Abstract
Multiple sclerosis (MS) is an autoimmune disease of the central nervous system (CNS) with a diverse disease course involving inflammation and degeneration of neurons and axons. Multiple sclerosis results from a complex interaction of genetic and environmental factors and clinically several disease subtypes with marked variation in symptoms can be discerned. Disease-modifying therapies (DMTs) impact disease activity and outcome. Long-term follow-up studies of DMTs in MS have generally shown that the short-term effects in clinical trials are maintained for up to 21 years, e.g. in the case of interferon beta-1b. However, attainment can be a problem in these studies. On the one hand, so-called real-world studies can augment clinical trials by providing data on the long-term effectiveness and safety of DMTs but lack, on the other hand, randomization and may, in addition, also yield biased findings as a result of compliance issues. Long-term data from clinical trials in clinically isolated syndrome (CIS) patients have been limited but in the case of interferon beta-1b this aspect has been addressed over 11 years in the BENEFIT 11 trial. The results suggest that early treatment results in persistent long-term benefits including conversion to clinically definite MS (CDMS) as well as time to and risk of a first relapse. Here we primarily review the findings of the BENEFIT 11 trial in the context of long-term studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Natural history of multiple sclerosis
Multiple sclerosis (MS) is an autoimmune disease of the central nervous system (CNS) involving inflammation and degeneration of neurons and axons. Aspects of the disease are diverse with respect to clinical presentation, disease course, paraclinical read-outs such as magnetic resonance imaging (MRI) and histopathological features [1, 2]. Considerable research has suggested that MS is associated with both genetic and environmental factors [3, 4] but it is still unclear if there is a single or multiple causes for MS. A number of contributing factors increasing the susceptibility to MS have been proposed including vitamin D, viral infections (most commonly Epstein–Bar virus [EBV]), obesity in adolescence, latitude, female sex and smoking [1, 4,5,6].
Clinically, there are two different disease subtypes of MS—relapsing MS (RMS), and progressive MS (PMS) either manifesting itself as primary-progressive MS (PPMS) or secondary-progressive MS (SPMS) [7]. Furthermore, there are two defined MS pre-stage syndromes—radiologically and clinically isolated syndrome (RIS and CIS, respectively). RIS is controversial in that incidental MRI findings suggesting inflammatory demyelination are seen in the absence of clinical symptoms. CIS, on the other hand, is commonly accepted as the first clinical manifestation of inflammatory CNS demyelination that may eventually convert to MS but does not yet formally fulfill the criteria for dissemination in time and space [8,9,10]. The definition of CIS has considerably changed over the years. While in the 2001 and 2005 McDonald criteria CIS was defined as the objective clinical evidence of one monosymptomatic lesion [11, 12], the 2010 criteria stress that CIS presentations can be monofocal or multifocal, and typically involve the optic nerve, brainstem/cerebellum, spinal cord, or cerebral hemispheres [13]. The recent 2017 criteria state that a CIS is a monophasic clinical episode with patient-reported symptoms and objective findings reflecting a focal or multifocal inflammatory demyelinating event in the CNS, developing acutely or subacutely. It must last at least 24 h, with or without recovery, and in the absence of fever or infection, similar to a typical multiple sclerosis relapse, but in a patient not known to have multiple sclerosis [10]. This development shows that with increased understanding of this entity the definition became increasingly precise. In PMS, which is characterized by a gradual worsening of symptoms with or without relapses, neurodegeneration outweighs inflammation. SPMS is diagnosed in patients who show a gradual worsening following a relapsing course.
MRI plays an important role in the diagnosis of MS. Characteristic CNS lesions (as defined by the MAGNIMS [Magnetic Resonance Imaging in MS] and McDonald 2017 criteria identified on MRI in combination with clinical symptoms are usually used for diagnosis [9, 10]).
Survival and causes of death have been investigated using patient records at Hordeland University Hospital, West Norway in a 60-year population-based MS cohort (n = 1388) compared with the general population [14]. Median life expectancy was 74.7 and 81.8 years for MS patients and the general population, respectively (p < 0.001), demonstrating that MS, per se, results in a shortened life expectancy. Similar results were obtained in a large scale analysis of databases from insurance companies in the US comparing MS patients and comparator subjects. Based on data from 30,402 MS patients and 89,818 non-MS controls annual mortality rates were calculated and shown to be 899/100,000 among MS patients and 446/100,000 among comparators. Kaplan–Meier analysis demonstrated a median survival from birth that was 6 years lower in MS patients versus comparators [15].
