Abstract
Adult polyglucosan body disease (APBD) is a rare glycogenosis manifesting progressive spastic paraparesis, sensorimotor polyneuropathy and neurogenic bladder. Misdiagnosis of APBD may lead to unnecessary investigations and to potentially harmful therapeutic interventions. To examine the frequency of misdiagnosis of APBD, we retrospectively reviewed the clinical data of 30 patients diagnosed between 1991 and 2013. Diagnosis was based on the combination of typical clinical and imaging findings, reduced glycogen branching enzyme activity, and the presence of p.Y326S GBE1 mutation. Initial symptoms started in the 5th–6th decade with bladder dysfunction (47 %), gait problems (33 %) or both. Diagnosis of APBD was delayed by 6.8 (±4.8) years. Consistent signs at diagnosis were spasticity in the legs (93 %), decreased or absent ankle reflexes (100 %), bilateral extensor plantar response (100 %) and distal sensory deficit (80 %). Nerve conduction study showed invariable sensorimotor polyneuropathy, and MRI demonstrated cervical spinal cord atrophy (100 %) and leukoencephalopathy (97 %). All 30 patients were initially misdiagnosed. Common misdiagnoses included cerebral small vessel disease (27 %), multiple sclerosis (17 %), amyotrophic lateral sclerosis (17 %) and peripheral neuropathies (20 %). Consequently, 27 % received inappropriate therapy. In addition, lower urinary tract symptoms in 60 % of men were attributed solely to prostatic disorders but did not respond to medical treatment or prostatectomy. These findings suggest that despite limited clinical variability, APBD is invariably misdiagnosed and patients are often mistreated. Physicians’ unfamiliarity with the typical clinical and imaging features of APBD appears as the main reason for misdiagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adult polyglucosan body disease (APBD) is an autosomal recessive glycogenosis due to glycogen branching enzyme (GBE) deficiency leading to the accumulation of polyglucosan bodies in the central (CNS) and peripheral (PNS) nervous system [1]. It typically presents in the 5th or 6th decade of age with the involvement of spinal cord and peripheral nerves [2, 3]. The most common clinical manifestation is progressive spastic paraparesis associated with sensorimotor axonal polyneuropathy and neurogenic bladder [2, 3]. Occasional reports describe hypokinetic rigid syndrome [4], fronto-temporal dementia [5], motor neuron disease [6], stroke-like episodes [7] or relapsing–remitting course and infrequent hepatopathy [8].
APBD is documented worldwide [3], but is apparently more frequent among patients of Ashkenazi Jewish background due to the presence of two founder mutations in the GBE1 gene [2, 9]. Although the disorder is considered rare, the estimated frequency of the common GBE1 mutation in this population is up to 1:35 [2, 10], raising the possibility of underdiagnosis. Therefore, we decided to examine the largest single cohort of APBD patients to determine how often the disease is misdiagnosed and whether this leads to inappropriate therapy.
Methods/patients
Retrospectively review of the clinical files of 23 Israeli APBD patients diagnosed between 1991 and 2010 [3], and of 7 new patients. Diagnosis was based on the combination of typical clinical and imaging findings, reduced GBE activity, routinely assayed in the peripheral blood leukocytes since 1991, and the presence of c.986A>C; p.Y326S GBE1 mutation in homozygosity (57 %) or in heterozygosity (43 %) with another mutation [2, 3]. Although initially sural nerve biopsy had been used for diagnosis, this practice was replaced by biochemical and molecular testing. Medical records were searched for all initial non-APBD diagnoses and for the time to correct diagnosis. An attempt was made to identify pitfalls leading to misdiagnosis. The treatment prescribed before diagnosis was classified as “appropriate” or “inappropriate” in relation to APBD.
Results
Clinical findings
Main demographic data and clinical findings in 30 patients with APBD are summarized in Table 1. Initial symptoms typically started in the 5th–6th decade of life. In 14 (47 %) patients, lower urinary tract symptoms preceded gait problems and in 5 of them by more than 5 years. In 10 (33 %) patients, weakness of the legs and spasticity preceded urinary symptoms, and in 2 of them by more than 5 years. Six patients had simultaneous onset of symptoms.
The median age at onset of gait disturbance was 55 years with a median interval to gait with a cane of 5 years, to a walker of 10 years and to a wheelchair of 13 years. No fluctuations, acute exacerbation of symptoms or hepatic dysfunction were reported or recorded.
