Abstract
This retrospective study was conducted to determine the relationship between variable factors and the recurrence rate of post-semicircular canal benign paroxysmal positional vertigo (PSC-BPPV) after canalith repositioning procedure (CRP). Patients with PSC-BPPV were diagnosed by history and the presence of a positive Dix–Hallpike maneuver between 2008 and 2010. In total, 243 patients (47 males and 196 females, average age = 57.5 years) treated with Epley’s maneuver or canalith repositioning procedure (CRP) were included in the study. The demographic factors studied were age, sex, sleep disorders, inner ear diseases, head trauma history, and cardiovascular diseases. Multivariate statistics using SPSS version 15, Pearson’s Chi-squared test (χ 2), Kaplan–Meier analysis, log-rank test, and Cox proportional hazards regression model were used for the analysis. The success rate of vertigo control after the initial CRP was 83.1 %. Pearson’s χ 2 test results showed that females and participants with sleep disorders exhibited a significant difference in the recurrence of vertigo after the initial CRP. In addition, the Kaplan–Meier analysis and log-rank test survival analysis revealed that the recurrence was associated with females and participants with sleep disorders and inner ear diseases. However, Cox proportional hazards regression showed no differences in recurrences associated with old age, sex, sleep disorders, inner ear diseases, head trauma, and cardiovascular diseases. Epley’s maneuver or CRP is an effective, safe, and simple treatment for BPPV. Females and participants with sleep disorders and inner ear diseases are likely associated with the recurrence of BPPV after CRP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dizziness is a major complaint of elderly people. The most common cause (approximately 26 %) of dizziness reported in elderly patients is benign paroxysmal positional vertigo (BPPV) [1]. The prevalence of BPPV increases with age [2–4]. BPPV is observed in approximately 20 % [5] of patients with dizziness and contributes up to 43 % of the patient population in otology clinics [4]. BPPV is exacerbated by sudden head movements, especially when lying down, bending forward (e.g., when tying shoes), turning on the bed, looking upward, or reaching for high objects (bookshelf syndrome). The attack duration is typically brief (<60 s), and the most prominent symptom of BPPV is vertigo occurring when a patient rolls into a lateral position on a bed [6].
Although the etiology of BPPV is mostly idiopathic (approximately 50–70 %) [7], an increased susceptibility of the condition is likely caused by head and neck traumas, advanced age, vestibular degeneration, and other ear disorders and ear surgeries [4].
The success rate of the canalith repositioning procedure (CRP; also known as canalith repositioning maneuver) for BPPV is approximately 70–90 % [8]. The Semont’s manoeuvre is also used, like Epley’s, to treat posterior canal canalolithiasis. The Lempert maneuver is used for treating horizontal canal canalithiasis, and the Hamid maneuver is used for treating horizontal canal cupulolithiasis [9]. Epley’s initial publication on the use of bedside treatment for benign paroxysmal positional vertigo reported a success rate of 80 % after a single treatment session and a success rate of 100 % after more than one treatment sessions [6]. Despite the high success rate, vertigo may recur after a few months. Nevertheless, CRP remains the first choice of treatment when BPPV recurs.
Nunez et al. [7] showed that the rate of symptom resolution after the CRP in patients after acute vestibulopathy was 94.1 %, with a recurrence rate of 37.5 % (after an average of 12.8 months). For the idiopathic group, the resolution rate was 90.5 %, with a recurrence rate of 22.1 % (after an average of 15.9 months).
Some studies have found BPPV was associated with sleep disorders. In Korres et al. [10], vertigo in most patients (75.9 %) was associated with sleep disorders. Common sleep disorders include insomnia (inability to sleep), sleep apnea, narcolepsy, sleepwalking, night tremors, periodic limb movement disorder, restless legs syndrome, bruxism (involuntary grinding or clenching of the teeth during sleep), and nocturia. Moreover, past medical history is likely related to recurrence. Several studies have investigated the comorbidities of BPPV including age, sex, head trauma, Meniere’s disease, and vestibulitis, whereas the etiology of it with sleep disorders remain scarcely discussed [7, 8, 11, 12]. In the present study, we analyzed variable factors associated with recurrence of posterior canal BPPV (PC-BPPV) patients treated with CRP.
