and doses of intranasal insulin [30, 32,33,34,35]. Significant improvement was noticed only in one study, but the effect was restricted to discordant items [34]. There was no effect on concordant items or the number of errors [34].
Another study assessed attention/executive function with the use of “Trails B test”, “RBANS digit span forward” and “RBANS digit span backward” [35]. Significantly improved performance was observed only for the first task [35] (Table 4).
Visuospatial function
Visuospatial function was assessed in four studies [30, 32, 33, 35]. In general, no significant effects were observed [30, 32, 33, 35]. Exception to this was the significantly improved performance regardless of apoe4 status on BVTR (Benton Visual Retention Test) after the administration of 40 IU of IN insulin detemir, regardless of apoe4 status [30]. The effect was not observed for the 20 IU dose [30] (Table 5).
Functional status, daily activity and global cognition
Functional status and daily activity were assessed in four studies with the use of DSRS (Dementia Severity Rating Scale) or Alzheimer’s Disease Cooperative Study-activities of daily living (ADCS-ADL) scores, respectively [30, 31, 34, 36]. Regarding DSRS scores, the results were conflicting [30, 31, 34, 36]. ADCS-ADL scale scores were preserved for AD patients of the insulin-assigned group but declined for the AD patients of the placebo group; scores of MCI patients were all unaffected regardless of group assignment [31]. Craft et al. used a measure of global cognition named ADAS-Cog scale, in their two studies [31, 36]. Improvements were found only in one study [31] (Table 6).
Secondary outcomes
Effects on Αβ40 and Αβ42
Two studies reported the effects of IN insulin on plasma Αβ40 and Αβ42 amyloid levels [33, 34]. In addition, two studies reported the effects on the CSF Αβ40 and Αβ42 levels [31, 36]. The results were very conflicting [31, 33, 34, 36] (Table 7).
Metabolic data
Four studies reported the effects of IN insulin treatment on plasma glucose and insulin levels [32,33,34,35]. In three of them, no significant change in plasma glucose or insulin levels were observed after treatment [32, 33, 35]. In Rosenbloom et al.’s study, there was also no change in fasting glucose or insulin levels after 21 days of treatment [35]. However, reduced postprandial plasma insulin levels were observed for treatment group when compared to placebo [F (1, 20 = 4.43, p = 0.0481)] [35].
Adverse effects
Adverse effects included nose-related side effects (minor bleeding, soreness, rhinitis, sneezing), headache, dizziness, weakness and upper respiratory tract infections. A complete list of adverse effects is depicted in Table 8.
Discussion
In this systematic review of randomized clinical trials, we found evidence that IN insulin may have a beneficial effect on verbal memory, probably modified by apoe4 allele carrier status; the effect was favorable for apoe4 (−) patients but not for apoe4 (+) patients. For the rest cognitive domains (visuospatial function, attention, executive function, response inhibition and everyday functioning) there was not any clear effect by IN insulin administration. Of note, the expected absence of systemic side effects of IN insulin treatment was confirmed by our findings.
Response to treatment and apoe4 status
Of all cognitive domains tested, verbal memory (story and/or word list recall) was affected the most. Interestingly, the patients’ apoe4 allele carrier status appeared to determine the response to treatment, which is in accordance with previous studies [37]. In particular, apoe4 (−) patients were positively affected by treatment especially when they were tested on story recall component of verbal memory [32, 33, 36]. On the other hand, patients with apoe4 (+) status, had either unchanged or worse performance on verbal memory tasks after treatment [32, 33, 35]. Negative for apoe4 gene, AD patients are known to have increased insulin resistance and decreased glucose utilization, in comparison to apoe4 (+) patients [38]. Apolipoprotein4 (−) patients require higher insulin doses than for apoe4 (+) patients, for memory enhancement [37]. However, they have greater memory improvements in hyperinsulinemic states and this may partially explain the selective positive response of apoe4 (−) patients to IN insulin [39]. Our data showed that IN insulin doses of 10 or 20 IU were potent enough to facilitate verbal memory and especially story recall component [31,32,33,34]. Generally, absence of apoe4 gene in AD or MCI patients is associated with better responses to various AD treatments, especially in high doses [40,41,42]. In contrast to apoe4 (−) patients, it is hypothesized that insulin may worsen functional and metabolic brain abnormalities that apoe4 (+) patients are shown to have [43, 44]. In addition, there is evidence of mitochondrial dysfunction in posterior cingulate gyrus of apoe4 (+) carriers [45]. Such a finding could explain the unresponsiveness of apoe4 (+) patients to IN insulin. Studies have demonstrated a relative increase in apoe4 carriage among individuals with AD [46]. These facts may restrict IN therapy application and may at least require appropriate selection of candidates for treatment. However, in two included studies in which a long-acting IN insulin (detemir) was used, there was an improvement for apoe4 carriers in verbal memory, but not for apoe4 (−) [30, 36]. This evidence provides hope for the treatment of apoe4 (+) patients and it could mean that different types of IN insulin are required for different apoe4 groups.
