Abstract
Hypothalamus is a key brain region regulating several essential homeostatic functions, including the sleep–wake cycle. Alzheimer’s disease (AD) pathology affects nuclei controlling sleep–wake rhythm sited in this brain area. Since only post-mortem studies documented the relationship between hypothalamic atrophy and sleep–wake cycle impairment, we investigated in AD patients the possible hypothalamic in vivo alteration using 2-deoxy-2-(18F) fluoro-d-glucose ([18F]FDG) positron emission tomography ([18F]FDG PET), and its correlations with sleep impairment and cerebrospinal-fluid (CSF) AD biomarkers (tau proteins and β-amyloid42). We measured sleep by polysomnography, CSF AD biomarkers and orexin levels, and hypothalamic [18F]FDG PET uptake in a population of AD patients compared to age- and sex-matched controls. We documented the significant reduction of hypothalamic [18F]FDG PET uptake in AD patients (n = 18) compared to controls (n = 18) (p < 0.01). Moreover, we found the increase of CSF orexin levels coupled with the marked alteration of nocturnal sleep in AD patients than controls. We observed the significant association linking the reduction of both sleep efficiency and REM sleep to the reduction of hypothalamic [18F]FDG PET uptake in the AD group, which in turn negatively correlated with the total-tau/beta-amyloid42 ratio (index of more marked neurodegeneration). Moreover, controls but not AD patients showed [18F]FDG PET interconnections between hypothalamus and limbic system. We documented the in vivo dysfunction of hypothalamus in AD patients, which lost the physiological connections with limbic system and was correlated with both nocturnal sleep disruption and CSF AD biomarkers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The hypothalamus is one of the older and smaller brain areas. It contains highly conserved neural circuitries exerting basic life functions such as energy metabolism, fluid and electrolyte balance, thermoregulation, reproductive control, and the sleep–wake cycle [1]. In particular, hypothalamus has a critical role in controlling the sleep–wake rhythm [1]. In keeping with this observation, key regions regulating the sleep–wake cycle are sited in the hypothalamus: suprachiasmatic nucleus (SCN), tuberomammillary nucleus (TMN), and orexinergic and melanin-concentrating hormone (MCH) neurons [1]. The mutual interconnections between these areas ensure the physiological sleep–wake cycle [1]. Alzheimer’s disease (AD) pathology affects the hypothalamic region, which shows a substantial decrease in the neuronal population in post-mortem AD brains [2,3,4,5]. AD neuropathology is marked by the deposition of extracellular plaques of β-amyloid42 (Aβ42) peptides and intracellular neurofibrillary tangles (NFT) of abnormally hyperphosphorylated tau (p-tau) proteins [6]. AD is clinically characterized by memory loss and deterioration of cognition, but also sleep impairment and daytime napping represent symptoms owing to AD pathology [7,8,9,10,11,12,13]. Sleep impairment has been recently associated with pathological changes of cerebrospinal-fluid (CSF) biomarkers (Aβ42 and tau proteins) in AD patients, as well as post-mortem studies documented that sleep–wake cycle alteration is related to orexinergic system, SCN and ventrolateral preoptic/intermediate nucleus dysfunction in AD patients [5, 8, 14,15,16]. Therefore, the association between hypothalamic neuronal circuitries dysfunction and sleep impairment has been widely documented in AD pathology. However, studies aimed at evaluating the hypothalamic activity and the association between hypothalamic function and sleep architecture in AD patients are missing. Brain 2-deoxy-2-(18F) fluoro-d-glucose ([18F]FDG) positron emission tomography ([18F]FDG PET) actually represents a valid instrument for measuring brain, and thus hypothalamic, functional activity [17]. On these bases, to evaluate the possible in vivo alteration of hypothalamus and its correlation with sleep impairment and CSF biomarkers changes in AD patients, in this study we investigated sleep measured by polysomnography (PSG), CSF AD biomarkers and orexin levels, and hypothalamic [18F]FDG PET uptake in a population of AD patients compared to non-demented elderly controls.
Methods
Participants and study design
We included in our study consecutive drug-naïve AD patients admitted to the Neurology Clinic of the University of Rome “Tor Vergata”. All patients underwent a standard dementia screening including history, neurological examination, laboratory tests, EEG, neuropsychological testing counting Mini Mental State Examination (MMSE), brain MRI, [18F]FDG PET, and lumbar puncture (LP) for CSF analysis. All patients included in this study received the diagnosis of AD according to the recently proposed version of the diagnostic guidelines [18]. The biomarkers were considered positive for AD when decreased CSF levels of Aβ42 and the following abnormalities were observed: medial temporal lobe atrophy on MRI, cortical temporo-parietal hypometabolism on [18F]FDG PET, and increased CSF levels of total tau (t-tau) or p-tau [18].