Diagnosis of APBD was delayed by 6.8 (± 4.8) years, making up to 45 % (6.8/15.0) of the total disease duration from initial symptoms to death or last follow-up. Most consistent signs at diagnosis were spasticity in the legs (93 %), decreased or absent ankle reflexes (100 %), extensor plantar response (100 %) and distal sensory deficit in the legs (80 %). Of the 2 patients without spasticity in the legs at diagnosis, one was a 51-year-old woman with urinary incontinence of 2-year duration, peripheral neuropathy and bilateral extensor plantar response, whose brother had APBD, and the other was a 67-year-old woman with unsteady gait and recurrent falls of 2-year duration, symptomatic orthostatic hypotension, mild hypomimia and bradykinesia, peripheral neuropathy and bilateral extensor plantar response (Fig. 1).
Representative cerebral MRI findings in a 67-year-old woman with APBD misdiagnosed as MSA. Sagittal T1-weighted image (a) showing upper cervical spinal cord atrophy and incidental empty sella. Axial T2-weighted (b, d) and fluid-attenuated inversion recovery (c, e, f) images showing mild cerebral atrophy and extensive confluent and multifocal white matter hyperintensities specifically involving brainstem (b, c), posterior limb of the internal capsule (d, arrow), periventricular, lobar and subcortical white matter (c–f). Midbrain (c, arrow) and corpus callosum (e, arrow) linear pial hyperintensity is seen. Although involvement of the external capsule (d, dashed arrow) may look like “slit-like putaminal rim” in MSA [15], typical pontine “hot-cross bun” sign and middle cerebellar peduncle atrophy (b) are not seen
In addition, borderline to mild cognitive impairment was identified in 47 % of the patients using bedside (21/30) or formal (9/30) neurocognitive evaluation showing signs of frontal–subcortical impairment, and symptomatic orthostatic hypotension was documented in 5 of 12 patients with available data.
Initial spinal and/or cerebral MRI was performed 4.9 (±5.1) years before the diagnosis of APBD. Imaging abnormalities were remarkably similar (Fig. 1), including medullary and cervical spinal cord atrophy (100 %), cerebellar atrophy (57 %) and thinning of the corpus callosum (43 %). Cerebral subcortical and periventricular white matter lesions (97 %) were predominantly symmetrical, confluent or multifocal and were frequently associated with involvement of the posterior limb of internal capsule (93 %), and the brainstem (97 %). Cervical cord atrophy associated with significant spondylosis and parallel intramedullary T2 signal abnormality was identified in 1 patient. Lacunar infarcts were seen in 2 patients with comorbid cerebrovascular risk factors, but no microbleeds or areas of restricted diffusion were appreciated in the 10 studies obtained using appropriate acquisition sequences.
Nerve conduction study (NCS) showing a length-dependent, predominantly axonal sensorimotor peripheral neuropathy was performed 4.9 (±4.5) years before the diagnosis of APBD.
Results of auxiliary blood and CSF studies performed elsewhere were noncontributory, including normal CSF protein content in 15/18 (83 %) and negative oligoclonal bands in 18/18 (100 %) patients who had lumbar puncture.
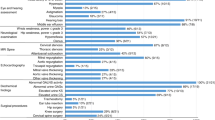
Misdiagnoses and inappropriate therapies
All 30 patients were misdiagnosed at the initial stages of their disease (Table 2). The incorrect diagnosis was made by neurologists, except in 9/15 men with early lower urinary tract symptoms attributed by their urologists solely to prostatic disorders, including benign prostatic hypertrophy (BPH) in 8/15 (53 %) men and cancer in 1. All 9 men had associated constipation, 6 had overflow fecal incontinence, and 8 complained of erectile dysfunction. Because all 9 men received medical treatment and 6/9 (73 %) had prostatectomy with no symptomatic improvement, we assume that these complaints could be attributed at least in part to APBD.
Most common neurological misdiagnoses were cerebral small vessel disease, multiple sclerosis (MS), amyotrophic lateral sclerosis (ALS) and various peripheral neuropathies. Consequently, 8/30 (27 %) patients received inappropriate therapy, including disease-modifying agents used for MS, immunosuppressive therapy for vasculitis or inflammatory neuropathy, and antiplatelet agents indicated for stroke. In addition, 1 of the 3 patients with presumed symptomatic cervical spondylotic myelopathy had major decompression surgery for the cervical and lumbar spinal degenerative changes without subsequent clinical improvement or stabilization.
Pitfalls in the diagnosis of APBD
Based on the limited available documentation from community physicians, we assume that failure to recognize or take into account the clinical and NCS signs of peripheral neuropathy in face of spastic paraparesis, or misattribute them to other conditions was the most common pitfall leading to misdiagnoses in 15/30 (50 %) patients. Consequently, this resulted in consideration of exclusively CNS diseases. Likewise, forms of peripheral neuropathy were diagnosed without explanation for spasticity and pyramidal signs in 6/30 (20 %) patients. A failure to suspect neurological cause for dominant urinary complaints associated with prostatic enlargement in 8/15 (53 %) men may have played a role in urological misdiagnosis.