Performance in cognitive domains such as visuospatial function, attention, executive function and response inhibition stayed unaffected [30,31,32,33,34,35]. One possible explanation is that since these functions have already declined up to some point in AD or MCI patients, the neuropsychological tests may not be sensitive enough to show further decline (or improvement).
Intranasal insulin had some beneficial effects on general functioning of MI patients, tested with DSRS [30, 31, 34, 36]. Regarding ADCS-ADL scale, a daily activity testing tool, there was a beneficial effect for AD patients only, who preserved their function relative to placebo. The same was not true for MCI patients [31, 33, 34]. This may be attributed to the fact that ADCS-ADL scale was originally designed for AD patients only, which are by definition considered to be at a more advanced stage cognitive decline than MCI patients [23]. Finally, performance on a general cognition measure called ADAS-cog varied among studies [31, 36, 47]. Such inconsistencies between studies can be attributed to the small number of subjects participating in those trials [31, 36].
Types and doses of IN insulin
Studies on healthy subjects have shown that IN regular insulin has beneficial effect on memory [48]. Such benefits were shown in our review mostly for story recall task in apoe4 (−) patients, actually for all possible doses (10, 20, 40, 60 IU) and for both short- and long-term treatments [31,32,33,34, 36]. It has been suggested that rapid-acting IN insulin is superior to regular insulin [49]. However, this was not confirmed by our included study which used glulisine (rapid-acting insulin) [35]. Of interest, this study included patients that were exclusively apoe4 (+) which is known to be “difficult” for treatment subgroup [45]. This may explain why findings were not in accordance with previous studies [35, 49].
Despite the unresponsiveness of apoe4 carriers to rapid- or short-acting types of IN insulin (regular, glulisine), there was a beneficial effect after administration of a long-acting IN insulin analogue (detemir) on verbal memory [30, 36]. It is known that insulin detemir binds plasma albumin [50]. In addition, apoe4 carriers with AD have a tendency for post-translational modifications of albumin which in turn may affect the binding of detemir [51, 52]. Thus, special pharmacokinetic properties of insulin determir may be responsible for its positive effects on apoe4 (+) patients. In addition, it has been shown that this type of insulin exerts strong CNS effects which supports further the possible use of it in the resistant to treatment apoe4 (+) patients [53]. Of interest, the benefits were observed for the 40 IU but not the 20 IU dose [30, 36]. This could mean that low doses of detemir may not be enough for improvement of cognitive functions in apoe4 (+) patients, but there is need for further studies to confirm these findings.
Safety issues
Studies on healthy subjects have shown that IN insulin is well tolerated even in high dose (60 IU daily) and for a long period of time (3 weeks) [54]. The observation that serious adverse effects are almost absent after IN insulin administration has already been underlined in previous studies [20, 55]. That was also confirmed by the findings of the present review. The only adverse effects had to do with nasal symptoms, which may be due to the route of administration rather than the drug itself [30,31,32, 34, 36]. Of great importance is that the risk of hypoglycemia was practically negligible, finding that is also in accordance with previous data [30,31,32, 34, 36, 54]. The minimal risk of hypoglycemia by IN insulin has also been demonstrated in studies where this type of treatment failed to lower glucose in diabetic patients [56,57,58,59]. Therefore, IN insulin is a safe treatment for patients with AD or MCI.
Limitations
Intranasal insulin is a novel treatment for patients with AD or MCI and has been only tested in few clinical trials. The present systematic review included a total of 293 patients. Such a small sample size does not allow for safe conclusions. Additionally, all included studies took place at one country (USA), thus there is limitation in generalizability of the results.