Materials and methods
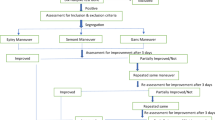
This retrospective study investigated the recurrence of posterior BPPV after treatment with Epley’s maneuver. The study was approved by the hospital’s institutional review board (13MMHIS054). We reviewed hundreds of patients diagnosed with PC-BPPV using Dix–Hallpike maneuvers from 2008 to 2010 and immediately treated with the Epley’s maneuver. A positive Dix–Hallpike maneuver was defined by the presence of an upbeating and torsional nystagmus with the top pole of rotation beating toward the affected ear [13, 14].
Participants aged <20 years and those with atypical posterior BPPV (including anterior canal BPPV, horizontal BPPV, bilateral canal or multiple canal BPPV, and contralateral posterior BPPV evoked after CRP and BPPV of idiopathic nature) were excluded. In total, 247 participants with typical PC-BPPV were recruited as study participants after a follow-up of at least 2 years until 2012. During follow-up at the clinic, Dix–Hallpike tests were performed to evaluate the result. If nystagmus was detected, Epley’s maneuver was performed again. The treatment was considered successful when neither nystagmus nor vertigo was detected. The recurrence of BPPV is clinically defined as the detection of vertigo evoked by changing position 3 months after successful treatment with Epley’s maneuver.
Patient history, including the number of episodes of vertigo, the number of times Epley’s maneuver was performed, age, sex, and history [hypertension, hyperlipidemia, diabetes, and heart disease, sleep disorders (International Classification of Diseases, 9th edition, Clinical Modification codes 780.50, 780.51 m, 780.52, and 789.59), head trauma, and inner ear diseases (vestibulitis, sudden sensorial hearing loss, and Menière disease)] was recorded. In 2013 and 2014, we contacted all participants over the telephone to obtain additional information regarding recurrence. Four participants died during the follow-up period. Thus, data of 243 participants were analyzed using SPSS statistical software (version 15).
Risk factors associated with the recurrence of BPPV were compared using Pearson’s Chi-squared (χ 2) test. The recurrence until the end of follow-up was compared using Kaplan–Meier estimates and the log-rank test, with cases censored at the end of the follow-up. In addition, a multivariate Cox proportional hazards regression analysis was performed to compare recurrence by age, sex, sleep disorders, head trauma, inner ear diseases, and cardiovascular diseases.
Results
Of the 243 participants, 202 (83.1 %) were treated successfully after a single CRP session, 24 after 2 sessions, 6 participants after 3 sessions, 8 participants after 4 sessions, 2 participants after 5 sessions, and 1 participant after 6 sessions. Regarding risk factors associated with BPPV, none were observed were observed in 126 participants (51.9 %), sleep disorders in 40 participants (16.5 %), head trauma in 11 participants (4.7 %), inner ear diseases in 25 participants (10.3 %), and cardiovascular diseases in 80 participants (32.9 %). Among the 243 participants, 46 were classified into the recurrence group and 197 into the nonrecurrence group. The average age of the participants was 57.5 ± 13.9 years (age range = 25–87 years). The age distribution is shown in Fig. 1.
Table 1 presents the results for the recurrence and nonrecurrence groups obtained using Pearson χ 2 test. The results for females (P = 0.042) and participants with sleep disorders (P = 0.005) differed significantly. However, the results for elderly participants aged ≥65 years (P = 0.673) and participants with head trauma (P = 0.948), inner ear diseases (P = 0.078), and cardiovascular diseases (P = 0.091) did not differ significantly.
The results of the Kaplan–Meier estimates are as follows:
The recurrence rates at 12 and 24 months were 16 and 20 % in participants <65 years, respectively, and 18 and 20 % in participants >65 years, respectively (Fig. 2). The differences were nonsignificant (P = 0.766).
The recurrence rates at 12 and 24 months were 7 and 11 % in males, respectively, and 19 and 20 % in females, respectively (Fig. 3). The differences were significant (P = 0.049). Mean recurrence of BPPV was higher in females than in males.
The recurrence rates at 12 and 24 months were 14 and 17 % in participants without sleep disorders, respectively, and 30 and 40 % in participants with sleep disorders, respectively (Fig. 4). The differences were significant (P = 0.002). Mean recurrence of BPPV was higher in participants with sleep disorders than in those without.
The recurrence rates at 12 and 24 months were 18 and 18 % in participants without head trauma, respectively, and 17 and 20 % in participants with head trauma, respectively (Fig. 5). The differences were nonsignificant (P = 0.975).