We enrolled a group of non-demented controls similar for age and sex with AD patients, who underwent PSG, [18F]FDG PET, and LP for diagnostic purposes. In particular, those patients were admitted for suspected cognitive impairment, ruled out after diagnostic investigations. Accordingly, PSG did not document sleep disorders, LP did not show alteration of the CSF biomarkers analyzed, [18F]FDG PET did not detect pathological focal brain hypometabolisms, and neuropsychological testing resulted normal in those patients, who were then considered non-demented controls.
Patients and controls were required to fulfil the following entry criteria: no additional neurological or psychiatric disease; no intake of CNS active drugs; no use of caffeine, tobacco and/or alcohol at the time of the sleep laboratory investigation. On the other hand, exclusion criteria for patients and controls were: systemic and/or neurologic infectious, inflammatory or autoimmune diseases; diabetes; diagnosis of primary sleep disorders or other conditions interfering with sleep quality, such as symptomatic obstructive pulmonary disease and uncontrolled seizures; abnormal cell count (>4 cells/mcL) at the CSF sample analysis.
Patients and controls provided their informed consent to the study, which was approved by the Independent Ethical Committee of the University Hospital of Rome “Tor Vergata”.
Polysomnographic recordings
AD patients and controls underwent two consecutive PSG studies to evaluate nocturnal sleep (SOMNOscreen, SOMNOmedics GmbH, Randersacker, Germany) [19]. Electrodes were positioned according to the International 10–20 System. The montage consisted of two electrooculography channels, three electromyographic channels (chin and anterior tibialis muscles) and eight EEG channels (F4, C4, O2, A2, F3, C3, O1, A1). Cardiorespiratory parameters were assessed by recording oronasal flow, thoracic and abdominal movements (plethysmography), pulsoximetry and electrocardiography. Patients were also instructed to maintain the usual sleep schedule and report it in a sleep diary during the week before the test. The first night-sleep study was considered an adaptation period. The second PSG monitoring was considered for sleep analysis, which was performed according to standard criteria [20]. The following standard parameters were computed: time in bed (TIB, time spent in bed between lights off and lights on), sleep onset latency (SL, the time-interval between the lights off and the first sleep epoch), total sleep time (TST, the actual sleep time without SL and awakenings), sleep efficiency (SE, the ratio between TST and TIB), REM sleep latency (LREM, the time-interval between the sleep onset and the first epoch of REM), stage 1 of non-REM sleep (N1), stage 2 of non-REM sleep (N2), stage 3 of non-REM sleep (N3), REM sleep (REM), WASO. Sleep stages percentages were calculated during the TST. PSG scorers (CL, FP, FI) identified apnoea/hypopnoea events based on the international standard criteria of the American Academy of Sleep Medicine [20]. Leg movements were scored according to standard criteria [20]. Patients and controls with an apnea–hypopnea index (AHI) >15/h and periodic leg movement index (PLMI) >15/h at PSG recording were excluded.
CSF collection and analysis
CSF samples were obtained by LP performed in the decubitus position with an atraumatic needle, between 8:00 and 9:30 a.m, within 1–2 h after morning awakening, the day after the second PSG recording [21]. Blood specimens were obtained at the same time of the LP procedure. CSF samples were collected in polypropylene tubes using standard sterile techniques. The first 4 ml of CSF sample was used for total cell count. Another 4 ml of CSF sample was centrifuged to eliminate cells and cellular debris, and immediately frozen at −80 °C to measure orexin, t-tau, p-tau and Aβ42 levels. CSF Aβ42, t-tau and p-tau levels were determined according to previously published standard procedures, using commercially available sandwich enzyme-linked immunosorbent assays (ELISA) (Innotest β-Amyloid 1-42, Innotest h-T-tau, Innotest Phospho-T-tau 181; Innogenetics, Ghent, Belgium) [22]. The t-tau/Aβ42 ratio was also calculated, and the cut-off >0.52 was considered to represent the CSF AD profile [23]. CSF orexin levels were detected according to previously published standard procedures with commercially available ELISA kit (Orexin A/Hypocretin-1 EIA Kit; Phoenix Pharmaceuticals, Burlingame, CA), based on the principle of competitive enzyme immunoassay [22, 24]. The two researchers (MN, SB) who performed the analysis were blinded to the clinical status of participants. All the samples in the study were analyzed each time on the same ELISA plate, in duplicate and in random order. Experiments were replicated two times to confirm the values and to demonstrate the reliability of the assay. An external positive control included in the assay kit and internal positive controls (patients affected by narcolepsy type 1) were used as reference samples [24, 25].