Another limitation of the present review is the heterogeneity of the included studies. First of all, there was heterogeneity in respect to patients’ characteristics such as gender, age and apoe4 status (see Table 1). In addition, different cognitive domains were assessed in each study, while cognitive tasks varied even among studies assessing the same cognitive domains (see Tables 3, 4, 5, 6). Moreover, types and doses of insulin varied between studies (see Table 1). Finally, the duration of treatment was heterogeneous, too (days of treatment varied from 1 to 120). Consequently, quantitative analysis (meta-analysis) of the included studies was not feasible.
Conclusions
The present systematic review examined the effects of IN insulin administration on cognitive function of patients with AD or MCI. Collective evidence shows improvement in verbal memory and especially story recall, while IN insulin effects on other aspects of cognition was neutral. The data suggest that the treatment effect is modified by the apoe4 gene carriage status of patients: Apoe4 (−) patients showed more consistent cognitive gains in comparison to apoe4 (+) patients, whose performance either remained stable or declined after IN insulin treatment. However, there is evidence hinting that even these patients may benefit from IN insulin if a long-acting form of insulin rather than a rapid or short-acting form is used. Current data are not definite on whether IN insulin can be used as treatment for dementia of AD or MCI but provide strong evidence for its safety as the systemic side effects and especially hypoglycemia were essentially negligible. Proper selection of patients, stratification by disease stage, apoe4 carrier status and different types of insulin and doses will be needed in future studies for clearer results.
References
Keuck L (2017) Slicing the cortex to study mental illness: alois Alzheimer’s pictures of equivalence. Prog Brain Res 233:25–51
Fiest KM, Roberts JI, Maxwell CJ, Hogan DB, Smith EE, Frolkis A et al (2016) The prevalence and incidence of dementia due to Alzheimer’s disease: a systematic review and meta-analysis. Can J Neurol Sci Le journal canadien des sciences neurologiques 43(Suppl 1):S51–S82
Olazaran J, Aguera-Ortiz L, Argimon JM, Reed C, Ciudad A, Andrade P et al (2017) Costs and quality of life in community-dwelling patients with Alzheimer’s disease in Spain: results from the GERAS II observational study. Int Psychogeriatr 29(12):2081–2093
Birks JS, Grimley EJ (2015) Rivastigmine for Alzheimer’s disease. Cochrane Database Syst Rev 10(4):Cd001191
Jiang J, Jiang H (2015) Efficacy and adverse effects of memantine treatment for Alzheimer’s disease from randomized controlled trials. Neurol Sci Off J Italian Neurol Soc Italian Soc Clin Neurophysiol 36(9):1633–1641
Liao X, Li G, Wang A, Liu T, Feng S, Guo Z et al (2015) Repetitive transcranial magnetic stimulation as an alternative therapy for cognitive impairment in Alzheimer’s disease: a meta-analysis. JAD 48(2):463–472
Yang M, Xu DD, Zhang Y, Liu X, Hoeven R, Cho WC (2014) A systematic review on natural medicines for the prevention and treatment of Alzheimer’s disease with meta-analyses of intervention effect of ginkgo. Am J Chin Med 42(3):505–521
Tsolaki MN, Koutsouraki ES, Katsipis GK, Myserlis P Gr., Chatzithoma MA, Pantazaki AA (2017) Alternative anti-infective/anti-inflammatory therapeutic options for fighting Alzheimer’s disease. In: Frontiers in anti-infective drug discovery, chap 1, vol 6. Bentham Science Publishers, pp 1–153
Cukierman T, Gerstein HC, Williamson JD (2005) Cognitive decline and dementia in diabetes–systematic overview of prospective observational studies. Diabetologia 48(12):2460–2469
Biessels GJ, Staekenborg S, Brunner E, Brayne C, Scheltens P (2006) Risk of dementia in diabetes mellitus: a systematic review. Lancet Neurol 5(1):64–74
Stanley M, Macauley SL, Holtzman DM (2016) Changes in insulin and insulin signaling in Alzheimer’s disease: cause or consequence? J Exp Med 213(8):1375–1385