The evolving concepts in the treatment of RMS have already been concisely reviewed: Results from randomised controlled trials in populations with CIS as well as observational clinical studies, support the efficacy of early use of disease-modifying therapies in delaying the conversion to clinically definite multiple sclerosis (CDMS) and post-marketing studies have also confirmed the importance of early treatment [16,17,18,19,20,21,22]. This review focuses on the lessons learned from the extension phases of randomized-controlled interferon beta trials.
Long-term studies in multiple sclerosis
Several long-term MS studies have been reported, which generally follow-up shorter, randomized, controlled trials (Table 1).
Interferon beta-1b (IFNβ-1b)
The 16-year long-term follow-up of the pivotal IFNβ-1b trial reassessed patients and evaluated which clinical and MRI measures of the original trial predicted change in both physical and cognitive outcomes [23]. The results indicated that the baseline Expanded Disability Status Score (EDSS) significantly correlated with the development of physical disability and cognitive decline in the further course of the disease (both p < 0.0001). Furthermore, the accrual of disability and annualized relapse rate (ARR) in the randomized, controlled initial trial also correlated with physical outcome but not cognition 16 years later (both p < 0.0001). Interestingly, baseline T2 lesion load and baseline brain atrophy on MRI only correlated with cognition (p < 0.0001) but not physical outcome. In a follow-up analysis the predictive validity of different NEDA (No evidence of disease activity) composite measures at 2 years for negative disability outcomes (defined as death, requirement for a wheelchair, EDSS 6, or progressive MS), at 16 years and survival at 21 years after randomization were examined [24]. Only absence of relapses or disability progression captured by EDSS (i.e. clinical NEDA) during the first 2 years predicted long-term clinical outcome. NEDA-3 encompassing MR metrics of disease activity and burden failed to increase predictive validity.
The authors concluded, therefore, that since baseline measures showed stronger prediction than on-trial changes, long-term outcome can be mainly determined early in the course of MS. This is a crucial result as more accurate prognosis of the future disease course at disease onset will be facilitated.
A total of 366 patients (98.4% of the originally-recruited patients) from the pivotal IFNβ-1b trial could be assessed further for all-cause mortality after 21 years [25]. At follow-up (median 21.1 years), a total of 81 deaths had occurred (22.1%) with a significant reduction in all-cause mortality in patients treated with 250 µg IFNβ-1b versus placebo (p = 0.0173). In addition, the hazard rate of death was lowered by 46.8% or 46.0% (IFNβ-1b treatment 250 µg or 50 µg, respectively). Of note, the authors themselves concede that it is unclear why IFNβ-1b 50 µg had a similar effect on survival as IFNβ-1b 250 µg compared with placebo. They assume that this benefit may be attributable to effects of IFNβ-1b, which are independent of the dose differences. While the precise mechanisms of IFNβ-1b are still unclear, antioxidative effects might play a role in this context. Taken together, these findings indicate a significant survival advantage for patients treated earlier with IFNβ-1b compared with placebo. Of note and as pointed out above, several reports have indicated that patients with MS have a shorter life expectancy [14, 15].
Interferon beta-1a (IFNβ-1a)
Patients with RRMS from the randomized, placebo-controlled, double-blind, 2-year trial of intramuscular (i.m.) IFNβ-1a entered an open-label, non-standardized treatment regime following the 2-year period [26]. In those patients who remained on IFNβ-1a (46%) there was a significantly lower mean EDSS score (p = 0.011), less progression with better general health and greater independence after 15 years. In addition, patients continuing IFNβ-1a had a better quality of life (QOL) and less disability than patients who were not using this DMT at 15 years.
The original Prevention of Relapses and Disability by Interferon beta-1a Subcutaneously in Multiple Sclerosis (PRISMS) trial of subcutaneous (s.c.) IFNβ-1a demonstrated significant clinical and MRI benefits after 2 years with both doses (22 and 44 µg, respectively). Patients who initially received placebo were randomized to blinded 22 or 44 µg IFNβ-1a (crossover group), while the remainder continued blinded treatment with the originally assigned dose. After 4 years, patients treated with IFNβ-1a in the crossover group had reduced relapse count, MRI activity and accumulation of lesion load compared with the placebo period (p < 0.001), demonstrating that even a later initiation of therapy still results in clinical and paraclinical benefits [27]. Patients on continuous treatment had better overall outcomes than those in the crossover group. Subsequently, long-term follow-up (7 or 8 years) in 68.2% of the initial population showed a continued benefit for patients initially randomized to the 44 µg dose versus the other treatment groups [28].