[18F]FDG PET scanning analysis
According to other similar reports of our group in this field, [18F]FDG PET was performed after overnight fasting the day before PSG recordings. [18F]FDG i.v. injection was performed in each subject after controlling serum glucose level, which has to be in the range proposed by the guidelines of the European Association of Nuclear Medicine. All subjects were injected i.v. with 185–210 MBq of [18F]FDG and were hydrated with 500 ml of NaCl 0.9%. The PET system Discovery VCT (GE Medical Systems, Tennessee, USA) has been used to assess [18F]FDG brain distribution in all patients. More details concerning PET acquisition parameters are described in our previous studies [26].
Data and statistical analysis
PSG and CSF data analysis
Demographic, clinical CSF, and PSG data were analyzed using the commercial software Statistica 10.0 program; Statsoft Inc, Tulsa, OK, USA. All data achieved in AD and control groups were first tested for normality using the Kolmogorov–Smirnov test, after which appropriate statistical tests were applied to compare AD and control groups (Student t test for normally distributed data, Mann–Whitney U test for nonparametric data). In the AD and control groups, correlations between all the CSF biomarkers levels (orexin, Aβ42, t-tau, p-tau) and hypothalamic [18F]FDG PET uptake were performed separately considering the distribution of data using both Pearson (normal distribution) or Spearman (non-normal distribution) correlation tests. Finally, the additional multiple regression analysis among normally distributed data was performed. In particular, clinical (age and MMSE scores), CSF (orexin, t-tau/Aβ42 ratio), [18F]FDG PET bilateral hypothalamic uptake, and PSG data (TIB, TST, SE, SL, LREM, N1, N2, N3, REM, WASO) were considered for the multiple regression analysis. p value <0.05 was considered to be statistically significant.
[18F]FDG-PET analysis
We used statistical parametric mapping (SPM8, Wellcome Department of Cognitive Neurology, London, UK) implemented in Matlab R2012b (Mathworks, Natick, MA, USA) for the analysis of [18F]FDG PET data. Non-linear spatial normalization allows us to transform the [18F]FDG PET data into the Montreal Neurological Institute space. A specific template for spatial normalization was used [27]. The spatially normalized set of images was then smoothed with an 8 mm isotropic Gaussian filter to blur for individual variations in gyral anatomy and to increase the signal-to-noise ratio. Images have been globally normalized to 50 using proportional scaling to remove confounding effects to global cerebral glucose consumption changes, with a masking threshold of 0.8. The resulting statistical parametric maps, SPM[t], have been transformed into normal distribution (SPM[z]) unit. Correction of SPM coordinates to match the Talairach Coordinates was achieved by the subroutine implemented by Matthew Brett (http://www.mrc-cbu.cam.ac.uk/Imaging). Cerebral areas have been identified at a range from 0 to 3 mm from the corrected Talairach coordinates of the SPM output isocentres, after importing the corrected coordinates, by Talairach client (http://www.talairach.org/index.html). According to Bennett and colleagues SPMt-maps have been set at p < 0.05, corrected for multiple comparisons with the False Discovery Rate option at voxel level, and at p < 0.01 corrected for multiple comparisons at cluster level [28]. Those clusters containing more than 100 (5 × 5 × 5 voxels, i.e., 11 × 11 × 11 mm) contiguous voxels have been accepted as significant [28]. The comparison between AD and control groups was performed by means of the ‘two-sample t test’ study design model, using an inclusive mask of the hypothalamus (WFU pickatlas tool implemented in SPM 8) [29]. We used age and sex as covariates in this analysis. The relationships between [18F]FDG hypothalamic distribution and the CSF orexin levels was evaluated using a ‘regression analysis’ design model with an inclusive mask of the hypothalamus (WFU pickatlas, see above [29]). Sex, age and CSF AD biomarkers data were used as covariates in the regression analysis. The cluster obtained by this latter analysis was then exported by means of WFU Pickatlas tool and further analyzed after a normalization process. In particular, the mean signal intensities computed by each cluster were normalized within each subject to the average intensities of the cerebellum volume of interest, as defined by other similar reports of our group in this field [26, 30]. The use of a normalization based upon activity in the cerebellum, instead of whole brain counts as in the reference region, was reported to result in a higher accuracy in distinguishing patients from controls in neurodegenerative diseases [31]. As proposed previously by Pagani et al. [32], a dataset including normalized [18F]FDG PET values relevant to the examined cluster has been exported. To determine if cerebellum-normalized [18F]FDG values for the cluster examined were of Gaussian distribution, the D’Agostino K squared normality test has been applied (where the null hypothesis is that the data are normally distributed).