Zhao WQ, Townsend M (2009) Insulin resistance and amyloidogenesis as common molecular foundation for type 2 diabetes and Alzheimer’s disease. Biochem Biophys Acta 1792(5):482–496
de la Monte SM, Wands JR (2008) Alzheimer’s disease is type 3 diabetes-evidence reviewed. J Diabetes Sci Technol 2(6):1101–1113
De Felice FG, Vieira MN, Bomfim TR, Decker H, Velasco PT, Lambert MP et al (2009) Protection of synapses against Alzheimer’s-linked toxins: insulin signaling prevents the pathogenic binding of Abeta oligomers. Proc Natl Acad Sci USA 106(6):1971–1976
Gasparini L, Gouras GK, Wang R, Gross RS, Beal MF, Greengard P et al (2001) Stimulation of beta-amyloid precursor protein trafficking by insulin reduces intraneuronal beta-amyloid and requires mitogen-activated protein kinase signaling. J Neurosci 21(8):2561–2570
Craft S, Asthana S, Newcomer JW, Wilkinson CW, Matos IT, Baker LD et al (1999) Enhancement of memory in Alzheimer disease with insulin and somatostatin, but not glucose. Arch Gen Psychiatry 56(12):1135–1140
Craft S, Newcomer J, Kanne S, Dagogo-Jack S, Cryer P, Sheline Y et al (1996) Memory improvement following induced hyperinsulinemia in Alzheimer’s disease. Neurobiol Aging 17(1):123–130
Hanson LR, Frey WH 2nd (2008) Intranasal delivery bypasses the blood-brain barrier to target therapeutic agents to the central nervous system and treat neurodegenerative disease. BMC Neurosci 9(Suppl 3):S5
Freiherr J, Hallschmid M, Frey WH 2nd, Brunner YF, Chapman CD, Holscher C et al (2013) Intranasal insulin as a treatment for Alzheimer’s disease: a review of basic research and clinical evidence. CNS Drugs 27(7):505–514
Lioutas VA, Alfaro-Martinez F, Bedoya F, Chung CC, Pimentel DA, Novak V (2015) Intranasal insulin and insulin-like growth factor 1 as neuroprotectants in acute ischemic stroke. Transl Stroke Res 6(4):264–275
Holscher C (2014) First clinical data of the neuroprotective effects of nasal insulin application in patients with Alzheimer’s disease. Alzheimer’s Dementi 10(1 Suppl):S33–S37
Reger MA, Craft S (2006) Intranasal insulin administration: a method for dissociating central and peripheral effects of insulin. Drugs Today (Barcelona, Spain: 1998) 42(11):729–739
Petersen RC, Doody R, Kurz A, Mohs RC, Morris JC, Rabins PV et al (2001) Current concepts in mild cognitive impairment. Arch Neurol 58(12):1985–1992
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clinical research ed). 339:b2535
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clinical research ed). 343:d5928
Claxton A, Wilkinson C, Baker L, Watson G, Bonner LM, Trittschuh E et al (2012) Intranasal insulin treatment response in Alzheimer’s disease influenced by glucose-stimulated insulin secretion. Alzheimer’s Dementia 8(4 suppl. 1):[P582 p.]. http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/247/CN-01031247/frame.html. Accessed 25 May 2017
Craft S, Claxton A, Hanson A, Cholerton B, Neth B, Trittschuh E et al (2014) Therapeutic effects of intranasal insulin and insulin analogues on cognition and MRI measures in mild cognitive impairment and Alzheimer’s disease. Alzheimer’s Dementia 10:[P126 p.]. http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/790/CN-01056790/frame.html. Accessed 25 May 2017
Rosenbloom M, Barclay T, Pyle M, Owens B, Anderson C, Frey W et al (2013) The effect of intranasal rapid acting insulin on ApoE-epsilon4 carriers with mild-to-moderate Alzheimer’s disease. Alzheimer’s Dementia 9(4 suppl. 1):[P888 p.]. http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/845/CN-01060845/frame.html. Accessed 25 May 2017
Main (2007) Intranasal insulin and memory in early Alzheimer’s disease. ClinicalTrialsgov. http://clinicaltrials.gov. http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/747/CN-00724747/frame.html. Accessed 25 May 2017
Claxton A, Baker LD, Hanson A, Trittschuh EH, Cholerton B, Morgan A et al (2015) Long-acting intranasal insulin detemir improves cognition for adults with mild cognitive impairment or early-stage Alzheimer’s disease dementia. JAD 44(3):897–906