Glatiramer acetate (GA)
Patients with RRMS have received continuous treatment with glatiramer acetate (GA) as sole DMT in the ongoing US Glatiramer Acetate Trial [29]. In this open-label study, which started in 1991, patients were prospectively and regularly evaluated and were treated on average for 13.6 years. The ARR declined from baseline (1.12 ± 0.82 versus 0.25 ± 0.34 per year), EDSS scores were stable or improved (change ≤ 0.5 points) and 65% had not progressed to SPMS in the ongoing patient cohort, without any long-term safety issues.
Combination of glatiramer acetate and interferon
In a blinded extension for up to 7 years of the randomized, controlled study of combined use of IFNβ-1a and GA in patients with RRMS, the combination showed no clinical benefit compared with each alone [30]. An initial superior reduction of MRI disease activity with the combination did not result in a later clinical advantage. However, a sustained advantage was observed in the reduction of disease activity-free status.
Clinical trials in CIS patients
Often CIS is the first manifestation of MS and most of these patients will subsequently be diagnosed with MS [3, 31]. In clinical studies, CIS patients treated early with disease-modifying therapies (DMTs) show delayed conversion to CDMS [17, 20, 32,33,34,35]. However, relatively limited data are available on the long-term effects of early treatment of CIS in particular with respect to disability progression and QOL. In this context, the results from the Betaferon/Betaseron in Newly Emerging Multiple Sclerosis for Initial Treatment (BENEFIT) trial are of special interest as the patients were first randomly assigned to verum or placebo and after conversion to clinically definite multiple sclerosis (CDMS) or 2 years, patients on placebo could switch to IFNβ-1b or another treatment [33].
The BENEFIT trial investigated the effect of IFNβ-1b treatment after diagnosis of CIS [33]. Patients were initially randomized to receive IFNβ-1b 250 µg (early treatment) or placebo (delayed treatment) for 2 years. Placebo patients were offered IFNβ-1b treatment after 2 years or earlier if and when they converted to clinically definite MS CDMS. All were then eligible to enter a prospectively-planned and double-blinded follow-up phase for up to 5 years post-randomization. Patients in the early treatment group had a 37% reduced risk of CDMS (p = 0.007) compared with delayed treatment at 5 years, underlining the importance of early treatment. Patients were then entered into an open-label observational extension study for a maximum of 8.7 years.
Finally, the effects of IFNβ-1b treatment were evaluated in a prospective, comprehensive, 11-year (from randomization), cross-sectional assessment (BENEFIT 11) [36]. The patients included had to have been randomized and treated in the controlled phase at least once. The assessments included neurological history, EDSS and several tests for cognition, QOL, employment status and resource use. To include the more disabled patients who could not attend one of the centers, structured phone interviews were offered. A validated instrument for the telephone assessment of EDSS was included as part of these interviews. The primary objectives (disease course, relapse activity, change in disability, cognitive function, resource use and working status) and secondary objectives (MRI assessment, treatment history, QOL, fatigue, depression) were assessed with proportional hazards regression. Of note, patients in the “delayed” treatment group started on average only 1.5 years later than those with “early” treatment start, thus qualifying both groups as patients with a relatively early treatment start within a maximum of 2 years after CIS. In addition, the patient cohort in this study had active disease and high baseline T2 lesion load.
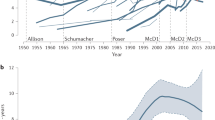
Of the 97 original BENEFIT sites, 66 participated in BENEFIT 11, enrolling overall 59.7% patients from the original BENEFIT study. In total, 71.3% of those randomized at these sites were evaluated in BENEFIT 11. Patients from both the early- and delayed-treatment arms had similar baseline characteristics and were comparable to the whole BENEFIT cohort. The results showed that the early treatment group demonstrated considerable improvement compared with those who had delayed treatment (Table 2). A reduction of 33% in the risk of converting to CDMS was seen in the early-treatment group compared with those treated later (p = 0.0012) and the time to CDMS was shorter in the delayed-treatment group (log rank p = 0.0034) (Fig. 1). Furthermore, the time to first relapse was reduced in the delayed-treatment group (p = 0.0005) while risk of a first relapse was reduced by 34.5% in those treated early compared with later. As the overall ARR was lower in the early-treatment group, a 19.1% reduction in the risk of relapses was seen (p = 0.0018). The risk of conversion to SPMS was slightly lower in the early group versus the delayed group (4.5% vs. 8.3%, respectively, Kaplan Meier (KM) estimate p = 0.4857). The Paced Auditory Serial Addition Task (PASAT)-3 total score, adjusted for baseline score, was higher in early treated patients (p = 0.0070) (Fig. 2). Overall, conversion to SPMS, change in EDSS, neuropsychological measures including fatigue and depressive symptoms [Symbol Digit Modalities Test (SDMT), Fatigue Scale for Motor and Cognitive Functions (FSMC), Center for Epidemiologic Studies Depression Scale (CES-D)], health-related QOL outcomes [EuroQoL-5 Dimension (EQ-5D), Functional Assessment of Multiple Sclerosis (FAMS)], and MRI outcomes were similar in both patient groups. In addition, employment and resource utilization were also comparable in both groups starting treatment relatively early.