The comparison of [18F]FDG brain glucose consumption of hypothalamic region between AD patients and controls was assessed with an inclusive mask of the hypothalamus obtained using the WFU PickAtlas [29, 31]. As reported previously by our group, a connectivity relationship analysis was performed based on voxel-wise interregional correlation analysis (IRCA) of SPM within 18F[FDG] PET data using population-based cytoarchitectonic seed brain regions as previously proposed [33]. For IRCA analysis, extracted mean regional VOI counts were then normalized (see above) and used as covariate to find regions showing significant (corrected <0.05) voxel-wise correlations across scans (subjects) using SPM8 [34].
Results
Demographic and clinical data
Thirty-six consecutive AD patients were screened from September 2015 to September 2016. Among these AD patients, 18 presented some exclusion criteria for this study and were excluded. In particular: 6 patients showed an AHI >15/h OSA at PSG recording, 2 patients showed PLMI >15/h at PSG recording, 1 had abnormal cell count at CSF analysis, 4 reported intake of CNS active drugs, 5 were diabetic. Therefore, 18 AD patients were included in the study and compared to 18 age- and sex-matched controls (Table 1).
CSF data
We found higher CSF orexin levels in AD patients compared to controls (165.33 ± 58.07 vs 145.26 ± 36.91, p < 0.05, see Table 1). As expected, higher CSF t-tau and p-tau levels and lower CSF Aβ42 levels were found in the AD group compared to control group. In addition, AD patients showed higher CSF t-tau/Aβ42 ratio with respect to controls.
CSF data of AD patients and controls were reported in Table 1.
PSG data
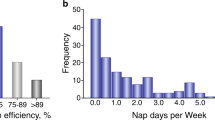
Reduced TST, SE, and N3 were documented in AD patients compared to controls (see Table 2). Moreover, higher WASO, SL, and N1 were found in AD patients than controls (see Table 2). Finally, REM sleep dysregulation was documented in the AD group, as shown by the reduction of REM sleep and the increase of LREM with respect to controls (Table 2).
[18F]FDG PET data
We documented the significant reduction of global hypothalamic [18F]FDG PET uptake in the AD group compared to the control group (0.81 ± 0.08 vs 0.90 ± 0.04, p < 0.05, see Table 3; Fig. 1). We also documented both the right and left hypothalamic [18F]FDG PET uptake reduction in the AD group compared to the control group (Table 3).
T1-weighted brain MRI sequences superimposition showing the significant reduction of glucose consumption in the right (a) and left (b) hypothalamus of AD patients compared to controls (Talairach coordinates −8 −6 −5 for left hypothalamus and 4 −4 −2 for right hypothalamus). An inclusive mask with WFU pickatlas was generated (see text). R right; L left
When comparing AD and control groups by SPM analysis (see methods section), we found a significant reduction of brain glucose consumption in the left and right hypothalamus of AD patients: cluster p(FWE-corrected) = 0.001; cluster p(FDR-corrected) = 0.003; cluster extent = 764; Z score of maximum = 5.44; Talairach coordinates: −8 −6 −5 and 4 −4 −2, respectively.
Connectivity Analysis of [18F]FDG PET data
The connectivity analysis performed in the control group showed a significant positive correlation between [18F]FDG glucose consumption in hypothalamus and in the bilateral Brodmann area (BA) 24, owing to the limbic system (see Table 4; Fig. 2). Notably, these interconnections were not documented in the AD group. We did not find other significant positive or negative correlations between brain glucose consumption in hypothalamus and [18F]FDG uptake in the rest of the brain in both AD and control groups.
Multiple axial views of T1-weighted brain MRI sequences superimposition showing the significant positive relationship between brain glucose consumption in hypothalamus and in both left and right Brodmann area 24 (anterior cingulate cortex; Talairach coordinates: 8, 24, 20 and 4, 38, 4 for right Limbic cortex and 0, 18, 24 for left limbic cortex) in controls. Coordinates are reported in Table 4
Correlations in the AD group
Considering the correlation analysis between CSF and [18F]FDG PET data in the AD group, we documented the significant negative correlation between the t-tau/Aβ42 ratio and the hypothalamic [18F]FDG PET uptake (R = −0.47, p < 0.05). Conversely, we did not find significant correlations in the control group. Remarkably, CSF orexin levels did not correlate with the hypothalamic [18F]FDG PET uptake in both AD and control groups.