Craft S, Baker LD, Montine TJ, Minoshima S, Watson GS, Claxton A et al (2012) Intranasal insulin therapy for Alzheimer disease and amnestic mild cognitive impairment: a pilot clinical trial. Arch Neurol 69(1):29–38
Reger MA, Watson GS, Frey WH 2nd, Baker LD, Cholerton B, Keeling ML et al (2006) Effects of intranasal insulin on cognition in memory-impaired older adults: modulation by APOE genotype. Neurobiol Aging 27(3):451–458
Reger MA, Watson GS, Green PS, Baker LD, Cholerton B, Fishel MA et al (2008) Intranasal insulin administration dose-dependently modulates verbal memory and plasma amyloid-beta in memory-impaired older adults. JAD 13(3):323–331
Reger MA, Watson GS, Green PS, Wilkinson CW, Baker LD, Cholerton B et al (2008) Intranasal insulin improves cognition and modulates beta-amyloid in early AD. Neurology 70(6):440–448
Rosenbloom MH, Barclay TR, Pyle M, Owens BL, Cagan AB, Anderson CP et al (2014) A single-dose pilot trial of intranasal rapid-acting insulin in apolipoprotein E4 carriers with mild-moderate Alzheimer’s disease. CNS Drugs 28(12):1185–1189
Craft S, Claxton A, Baker LD, Hanson AJ, Cholerton B, Trittschuh EH et al (2017) Effects of regular and long-acting insulin on cognition and Alzheimer’s disease biomarkers: a pilot clinical trial. JAD 57(4):1325–1334
Craft S, Asthana S, Cook DG, Baker LD, Cherrier M, Purganan K et al (2003) Insulin dose-response effects on memory and plasma amyloid precursor protein in Alzheimer’s disease: interactions with apolipoprotein E genotype. Psychoneuroendocrinology 28(6):809–822
Craft S, Asthana S, Schellenberg G, Baker L, Cherrier M, Boyt AA et al (2000) Insulin effects on glucose metabolism, memory, and plasma amyloid precursor protein in Alzheimer’s disease differ according to apolipoprotein-E genotype. Ann N Y Acad Sci 903:222–228
Craft S, Asthana S, Schellenberg G, Cherrier M, Baker LD, Newcomer J et al (1999) Insulin metabolism in Alzheimer’s disease differs according to apolipoprotein E genotype and gender. Neuroendocrinology 70(2):146–152
Risner ME, Saunders AM, Altman JF, Ormandy GC, Craft S, Foley IM et al (2006) Efficacy of rosiglitazone in a genetically defined population with mild-to-moderate Alzheimer’s disease. Pharmacogenomics J 6(4):246–254
Podewils LJ, Guallar E, Kuller LH, Fried LP, Lopez OL, Carlson M et al (2005) Physical activity, APOE genotype, and dementia risk: findings from the Cardiovascular Health Cognition Study. Am J Epidemiol 161(7):639–651
Reger MA, Henderson ST, Hale C, Cholerton B, Baker LD, Watson GS et al (2004) Effects of beta-hydroxybutyrate on cognition in memory-impaired adults. Neurobiol Aging 25(3):311–314
Reiman EM, Caselli RJ, Chen K, Alexander GE, Bandy D, Frost J (2001) Declining brain activity in cognitively normal apolipoprotein E epsilon 4 heterozygotes: a foundation for using positron emission tomography to efficiently test treatments to prevent Alzheimer’s disease. Proc Natl Acad Sci USA 98(6):3334–3339
Reiman EM, Chen K, Alexander GE, Caselli RJ, Bandy D, Osborne D et al (2004) Functional brain abnormalities in young adults at genetic risk for late-onset Alzheimer’s dementia. Proc Natl Acad Sci USA 101(1):284–289
Valla J, Yaari R, Wolf AB, Kusne Y, Beach TG, Roher AE et al (2010) Reduced posterior cingulate mitochondrial activity in expired young adult carriers of the APOE epsilon4 allele, the major late-onset Alzheimer’s susceptibility gene. JAD 22(1):307–313
Farrer LA, Cupples LA, Haines JL, Hyman B, Kukull WA, Mayeux R et al (1997) Effects of age, sex, and ethnicity on the association between apolipoprotein E genotype and Alzheimer disease. A meta-analysis. APOE and Alzheimer Disease Meta Analysis Consortium. JAMA 278(16):1349–1356
Rosen WG, Mohs RC, Davis KL (1984) A new rating scale for Alzheimer’s disease. Am J Psychiatry 141(11):1356–1364
Benedict C, Hallschmid M, Hatke A, Schultes B, Fehm HL, Born J et al (2004) Intranasal insulin improves memory in humans. Psychoneuroendocrinology 29(10):1326–1334