Kaplan–Meier estimates of probability of clinically definite multiple sclerosis (a), annual relapse rate (b), EDSS scores (c) in BENEFIT 11 [36]. ARR annualized relapse rate, BENEFIT betaferon/betaseron in newly emerging multiple sclerosis for initial treatment, CDMS clinically confirmed multiple sclerosis, CI confidence interval, EDSS expanded disability status score, RR risk ratio. Reproduced by permission from Kappos et al. [36]. http://www.neurology.org
Paced Auditory Serial Addition Task total score (PASAT-3) from Baseline to Year 11 in BENEFIT 11 [36]. BENEFIT betaferon/betaseron in newly emerging multiple sclerosis for initial treatment, PASAT-3 paced auditory serial addition task total score. Reproduced by permission from Kappos et al. [36]. http://www.neurology.org
Interestingly, all outcome measures were positive when put into context with cohorts in other trials, despite the participants in BENEFIT 11 having highly active disease (exemplified by the median T2 lesion number in the early and delayed treatment groups). During the 11 years of this trial, adverse events were consistent with the known profile of IFNβ-1b and no new safety signals were reported. The overall findings from this study suggest that early treatment with IFNβ-1b has a long-term beneficial impact on the clinical course of MS.
With regard to fatigue and depression, the prevalence rates were lower in BENEFIT 11 over 11 years than rates from several natural history findings such as the North American Research Committee on Multiple Sclerosis (NARCOMS) database (moderate/severe fatigue prevalence 52% and depression 13% in patients with a self-reported diagnosis of MS) [37] and from other studies where prevalence rates for fatigue range from 50 to 97% and depression up to 59.6% [38,39,40]. In addition, the median number of correct responses in the SDMT in BENEFIT 11 (53 in 90 s) was similar to healthy controls and better than in patients with RRMS in various cohorts [41, 42]. For example, Benedict reported a mean score of 47.66 in RRMS and SPMS patients versus 62.16 in controls for SDMT. In total, 73.4% of all patients in BENEFIT 11 were still employed in the 11-year follow-up, which compares favorably with a survey conducted by the Multiple Sclerosis International Federation (MSIF). This online survey in 10 languages, which was completed by 8681 people from 125 countries, showed that 83% of people were not employed due to MS, with 47% stopping work within 3 years of MS diagnosis [43].
This 11-year long-term follow-up of the randomized BENEFIT trial in CIS patients fulfilled criteria of an interventional phase IV trial with rigid regulatory conduct due to the interventional diagnostic procedures undertaken. It was an open-label follow-up of the initial randomized study that had been double-blind during the 2 years of the placebo-controlled phase and then rater-blinded up to Year 5 of the prospectively planned BENEFIT / BENEFIT follow-up study.
In this trial, selection bias was minimized by facilitating non-mobile patients to participate using telephone assessments. Furthermore, there were no differences in baseline and Year 5 characteristics between patients enrolled in BENEFIT 11 who were treated early or late, with the only difference being an imbalance in T2 lesion numbers in the BENEFIT 11 cohort with a disadvantage for the early treatment group.
The patients enrolled in the BENEFIT 11 study represented an ideal patient group to examine long-term benefits of early treatment because of the frequent and comprehensive assessments from the start of the first clinical event. There was relatively stable disease after 11 years in both treatment arms possibly because all patients were treated relatively early in the disease course. Of note, the persistence of the beneficial effects of early treatment were seen despite only a short delay compared with the delayed group. In particular, ARR was lower in all but 2 of the follow-up years. Additionally, in the BENEFIT 11 trial, the two treatment groups did not differ in EDSS or change in EDSS. Furthermore, no difference was observed in patient-reported outcomes. There were no significant group differences on MRI outcomes of atrophy or lesion load. Nevertheless, there is a high proportion of patients having EDSS score < 3.0 whereas a natural history study from Canada found that after 10.2 years, 50% of the patients had reached EDSS score ≥ 3.0 [44].