The additional multivariate regression analysis was performed in the AD group among clinical (age and MMSE scores), CSF (orexin, t-tau/Aβ42 ratio), [18F]FDG PET bilateral hypothalamic uptake, and PSG data (TIB, TST, SE, SL, LREM, N1, N2, N3, REM, WASO), and showed a significant interplay between the reduction of both SE and REM sleep and the reduction of [18F]FDG PET hypothalamic uptake (β = 0.63 and p < 0.0001, β = 0.92, p < 0.0001, respectively). We did not find other significant mutual relationships among the data analyzed in the multiple regression model performed in the AD group.
Discussion
The present study documented the in vivo hypothalamic dysfunction in AD patients. Moreover, the reduced hypothalamic [18F]FDG uptake was associated with both sleep impairment and higher t-tau/Aβ42 ratios (sign of a more marked AD neurodegeneration). Hence, the present findings supported the suggestion that hypothalamus is altered by AD pathology and its dysregulation may be related to sleep impairment in AD patients.
Hypothalamus controls several homeostatic functions such as growth, metabolism, autonomic homeostasis, reproduction, and the sleep–wake cycle [1, 3]. These essential functions are frequently altered in AD patients; indeed, hypothalamus is significantly affected by AD pathology [3]. The hypothalamic alteration owing to AD neurodegeneration may be responsible for several non-cognitive deficits present in AD patients. In particular, weight loss, sleep–wake disorders and neuroendocrine alterations are attributable to the hypothalamic dysfunction caused by AD pathology [3]. Several post-mortem studies have reported β-amyloid plaque deposition and NFT of tau pathology in the hypothalamus of AD patients [3]. In particular, recent studies demonstrated that the reduction of neuronal populations of both SCN and ventrolateral/intermediate nucleus are associated with sleep impairment and rest–activity circadian rhythm alteration in AD patients [14, 15]. Nevertheless, also the reduction of orexinergic nucleus and TMN populations has been documented in the hypothalamus of AD patients [4, 5]. However, although several post-mortem studies reported the significant atrophy of hypothalamus in the brain of AD patients, fewer studies investigated the in vivo alteration of the hypothalamic function in AD patients [35]. Furthermore, evidence of the interplay between hypothalamic dysfunction and both sleep and CSF biomarkers levels have not been currently reported. Recent studies coupling CSF and polysomnographic recordings have reported that increased CSF orexin levels, expression of an upregulated orexinergic tone, are related to REM sleep impairment and nocturnal wakefulness in patients affected by AD pathology [8, 16]. Consistently, the increment of CSF orexin levels has been also associated with the impairment of sleep dysregulation in patients showing biomarkers consistent with AD pathology [8, 16]. Moreover, CSF orexin levels have been negatively correlated with wake fragmentation and diurnal nappings in AD patients [36]. Since several hypothalamic nuclei are considered regulating the sleep–wake cycle in AD patients [8, 14,15,16], this study was focused in evaluating the relationships between sleep and hypothalamic [18F]FDG PET uptake. Both PSG and [18F]FDG PET are considered gold standard tools to study sleep structure and brain functional activity, respectively [37].
PSG remains the gold standard for measuring sleep, since it is a well-validated approach to study and define sleep architecture, also in neurodegenerative diseases [37]. Accordingly, PSG-based studies documented REM sleep dysregulation, reduced sleep quality, increased nocturnal wakefulness, and diurnal napping in AD patients [8,9,10,11,12,13, 38]. Moreover, REM and slow wave sleep impairment are related to CSF AD biomarkers and orexin levels in AD patients [8]. In the present study, we confirmed sleep dysregulation and CSF orexin levels increase in AD patients.
[18F]FDG PET has been widely used during the last decade to study the physiopathology of AD [17]. In keeping with its intrinsic features, [18F]FDG PET is actually considered a sensitive biomarker to support the diagnosis of AD [39, 40], since it recognizes neurons disconnection, synaptic dysfunction and neurotransmission deregulation [41]. However, it can also represent an instrument able to investigate the steady-state integrity of different neuronal circuitries, including hypothalamic interconnections [40, 41]. A single study, investigating the interactions between brain axons tract integrity and glucose metabolism in a selection of brain areas, documented the reduction of [18F]FDG uptake in the hypothalamus of patients affected by mild cognitive impairment who progressed to AD [35]. Therefore, studies primarily focused at investigating hypothalamus in AD patients by means of [18F]FDG PET are missing. In the present report, we found the reduced hypothalamic [18F]FDG uptake in AD patients and its correlation with the t-tau/Aβ42 ratio. This ratio has been largely considered as a marker of more severe neurodegeneration [23]; thus we showed that hypothalamic dysregulation correlates with a more severe degree of neurodegeneration in AD patients.