Benedict C, Hallschmid M, Schmitz K, Schultes B, Ratter F, Fehm HL et al (2007) Intranasal insulin improves memory in humans: superiority of insulin aspart. Neuropsychopharmacology: official publication of the American College of Neuropsychopharmacology 32(1):[239–43 pp.]. http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/869/CN-00571869/frame.html. Accessed 15 Nov 2017
Pandyarajan V, Weiss MA (2012) Design of non-standard insulin analogs for the treatment of diabetes mellitus. Curr DiabRep 12(6):697–704
Wada T, Azegami M, Sugiyama M, Tsuneki H, Sasaoka T (2008) Characteristics of signalling properties mediated by long-acting insulin analogue glargine and detemir in target cells of insulin. Diabetes Res Clin Pract 81(3):269–277
Colton CA, Needham LK, Brown C, Cook D, Rasheed K, Burke JR et al (2004) APOE genotype-specific differences in human and mouse macrophage nitric oxide production. J Neuroimmunol 147(1–2):62–67
Hallschmid M, Jauch-Chara K, Korn O, Molle M, Rasch B, Born J et al (2010) Euglycemic infusion of insulin detemir compared with human insulin appears to increase direct current brain potential response and reduces food intake while inducing similar systemic effects. Diabetes 59(4):1101–1107
Kupila A, Sipila J, Keskinen P, Simell T, Knip M, Pulkki K et al (2003) Intranasally administered insulin intended for prevention of type 1 diabetes—a safety study in healthy adults. Diabetes/Metabol Res Rev 19(5):415–420
Novak V, Milberg W, Hao Y, Munshi M, Novak P, Galica A et al (2014) Enhancement of vasoreactivity and cognition by intranasal insulin in type 2 diabetes. Diabetes Care 37(3):751–759
Frauman AG, Jerums G, Louis WJ (1987) Effects of intranasal insulin in non-obese type II diabetics. Diabetes Res Clin Pract 3(4):197–202
Lalej-Bennis D, Boillot J, Bardin C, Zirinis P, Coste A, Escudier E et al (2001) Six month administration of gelified intranasal insulin in 16 type 1 diabetic patients under multiple injections: efficacy vs subcutaneous injections and local tolerance. Diabetes Metabol 27(3):372–377
Frauman AG, Cooper ME, Parsons BJ, Jerums G, Louis WJ (1987) Long-term use of intranasal insulin in insulin-dependent diabetic patients. Diabetes Care 10(5):573–578
Lalej-Bennis D, Boillot J, Bardin C, Zirinis P, Coste A, Escudier E et al (2001) Efficacy and tolerance of intranasal insulin administered during 4 months in severely hyperglycaemic Type 2 diabetic patients with oral drug failure: a cross-over study. Diabetic Med 18(8):614–618
Author information
Authors and Affiliations
Contributions
KLA: Study concept, design and writing of the manuscript (including tables). GK: Data collection process (literature search, flow diagram and data extraction from the included studies). AM: Data collection process (literature search, flow diagram and data extraction from the included studies). DK: Assessment of risk of bias of the included studies (including the respective figures of “Risk of bias”). PM: Contribution to methodology and design of the study, helped with the disagreements of literature search and data extraction which were originally conducted by Dr. Kalaitzidis and Dr. Malli, reviewed the initial draft. VSL: Critical revision of the manuscript for important intellectual content, approval of the paper.
Corresponding author
Ethics declarations
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Funding
This study was not sponsored by any company. Dr. Avgerinos reports no disclosures. Dr. Kalaitzidis reports no disclosures. Dr. Malli reports no disclosures. Dr. Kalaitzoglou reports no disclosures. Dr. Myserlis reports no disclosures. Dr. Lioutas reports no disclosures.
Rights and permissions
About this article
Cite this article
Avgerinos, K.I., Kalaitzidis, G., Malli, A. et al. Intranasal insulin in Alzheimer’s dementia or mild cognitive impairment: a systematic review. J Neurol 265, 1497–1510 (2018). https://doi.org/10.1007/s00415-018-8768-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-018-8768-0