The recurrence rates at 12 and 24 months were 15 and 19 % in participants without inner ear diseases, respectively, and 28 and 36 % in participants with inner ear diseases, respectively (Fig. 6). The differences were significant (P = 0.042). Mean recurrence was higher in participants with inner ear diseases.
The recurrence rates at 12 and 24 months were 14 and 17 % in participants without cardiovascular diseases, respectively, and 16 and 23 % in participants with cardiovascular diseases, respectively (Fig. 7). The differences were nonsignificant (P = 0.077).
To summarize, the recurrence of BPPV was compared according to sex, age, and comorbidities—namely sleep disorders, inner ear diseases, cardiovascular diseases, and head trauma—using Kaplan–Meier estimates and the log-rank test. The recurrence rates did not differ significantly when stratified by age (P = 0.680), head trauma status (P = 0.975), and cardiovascular disease status (P = 0.077). However, significant differences in recurrence rates were observed when stratified by sex (P = 0.049) and presence of sleep disorders (P = 0.002) and inner ear diseases (P = 0.042).
Finally, a multivariate Cox proportional hazards regression analysis was performed to compare recurrence-free survival by ethnicity. The prespecified Cox proportional hazards analysis showed that no significant difference in BPPV recurrence in age (P = 0.735), sex (P = 0.639), sleep disorders (P = 0.621), head trauma (P = 0.409), inner ear diseases (P = 0.774), or cardiovascular diseases (P = 0.686) (Table 2).
Discussion
The short term effectiveness of Epley’s maneuver in the present study was satisfactory. Among 243 participants, 202 completely recovered within 1 week. The success rate of the procedure was 83.1 %, consistent with that observed in other studies (80.2–98 %) [8, 12, 15–19]. Therefore, Epley’s CRP remains the first treatment choice for P-BPPV.
Among the 243 participants in our study (age range 25–88 years), the age distribution of the elderly participants was as follows: 51–59 years, 65 participants (26.7 %) and 61–69 years, 53 participants (21.8 %). The proportion of participants aged 50–70 years was 48.5 %, almost half that observed in other related studies [20, 21]. 199 females and 48 males were considered for the final analysis. This ratio is consistent with those observed in other studies [12, 15, 22].
Of the 243 participants, 126 participants (51 %) exhibited idiopathic factors, which is again consistent with the literature (50–70 %) [8, 12, 15, 23]. In total, 25 participants (10.5 %) exhibited inner ear diseases, including vestibular neuronitis (15 participants), unilateral sensorial hearing loss (5), and Meniere disease (5). Head trauma was noted in 11 participants (5.2 %); this proportion was slightly lower than that observed in previous studies (8.5–27 %) [8, 11, 15]. In the present study, 40 participants (16.5 %) exhibited sleep disorders. In Korres et al. [10], 155 patients with vertigo (75.9 %) had sleep disorders. In our subgroup of participants with sleep disorders, most experienced long-term insomnia and were under medication. Some participants seldom experienced poor sleep, and some attributed their abnormal sleep patterns to shift work (Circadian rhythm sleep disorder). In the present study, 81 participants (32.8 %) had cardiovascular diseases. In the study by Dornhffer and Colvin [12], 38 % of the patients had coronary artery disease, diabetes, cancer, or hypertension.
In the present study, the recurrence rate after 2 years was 19 % (46 of 243 participants). Epley [6] reported a recurrence rate of 30 % over a 30-month follow-up period. Furman demonstrated a yearly recurrence rate of 15 % after bedside treatment after a 4-year follow-up. Brandt [20] reported that the recurrence rate in BPPV patients after a mean follow-up of 10 years was 50 %. In most patients (80 %), recurrence occurred within the first year of the treatment, irrespective of the liberatory maneuver applied.
Fifteen of the 46 participants in the recurrence group (32.6 %) and 58 of the 197 participants in the no recurrence group (29.4 %) were older adults (>65 years). Pearson χ 2 test, Kaplan–Meier estimates, log-rank test, and Cox proportional hazards model revealed no significant difference between participants in the recurrence and nonrecurrence groups.