The novelty of this study lies in the observation that the reduced hypothalamic [18F]FDG uptake is related to the alteration of sleep, and in particular REM sleep. This finding is not unexpected since several hypothalamic nuclei concur to the generation of REM sleep [42]. REM sleep may be early affected by AD, since the cholinergic inefficiency caused by the AD pathological process impairs its regulation [11]. Nevertheless, also orexinergic and MCH-ergic nuclei participate in the regulation of REM sleep [43, 44]. In particular, MCH-ergic nucleus has been recently associated with the induction of REM sleep; conversely, orexinergic activity suppresses REM sleep [44]. We recently documented that REM sleep suppression is associated with an increased orexinergic tone in AD patients [8, 16]. However, in this study we did not find association between CSF orexin levels and hypothalamic [18F]FDG uptake. This lack of correlation could be explained by the fact that orexinergic neurons represent a very limited region of the hypothalamus. In agreement with this observation, studies investigating the alteration of orexinergic neurons in narcolepsy, a sleep disorder caused by the orexinergic system inefficiency, did not find hypothalamic [18F]FDG PET modifications [45, 46]. A possible explanation of this lack of correlation is the small dimension of hypothalamus (< 5 mm), which hampers the [18F]FDG PET detection. Future studies, possibly with advanced PET detector characteristics or by means of PET/MRI systems may improve this analysis. A further finding of the present study is the physiological interconnections found in the control group between the hypothalamic region and the bilateral BA 24, brain regions owing to the limbic system. However, the connectivity analysis performed in AD patients did not document these interconnections. This finding is in agreement with several studies documenting the significant alteration of the limbic system circuitries in AD patients [47]. Further studies will establish the direction of causation of these missing interconnections in AD patients, since both limbic and hypothalamic atrophies may cause this disconnection.
We are aware that this study presents several limitations. The sample size is small and did not allow further investigations, thus limiting potential associations in the multiple regression model. Future analyses should better address the association found between the hypothalamic dysfunction and CSF biomarkers of neurodegeneration in AD patients, also testing the possible influence of sleep impairment on this relationship. Moreover, the control group is not constituted by healthy volunteers, but by patients admitted for suspected cognitive impairment, which was ruled out after diagnostic investigation. Finally, we analyzed our data using the mean signal intensities of each cluster to normalize participant to the average intensities of the cerebellar VOI, and not using other more validated analysis procedures [48].
In conclusion, based on the results of this study showing the influence of hypothalamic dysfunction on sleep in AD patients, we documented once again the importance of hypothalamic dysregulation in the AD neurodegeneration. Therefore, we suggest the expansion of the current knowledge about the role of hypothalamus in the non-cognitive clinical symptoms of AD. In particular, hypothalamic and orexinergic circuitries alteration and its relationships with sleep dysregulation needs further investigations, to provide new directions in biomarkers research and therapeutic approaches.