The more favorable outcomes in the BENEFIT 11 study compared with reports from natural course studies, is possibly due to the overestimations from differences in ascertainment. The lower ascertainment in other studies may have resulted in the selection of patients with less severe disease than patients in BENEFIT 11. The trial participants in BENEFIT 11 had highly-active disease shown by the median T2 lesion number in both the early and delayed treatment groups.
The effect of baseline demographics as well as other factors was studied in the Barcelona CIS inception cohort [45]. In total, 1045 consecutive CIS patients had brain MRI scans within 5 months of the first attack and then at 1, 5, 10 and 15 years. Patients with an abnormal MRI scan were more likely to convert to CDMS than those with normal MRI scans (57% vs. 7%). These findings demonstrated that baseline MRI characteristics impact in the long-term.
In the Controlled High Risk Avonex® Multiple Sclerosis Prevention Study in Ongoing Neurological Surveillance (CHAMPIONS) trial that enrolled patients with CIS, factors associated with QOL were assessed 10 years after the diagnosis of CIS [46]. Not surprisingly, both a second clinical event indicating clinically definite MS (CDMS) and higher EDSS at 5 and 10 years was associated with lower scores on the 36-item Short Form Health Status Score Survey (SF-36) Physical Component Summary at year 10 (p < 0.01). Moreover, earlier onset of CDMS in patients resulted in worse patient-reported Physical Component Summary, AF-36 Mental Component Summary, fatigue and pain scores compared with those with no or later onset of CDMS after 10 years (p = 0.015).
General considerations
Following proof of clinical efficacy of a drug in a controlled trial, it is important to ascertain the long-term effects of therapeutic interventions. These can be assessed by trial extension or observational studies relying on large data bases. Extensions of clinical trials carry an advantage over observational studies since they are free from selection bias [47].
Ascertainment and selection bias
As mentioned further above, a major problem in long-term studies is ascertainment. In the IFNβ-1b 21-year study, ascertainment was extremely high at 98.4% whereas in other long-term studies it was significantly lower [25]. For instance, in the s.c. IFNβ-1a 8-year study ascertainment was 68.2% [48], while it was 40.5% in the IFNβ-1a 15-year trial [26], and 43% in the glatiramer acetate 15-year open label study [29]. Therefore, long-term trial results with low ascertainment may be associated with a selection bias.
Long-term evolution of disability in treated multiple sclerosis patients
In the prospective EPIC study (expression/genomics, proteomics, imaging and clinical) of actively-treated MS patients (recent onset of CDMS or CIS) to assess the long-term disease course and the predictive value of clinical and radiologic features at baseline and changes over 2 years, 41% showed stable or improved neurological disability (EDSS) up to 10 years compared with baseline [49]. Interestingly, patients assessed with no evidence of disease activity in the first 2 years had the same long-term outcomes as the whole cohort. Similarly, 25-OH vitamin D levels in serum had no effect on long-term disability. Overall, 10.7% (95% CI = 7.2–14%) of subjects reached EDSS ≥ 6 while 18.1% (95% CI 13.5–22.5%) developed SPMS from RMS at a median time of 16.8 years.
Overall conclusions and limitations
MS is an autoimmune disease with a diverse course, and both genetic and environmental factors are associated with susceptibility. Several different disease subtypes have been described and patients experience a wide range of symptoms. A number of long-term studies have been reported, especially with the DMTs that were licensed first and these generally show an advantage for early treatment. However, ascertainment is often low, which could bias the findings. Often patients who are doing poorly drop out and if this occurs more frequently in one arm of a study it can produce biased and therefore unreliable results [47].
Real-world studies, on the other hand, provide a valuable source of data on the long-term effectiveness and safety of DMTs and these data are usually routinely collected in clinical practice. The use of AUC analysis of EDSS has been suggested to leverage increased power from data on disability [50]. However, there is still a need for more extensive information on the real-world impact of these drugs, especially those licensed more recently.
To date, there is a lack of information on the long-term effects of early treatment in CIS, particularly for disability progression and QOL. The BENEFIT 11 follow-up of the pivotal BENEFIT trial has addressed these aspects with respect to IFNβ-1b. The results of the BENEFIT 11 study suggest that early treatment gives persistent long-term benefits that are possibly due to an early effect on immune regulation or a better preserved compensation capacity reducing the consequences of inflammatory attacks. The BENEFIT 11 study has the longest follow-up of the published studies of early treatment in CIS patients and includes outcome measures not used before. Furthermore, the patients recruited in this study were at the earliest stage of the disease.