Among participants in the recurrence and nonrecurrence groups, 42 were females (91.3 %) and 154 were females (78.2 %), respectively. Pearson χ 2 test, Kaplan–Meier estimates, and log-rank test revealed significant differences between the groups, suggesting that females are more likely to be associated with the recurrence of BPPV. However, Cox proportional hazards model yielded no significant differences. In Nunez et al. [7] study, a recurrence rate of 26.8 % was observed among participants who initially reported resolution of symptoms after CRP; a Kaplan–Meier estimate showed an annual recurrence rate of 15 %, with a 50 % recurrence rate at 40 months after treatment. No significant association was noted between the recurrence rate and sex, age, duration of symptoms, presumed cause, or treating physician [7], an observation that differs from the results of the present study, where the recurrence rate was higher among females. In Sakaida et al. [13], overall recurrence rate was 37 % after 60 months of follow-up. The patients with horizontal canal BPPV exhibited a significantly higher recurrence rate (50 %, N = 19) at 60 months of follow-up than those with posterior canal BPPV (26 %, N = 28) did. No significant association between recurrence rates and sex or age was noted [13]. This observation was different from the result of the current study where the recurrence rate was higher among females.
Among the participants recurrence and nonrecurrence groups, 14 (30.4 %) and 26 (13.2 %) participants experienced sleep disorders, respectively. Pearson χ 2 test, Kaplan–Meier estimates, and log-rank test revealed a significant difference between the groups, suggesting that sleep disorders are likely associated with the recurrence of BPPV. However, Cox proportional hazards model showed no significant difference. Korres et al. [10] reported that in most (75.9 %) vertigo patients, BPPV was related to sleep disorders. BPPV is a common peripheral vestibular disorder, and Insomnia is often complained in out patient department. However, the relationship between insomnia and BPPV is not well investigated. Our study is the first to analyze the relationship between insomnia and recurrence after treatment with Epley’s maneuver in p-BPPV patients. In our clinical experience, we highly speculated bad sleep caused patients a lot of head movement during the night bed time and more prone to have otoconia free movement and BPPV relapse.
Among the participants recurrence and nonrecurrence groups, 8 (17.4 %) and 17 (8.6 %) participants had inner ear diseases, respectively. The associated inner ear diseases in our BPPV study patients were vestibular neuritis in majority and Menière disease minority. Pearson χ 2 test and Cox proportional hazards model showed no significant differences. However, Kaplan–Meier estimates and log-rank test revealed a significant difference. This is consistent with Dornhoffer and Colvin [12], who showed that inner ear diseases increase BPPV recurrence rate. Lee et al. [23] and Gross et al. [24] have noted that BPPV associated with inner ear diseases takes longer to recover it does BPPV of idiopathic nature. However, in a secondary subgroup in Lee et al., no significant difference was noted between Meniere disease related–BPPV and idiopathic BPPV. Gross [24] reported that vertigo in Meniere disease related BPPV took longer time for recovery than that in idiopathic BPPV did. Head trauma was observed in 2 of the 46 participants in the recurrence group (4.3 %) and in 9 of the 197 participants in the nonrecurrence group (4.6 %). Pearson χ 2 test, Kaplan–Meier estimates, log-rank test and Cox proportional hazards model showed no significant differences in recurrence rates. Cardiovascular diseases were observed in 20 (43.5 %) and 60 (30.5 %) participants in the recurrence and nonrecurrence groups, respectively. Pearson χ 2 test, Kaplan–Meier estimates, log-rank test, and Cox proportional hazards model showed no significant differences in the recurrence rates.
The limitation of the present study is that it focused on posterior semicircular canal BPPV and not on all types of BPPV. In addition, we could not distinguish between sleep disorders with a psychological disorder and those associated with a physical disease, such as nocturia or hypertension. We inquired about relapses only by telephone interview, so the diagnosis of relapse relies on a similar symptomatology, not on reexamination and we cannot be sure if the same ear relapsed or the other ear.
Conclusion
Epley’s maneuver (or CRP) is an effective, safe, and simple treatment for P-BPPV. Females and participants with sleep disorders and inner ear diseases are likely to be associated with the recurrence of P-BPPV after CRP. However, BPPV recurrence is not associated with age, head trauma, or cardiovascular diseases.