References
Saper CB, Lowell BB (2014) The hypothalamus. Curr Biol 24(23):R1111–R1116
Baloyannis SJ, Mavroudis I, Mitilineos D, Baloyannis IS, Costa VG (2015) The hypothalamus in Alzheimer’s disease: a Golgi and electron microscope study. Am J Alzheimers Dis Other Demen 30(5):478–487
Ishii M, Iadecola C (2015) Metabolic and non-cognitive manifestations of Alzheimer’s disease: the hypothalamus as both culprit and target of pathology. Cell Metab 22(5):761–776
Shan L, Bossers K, Unmehopa U, Bao AM, Swaab DF (2012) Alterations in the histaminergic system in Alzheimer’s disease: a postmortem study. Neurobiol Aging 33(11):2585–2598
Fronczek R, van Geest S, Frölich M, Overeem S, Roelandse FW, Lammers GJ, Swaab DF (2012) Hypocretin (orexin) loss in Alzheimer’s disease. Neurobiol Aging 33(8):1642–1650
Yaari R, Corey-Bloom J (2007) Alzheimer’s disease. Semin Neurol 27(1):32–41
Vitiello MV, Prinz PN (1989) Alzheimer’s disease. Sleep and sleep/wake patterns. Clin Geriatr Med 5(2):289–299
Liguori C, Romigi A, Nuccetelli M et al (2014) Orexinergic system dysregulation, sleep impairment, and cognitive decline in Alzheimer disease. JAMA Neurol 71(12):1498–1505
Beaulieu-Bonneau S, Hudon C (2009) Sleep disturbances in older adults with mild cognitive impairment. Int Psychogeriatr 21(4):654–666
Bonanni E, Maestri M, Tognoni G et al (2005) Daytime sleepiness in mild and moderate Alzheimer’s disease and its relationship with cognitive impairment. J Sleep Res 14(3):311–317
Montplaisir J, Petit D, Lorrain D et al (1995) Sleep in Alzheimer’s disease: further considerations on the role of brainstem and forebrain cholinergic populations in sleep-wake mechanisms. Sleep 18(3):145–148
Maestri M, Carnicelli L, Tognoni G et al (2015) Non-rapid eye movement sleep instability in mild cognitive impairment: a pilot study. Sleep Med 16(9):1139–1145
Power AE (2004) Slow-wave sleep, acetylcholine, and memory consolidation. Proc Natl Acad Sci USA 101:1795–1796
Wang JL, Lim AS, Chiang WY et al (2015) Suprachiasmatic neuron numbers and rest-activity circadian rhythms in older humans. Ann Neurol 78(2):317–322
Lim AS, Ellison BA, Wang JL et al (2014) Sleep is related to neuron numbers in the ventrolateral preoptic/intermediate nucleus in older adults with and without Alzheimer’s disease. Brain 137(Pt 10):2847–2861
Liguori C, Nuccetelli M, Izzi F et al (2016) Rapid eye movement sleep disruption and sleep fragmentation are associated with increased orexin-A cerebrospinal-fluid levels in mild cognitive impairment due to Alzheimer’s disease. Neurobiol Aging 40:120–126
Varrone A, Asenbaum S, Vander Borght T et al (2009) European Association of Nuclear Medicine Neuroimaging Committee. EANM procedure guidelines for PET brain imaging using [18F]FDG, version 2. Eur J Nucl Med Mol Imaging 36(12):2103–2110
McKhann GM, Knopman DS, Chertkow H et al (2011) The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7(3):263–269
Romigi A, Liguori C, Placidi F et al (2014) Sleep disorders in spinal and bulbar muscular atrophy (Kennedy’s disease): a controlled polysomnographic and self-reported questionnaires study. J Neurol 261(5):889–893
Iber C, Ancoli-Israel S, Chesson A, Quan S, for the American Academy of Sleep Medicine (2007) The AASM manual for the scoring of sleep and associated events; rules, terminology and technical specifications, 1st edn. American Academy of Sleep Medicine, Westchester
Liguori C, Olivola E, Pierantozzi M et al (2016) Cerebrospinal-fluid Alzheimer’s disease biomarkers and blood-brain barrier integrity in a natural population of cognitive intact Parkinson’s disease patients. CNS Neurol Disord Drug Targets. 5 Dec 2016. [Epub ahead of print]
Liguori C, Placidi F, Albanese M et al (2014) CSF beta-amyloid levels are altered in narcolepsy: a link with the inflammatory hypothesis? J Sleep Res 23(4):420–424
Duits FH, Teunissen CE, Bouwman FH et al (2014) The cerebrospinal fluid “Alzheimer profile”: easily said, but what does it mean? Alzheimers Dement 10:713–723
Liguori C, Romigi A, Mercuri NB et al (2014) Cerebrospinal-fluid orexin levels and daytime somnolence in frontotemporal dementia. J Neurol 261(9):1832–1836
Liguori C, Placidi F, Izzi F et al (2016) Beta-amyloid and phosphorylated tau metabolism changes in narcolepsy over time. Sleep Breath 20(1):277–283
Alessandrini M, Micarelli A, Chiaravalloti A et al (2014) Cerebellar metabolic involvement and its correlations with clinical parameters in vestibular neuritis. J Neurol 261(10):1976–1985