The long-term follow-up studies with IFNs and GA have confirmed the efficacy and safety observed in the shorter, core clinical trials. However, the findings are more valuable when high ascertainment is achieved and selection biases are minimized as far as possible. Real-world data provide additional information to long-term follow-up studies in terms of evaluating different patient populations. Perhaps the most important outcome of long-term real-world studies investigating IFNs and GA in RMS is that these medications, while newer and more potent drugs have become available, continue to be effective MS treatments reliably reducing relapse rate, disability progression and conversion to CDMS while being well tolerated and remarkably safe. Therefore, they remain valuable therapeutic options in our armamentarium.
Of course, owing to the long duration of the trials discussed here, there are some relevant limitations that merit closer consideration. Dropout of patients is certainly a problematic point underlined by the fact that after 11 years only 71% of the originally randomized BENEFIT patients could be analyzed. Another issue is that in the 21 year follow-up of the original trial, it is not possible to distinguish between the possibility that the detected survival benefit resulted from an effect of early treatment or rather on a longer IFNβ-1b exposure as original placebo patients had less cumulative exposure to the drug. Maybe most importantly, however, correlations between short-term measures and long-term outcomes do not prove that these measures are true surrogates for long-term efficacy of any given drug. Of note, the authors of the 16 year cohort follow-up study themselves concede that. While the short-term measures they explored (relapses, disability and lesion load) are generally believed to reflect the pathological processes underlying permanent disability in MS (inflammation, demyelination and axonal injury) they were only modestly associated with disability or cognitive outcomes after 16 years. Their recent follow-up study provided evidence that absence of clinical activity at 2 years (“clinical NEDA”) had predictive validity long-term whereas incorporation of MR metrics, as in NEDA-3 did not increase this. Clearly, there is the necessity for an ongoing search for better and more reliable surrogate markers such as, for instance, NfL levels in the blood and CSF reflecting ongoing axonal damage.
Search criteria
Online literature search for this article was performed with PubMed (https://www.ncbi.nlm.nih.gov/pubmed) and Google scholar.(https://scholar.google.co.uk/) using parameters such as the respective drug or compound name in conjunction with the key words ‘interferons’, ‘CIS’, ‘conversion’, ‘survival’ and ‘long-term benefits’. There a large number of studies that could have been included but it was decided to focus on the BENEFIT study.
References
Efendi H, Karabudak R, Kantarci O et al (2015) Understanding multiple sclerosis better in 2014—environmental factors, remyelination, diagnostic techniques, treatment decisions and the future focus of multiple sclerosis treatment. Eur Neurol Rev 10(2):148–156
Dendrou CA, Fugger L, Friese MA (2015) Immunopathology of multiple sclerosis. Nat Rev Immunol 15:545–558
Compston A, Coles A (2008) Multiple sclerosis. Lancet 372:1502–1517
Reich DS, Lucchinetti CF, Calabrasi PA (2018) Multiple sclerosis. N Engl J Med 378:169–180
Olsson T, Barcellos LF, Alfredsson L (2017) Interactions between genetic, lifestyle and environmental risk factors for multiple sclerosis. Nat Rev Neurol 13:25–36
Geginat J, Paroni M, Pagani M et al (2017) The enigmatic role of viruses in multiple sclerosis: Molecular mimicry or disturbed immune surveillance? Trends Immunol 38:498–512
Lublin FD, Reingold SC, Cohen JA et al (2014) Defining the clinical course of multiple sclerosis. Neurology 83:278–286
Brownlee WJ, Hardy TA, Fazekas F et al (2017) Diagnosis of multiple sclerosis: progress and challenges. Lancet 388:1336–1346
Rovira A, Wattjes MP, Tintoré M et al (2016) MAGNIMS consensus guidelines on the use of MRI in multiple sclerosis—clinical implementation in the diagnostic process. Nat Rev Neurol 11:471–482
Thompson AJ, Banwell BL, Barkhof F et al (2018) Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol 17:162–173