References
Dlugaiczyk J et al (2011) Involvement of the anterior semicircular canal in posttraumatic benign paroxysmal positioning vertigo. Otol Neurotol 32(8):1285–1290
Whitney SL, Marchetti GF, Morris LO (2005) Usefulness of the dizziness handicap inventory in the screening for benign paroxysmal positional vertigo. Otol Neurotol 26(5):1027–1033
Fife TD et al (2008) Practice parameter: therapies for benign paroxysmal positional vertigo (an evidence-based review): report of the quality standards subcommittee of the American academy of neurology. Neurology 70(22):2067–2074
Steenerson RL, Cronin GW, Marbach PM (2005) Effectiveness of treatment techniques in 923 cases of benign paroxysmal positional vertigo. Laryngoscope 115(2):226–231
Herdman SJ (1997) Advances in the treatment of vestibular disorders. Phys Ther 77(6):602–618
Furman JM, Cass SP (1999) Benign paroxysmal positional vertigo. N Engl J Med 341(21):1590–1596
Nunez RA, Cass SP, Furman JM (2000) Short- and long-term outcomes of canalith repositioning for benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg 122(5):647–652
Monobe H, Sugasawa K, Murofushi T (2001) The outcome of the canalith repositioning procedure for benign paroxysmal positional vertigo: are there any characteristic features of treatment failure cases? Acta Otolaryngol Suppl 545:38–40
Hamid M (2010) Medical management of common peripheral vestibular diseases. Curr Opin Otolaryngol Head Neck Surg 18(5):407–412
Korres SG et al (2007) Benign paroxysmal positional vertigo and its management. Med Sci Monit 13(6):CR275–CR282
Gordon CR et al (2004) Is posttraumatic benign paroxysmal positional vertigo different from the idiopathic form? Arch Neurol 61(10):1590–1593
Dornhoffer JL, Colvin GB (2000) Benign paroxysmal positional vertigo and canalith repositioning: clinical correlations. Am J Otol 21(2):230–233
Sakaida M et al (2003) Long-term outcome of benign paroxysmal positional vertigo. Neurology 60(9):1532–1534
Imai T et al (2005) Natural course of the remission of vertigo in patients with benign paroxysmal positional vertigo. Neurology 64(5):920–921
Lin HC et al (1999) The canalith repositioning procedure for benign paroxysmal positional vertigo. J Taiwan Otolaryngol Head Neck Surg 34(5):379–384
Levrat E et al (2003) Efficacy of the Semont maneuver in benign paroxysmal positional vertigo. Arch Otolaryngol Head Neck Surg 129(6):629–633
Seo T et al (2007) Immediate efficacy of the canalith repositioning procedure for the treatment of benign paroxysmal positional vertigo. Otol Neurotol 28(7):917–919
Radtke A et al (2004) Self-treatment of benign paroxysmal positional vertigo: Semont maneuver vs Epley procedure. Neurology 63(1):150–152
Oh HJ et al (2007) Predicting a successful treatment in posterior canal benign paroxysmal positional vertigo. Neurology 68(15):1219–1222
Brandt T et al (2006) Benign paroxysmal positioning vertigo: a long-term follow-up (6–17 years) of 125 patients. Acta Otolaryngol 126(2):160–163
Bhattacharyya N et al (2008) Clinical practice guideline: benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg 139(5 Suppl 4):S47–S81
Cohen HS, Kimball KT (2005) Effectiveness of treatments for benign paroxysmal positional vertigo of the posterior canal. Otol Neurotol 26(5):1034–1040
Lee NH et al (2010) Benign paroxysmal positional vertigo secondary to inner ear disease. Otolaryngol Head Neck Surg 143(3):413–417
Gross EM et al (2000) Intractable benign paroxysmal positional vertigo in patients with Meniere’s disease. Laryngoscope 110(4):655–659
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
All authors including Peijen Su, Yun-Chih Liu, Hung-Ching Lin, declare no conflict of interests. There is also no financial support for this study.
Ethical standard
The study was approved by the Mackay memorial hospital’s institutional review board (13MMHIS054) with chairman of Yen-Ta Lu M.D. PhD. All patients records/information were anonymized and de-identified prior to analysis.
Rights and permissions
About this article
Cite this article
Su, P., Liu, YC. & Lin, HC. Risk factors for the recurrence of post-semicircular canal benign paroxysmal positional vertigo after canalith repositioning. J Neurol 263, 45–51 (2016). https://doi.org/10.1007/s00415-015-7931-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-015-7931-0