Della Rosa PA, Cerami C, Gallivanone F et al (2014) A standardized [18F]-FDG-PET template for spatial normalization in statistical parametric mapping of dementia. Neuroinformatics 12(4):575–593
Bennett CM, Wolford GL, Miller MB (2009) The principled control of false positives in neuroimaging. Soc Cogn Affect Neurosci 4(4):417–422
Lancaster JL, Rainey LH, Summerlin JL et al (1997) Automated labeling of the human brain: a preliminary report on the development and evaluation of a forward-transform method. Hum Brain Mapp 5(4):238–242
Liguori C, Chiaravalloti A, Sancesario G et al (2016) Cerebrospinal fluid lactate levels and brain [18F]FDG PET hypometabolism within the default mode network in Alzheimer’s disease. Eur J Nucl Med Mol Imaging 43(11):2040–2049
Soonawala D, Amin T, Ebmeier KP et al (2002) Statistical parametric mapping of (99 m)Tc-HMPAO-SPECT images for the diagnosis of Alzheimer’s disease: normalizing to cerebellar tracer uptake. Neuroimage 17(3):1193–1202
Pagani M, De Carli F, Morbelli S et al (2014) Volume of interest-based [18F]fluorodeoxyglucose PET discriminates MCI converting to Alzheimer’s disease from healthy controls A European Alzheimer’s Disease Consortium (EADC) study. Neuroimage Clin 7:34–42
Lee DS, Kang H, Kim H et al (2008) Metabolic connectivity by interregional correlation analysis using statistical parametric mapping (SPM) and FDG brain PET; methodological development and patterns of metabolic connectivity in adults. Eur J Nucl Med Mol Imaging 35(9):1681–1691
Maldjian JA, Laurienti PJ, Kraft RA, Burdette JH (2003) An automated method for neuroanatomic and cytoarchitectonic atlas-based interrogation of fMRI data sets. Neuroimage 19(3):1233–1239
Cross DJ, Anzai Y, Petrie EC et al (2013) Loss of olfactory tract integrity affects cortical metabolism in the brain and olfactory regions in aging and mild cognitive impairment. J Nucl Med 54(8):1278–1284
Friedman LF, Zeitzer JM, Lin L et al (2007) Alzheimer disease, increased wake fragmentation found in those with lower hypocretin-1. Neurology 68(10):793–794
Naismith SL, Lewis SJ, Rogers NL (2011) Sleep-wake changes and cognition in neurodegenerative disease. Prog Brain Res 190:21–52
Prinz PN, Vitaliano PP, Vitiello MV et al (1982) Sleep, EEG and mental function changes in senile dementia of the Alzheimer’s type. Neurobiol Aging 3(4):361–370
Herholz K (2003) PET studies in dementia. Ann Nucl Med 17(2):79–89
Mosconi L (2013) Glucose metabolism in normal aging and Alzheimer’s disease: methodological and physiological considerations for PET studies. Clin Transl Imaging. doi:10.1007/s40336-013-0026-y
Rocher AB, Chapon F, Blaizot X, Baron JC, Chavoix C (2003) Resting-state brain glucose utilization as measured by PET is directly related to regional synaptophysin levels: a study in baboons. Neuroimage. 20(3):1894–1898
Shan L, Dauvilliers Y, Siegel JM (2015) Interactions of the histamine and hypocretin systems in CNS disorders. Nat Rev Neurol 11(7):401–413
Lu J, Sherman D, Devor M, Saper CB (2006) A putative flip-flop switch for control of REM sleep. Nature 441(7093):589–594
Konadhode RR, Pelluru D, Blanco-Centurion C et al (2013) Optogenetic stimulation of MCH neurons increases sleep. J Neurosci 33(25):10257–10263
Dauvilliers Y, Comte F, Bayard S et al (2010) A brain PET study in patients with narcolepsy–cataplexy. J Neurol Neurosurg Psychiatry 81(3):344–348
Huang YS, Liu FY, Lin CY et al (2016) Brain imaging and cognition in young narcoleptic patients. Sleep Med 24:137–144
Bozzali M, Padovani A, Caltagirone C, Borroni B (2011) Regional grey matter loss and brain disconnection across Alzheimer disease evolution. Curr Med Chem 18(16):2452–2458
Schmahmann JD, Doyon J, McDonald D et al (1999) Three-dimensional MRI atlas of the human cerebellum in proportional stereotaxic space. Neuroimage 10(3 Pt 1):233–260
Acknowledgements
We thank Prof. Carlo Chiaramonte for helping us in the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Claudio Liguori, Agostino Chiaravalloti, Nicola Biagio Mercuri, Marzia Nuccetelli, Giuseppe Sancesario, Francesca Izzi, Andrea Cimini, Sergio Bernardini, Orazio Schillaci, and Fabio Placidi declare no conflict of interest or financial disclosures.
Rights and permissions
About this article
Cite this article
Liguori, C., Chiaravalloti, A., Nuccetelli, M. et al. Hypothalamic dysfunction is related to sleep impairment and CSF biomarkers in Alzheimer’s disease. J Neurol 264, 2215–2223 (2017). https://doi.org/10.1007/s00415-017-8613-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-017-8613-x