McDonald WI, Compston A, Edan G et al (2001) Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the Diagnosis of Multiple Sclerosis. Ann Neurol 50:121–127
Polman CH, Reingold SC, Edan G et al (2005) Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald Criteria”. Ann Neurol 58:840–846
Polman CH, Reingold SC, Banwell B et al (2011) Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol 69:292–302
Lunde HMB, Assmus J, Myhr K-M et al (2017) Survival and cause of death in multiple sclerosis: a 60-year longitudinal population study. J Neurol Neurosurg Psychiatry 88:621–625
Kaufman DW, Reshef S, Golub HL et al (2014) Survival in commercially insured multiple sclerosis patients and comparator subjects in the US. Mult Scler Relat Disord 3:364–371
Comi G, Radaelli M, Soelberg Sørensen P (2017) Evolving concepts in the treatment of relapsing multiple sclerosis. Lancet 389:1347–1356
Jacobs LD, Beck RW, Simon JH et al (2000) Intramuscular interferon beta-1a therapy initiated during a first demyelinating event in multiple sclerosis. New Engl J Med 343:898–904
Comi G, Filippi M, Barkhof F et al (2001) Effect of early interferon treatment on conversion to definite multiple sclerosis: a randomised study. Lancet 357:1576–1582
The IFNB Multiple Sclerosis Study Group (1993) Interferon beta-1b is effective in relapsing-remitting multiple sclerosis. I. Clinical results of a multicenter, randomized, double-blind, placebo-controlled trial. Neurology 43:655–661
Comi G, Martinelli V, Rodegher M et al (2009) Effect of glatiramer acetate on conversion to clinically definite multiple sclerosis in patients with clinically isolated syndrome (PreCISe study): a randomised, double-blind, placebo-controlled trial. Lancet 374:1503–1511
Comi G, De Stefano N, Freedman MS et al (2012) Comparison of two dosing frequencies of subcutaneous interferon beta-1a in patients with a first clinical demyelination event suggested of multiple sclerosis (REFLEX): a phase 3 randomised controlled trial. Lancet Neurol 11:33–41
Miller AE, Wolinsky JS, Kappos L et al (2014) Oral teriflunomide for patients with a first clinical episode suggestive of multiple sclerosis (TOPIC): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Neurol 13:977–986
Goodin DS, Traboulsee A, Knappertz V et al (2012) Relationship between early clinical characteristics and long term disability outcomes: 16 year cohort study (follow-up) of the pivotal interferon β-1b trial in multiple sclerosis. J Neurol Neurosurg Psychiatry 83:282–287
Goodin DS, Reder AT, Traboulsee AL et al (2018) Predictive validity of NEDA in the 16- and 21-year follow-up from the pivotal trial of interferon beta-1b. Mult Scler J 1:1352458518773511. https://doi.org/10.1177/1352458518773511
Goodin DS, Reder AT, Ebers GC et al (2012) A randomized cohort study 21 years after the start of the pivotal IFNβ-1b trial. Neurology 78:1315–1322
Bermel RA, Weinstock-Guttman B, Bourdette D et al (2010) Intramuscular interferon beta-1a therapy in patients with relapsing-remitting multiple sclerosis: a 15-year follow-up study. Mult Scler 16:588–596
PRISMS Study Group and the University of British Columbia MS/MRI Analysis Group (2001) PRISMS-4: long-term efficacy of interferon-beta-1a in relapsing MS. Neurology 56:1628–1636
Cohen BA, Rivera VM (2010) PRISMS: the story of a pivotal clinical trial series in multiple sclerosis. Curr Med Res Opin 26:827–838
Ford C, Goodman AD, Johnson K et al (2010) Continuous long-term immunomodulatory therapy in relapsing multiple sclerosis: results from the 15-year analysis of the US prospective open-label study of glatiramer acetate. Mult Scler 16:342–350
Lublin FD, Cofield SS, Cutter GR et al (2017) Long-term follow-up of a randomized study of combination interferon and glatiramer acetate in multiple sclerosis: efficacy and safety results up to 7 years. Mult Scler Relat Disord 18:95–102
Miller DH, Chard DT, Ciccarelli O (2012) Clinically isolated syndromes. Lancet Neurol 11:157–169
Edan G, Kappos L, Montalbán X et al (2014) Long-term impact of interferon beta-1b in patients with CIS: 8-year follow-up of BENEFIT. J Neurol Neurosurg Psychiatry 85:1183–1189
Kappos L, Freedman MS, Polman CH et al (2009) Long-term effect of early treatment with interferon beta-1b after a first clinical event suggestive of multiple sclerosis: a 5-year active treatment extension of the phase 3 BENEFIT trial. Lancet Neurol 8:987–997
Kinkel RP, Dontchev M, Kollman C et al (2012) Association between immediate initiation of intramuscular interferon beta-1a at the time of a clinical isolated syndrome and long-term outcomes: a 10-year follow-up of the controlled high-risk avonex multiple sclerosis prevention study in ongoing neurological surveillance. Arch Neurol 69:183–190
Leist TP, Comi G, Cree BA et al (2014) Effect of oral cladribine on time to conversion to clinically definite multiple sclerosis in patients with a first demyelinating event (ORACLE MS): a phase 3 randomised trial. Lancet Neurol 13:257–267
Kappos L, Edan G, Freedman MS et al (2016) The 11-year long-term follow-up study from the randomized BENEFIT CIS trial. Neurology 87:978–987
Kister I, Bacon TE, Chamot E et al (2013) Natural history of multiple sclerosis symptoms. Int J MS Care 15:146–158
Penner I-K, Paul F (2017) Fatigue as a symptom or comorbidity of neurological diseases. Nat Rev Neurol 13:663–675
Melanson M, Grossberndt A, Klowak M et al (2010) Fatigue and cognition in patients with relapsing multiple sclerosis treated with interferon beta. Int J Neurosci 120:631–640
Solaro C, Gamberini G, Masuccio FG (2018) Depression in multiple sclerosis: Epidemiolgy, aetiology, diagnosis and treatment. CNS Drugs 32:117–133
Benedict RH, Morrow S, Rodgers J et al (2014) Characterizing cognitive function during relapse in multiple sclerosis. Multi Scler 20:1745–1752
Brochet B, Deloire MSA, Bonnet M et al (2008) Should SDMT substitute for PASAT in MSFC? A 5-year longitudinal study. Mult Scler 14:1242–1249
MSIF survey on employment and MS (2010) http://www.ms-sep.be/userfiles/files/MSIF%20survey%20on%20Employment%20and%20MS%20FINAL.pdf. Accessed 30 Jan 2017
Karampampa K, Gustavsson A, Miltenburger C et al (2012) Treatment experience, burden, and unmet needs (TRIBUNE) in multiple sclerosis: the costs and utilities of MS patients in Canada. J Popul Ther Clin Pharmacol 19(1):e11–e25
Tintoré M, Comabella M, Sastre-Garriga J et al (2016) 1000 clinically isolated syndromes (CIS): the ‘Barcelona CIS inception cohort’ ECTRIMS 2016, abstract 38862
Kinkel RP, Laforet G, You X (2015) Disease-related determinants of quality of life 10 years after clinically isolated syndrome. Int J MS Care 17:26–34
Sormani MP, Bruzzi P (2015) Can we measure long-term treatment effects in multiple sclerosis? Nat Rev Neurol 11:176–182
Kappos L, Traboulsee A, Constantinescu C et al (2006) Long-term subcutaneous interferon beta-1a therapy in patients with relapsing-remitting MS. Neurology 67:944–953
Cree B, Gourraud P-A, Oksenberg JR et al (2016) Long-term evolution of multiple sclerosis disability in the treatment era. Ann Neurol 80:499–510
Fox RJ, Cutter G (2016) Long-term registries. Answering tough questions with big data? Neurol Clin Pract 6:97–99
Acknowledgements
We thank Eva-Maria Wicklein for her support in reviewing and commenting on the manuscript. Medical writing support, including preparation of the drafts under the guidance of the authors, was provided by Ray Ashton, Richmond Medical Communications. All named authors meet the criteria of the International Committee of Medical Journal Editors for authorship for this manuscript, take responsibility for the integrity of the work as a whole and have given final approval for the version to be published.
Funding
The publication of this article was supported by Bayer AG. The views and opinions expressed in the article are those of the authors and not necessarily those of Bayer AG. The original BENEFIT trial was sponsored by Schering AG / Bayer AG.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Hans-Peter Hartung has received fees for consulting, serving on steering committees and data monitoring committees from Bayer Healthcare, Biogen, GeNeuro, Medimmune, Merck, Novartis, Roche, Sanofi Genzyme, Teva, with approval by the Rector of Heinrich-Heine-University. Jonas Graf has no conflicts of interest. David Kremer has received compensation for speaking for Grifols SA.
Rights and permissions
About this article
Cite this article
Hartung, HP., Graf, J. & Kremer, D. Long-term follow-up of multiple sclerosis studies and outcomes from early treatment of clinically isolated syndrome in the BENEFIT 11 study. J Neurol 267, 308–316 (2020). https://doi.org/10.1007/s00415-018-09169-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-018-09169-w