Of the 14 available radiological or neurological interpretations of the initial cerebral MRI studies, 93 % misattributed imaging findings to other causes and only 1 (7 %) raised a possibility of APBD in the differential diagnosis.
Discussion
This is the first work to examine frequency, reasons and consequences of the misdiagnosis of APBD. We found that all our patients were misdiagnosed during initial stages of their disease, when presenting with dominant urinary symptoms (47 %), weakness of the legs and spasticity (33 %), or with both. Despite this relatively limited early clinical variability, correct diagnosis was delayed by an average of 6.8 years, which is 45 % of the total symptomatic disease duration.
At diagnosis, consistent neurological signs in 93 % of our patients represent a nearly invariable combination of pyramidal spastic paraparesis with peripheral neuropathy, characteristic of myeloneuropathy [11]. Although not all signs developed simultaneously and symptoms of the lower urinary tract dysfunction appeared late in 33 %, results of MRI and NCS suggestive of a mixed involvement of the CNS and the PNS preceded correct diagnosis by an average of 4.9 years. This likely implies physicians’ unfamiliarity with the typical clinical and imaging features of APBD as the main reason for its misdiagnosis.
Alternative neurological diagnoses before APBD include a wide range of relatively more common conditions (Table 2), such as cerebral small vessel disease in 27 %. Although it is a reasonable option for the specific age range of 5th–6th decade with possible comorbidity [12], and is occasionally suggested when stepwise episodes occur in APBD [7, 8], associated peripheral neuropathy and relentlessly progressive course in our patients without significant cognitive impairment argue against, as well as absent microbleeds or areas of restricted diffusion on MRI [12], infrequent lacunar infarcts and invariable spinal cord atrophy.
Another misdiagnosis is MS in 17 %. Given its worldwide occurrence and a 53.7/100,000 prevalence in Ashkenazi Jewish population [13], this may not be surprising. Furthermore, progressive spastic paraparesis with urinary incontinence and associated cerebral white matter lesions and spinal cord atrophy in APBD strongly mimics primary progressive MS and overlaps the age of onset [11]. The key features in our patients to distinguish the two conditions are invariable peripheral neuropathy, absent focal T2 spinal cord lesions and negative CSF oligoclonal bands [14]. It is likely that adherence to the accepted MS criteria and exclusion of possible imitators [14] would have prevented misdiagnosis and potentially harmful therapies. Likewise, application of the available diagnostic criteria for ALS, CIDP and multiple system atrophy (MSA) would probably yield earlier correct diagnosis in 30 % of our patients. Whereas clinical and NCS findings of sensorimotor peripheral neuropathy, bladder dysfunction, absent fasciculations and MRI abnormalities rule out ALS, symptomatic orthostatic hypotension in 5 of our patients and mild early motor manifestations in 2 of them may suggest a cerebellar variant of MSA [15]. However, their MRI findings (Fig. 1), peripheral neuropathy and progressive spastic paraparesis are non-supporting of this diagnosis [15].
Of the other neurological misdiagnoses (Table 2), cervical spondylotic myelopathy in 10 % deserves additional mention because of an option for therapeutic surgical decompression. It is the commonest cause of nontraumatic myelopathy and occurs in a similar age group as APBD [16]. Although both may coexist, as in one of our patients, spondylotic myelopathy typically presents with numbness, paresthesias and cervical pain of subacute onset [16], often with radicular and asymmetric involvement of the arms, all undocumented in our patients. In addition, associated cerebral white matter lesions in 97 % in this cohort represent important red flag to prefer other etiology [16].
Familial occurrence in 27 % of our patients, slowly progressive course with symmetric neurological manifestations, and imaging and nerve conduction findings may have contributed to suspect forms of leukodystrophy, hereditary spastic paraplegia and hereditary peripheral neuropathy in 17 %. However, their relatively late age, predominant Ashkenazi Jewish origin, characteristic myeloneuropathy [11] and the specific pattern of cerebral MRI abnormalities [3] are practically pathognomonic for APBD.
Important non-neurological misdiagnosis is BPH in 8/15 (53 %) men. Having estimated prevalence of 50 % among men in their sixties [17], it is probable that BPH coexisted with APBD in some of our patients. However, because 5/8 men had prostatectomy with no long-term symptomatic improvement, we assume that this condition was not solely responsible for their lower urinary tract dysfunction and that their complaints could be attributed at least in part to APBD. Associated erectile dysfunction, constipation, often with overflow fecal incontinence, and neurological symptoms are not explained by BPH and should prompt workup for non-urological etiology.
Review of the isolated descriptions of misdiagnosed APBD patients from different ethnic backgrounds reveals that our findings are shared by others [3, 7, 8, 11]. APBD is apparently underdiagnosed and, as shown by us, is often misdiagnosed. Taken together, our findings support the importance to improve physicians’ awareness of the clinical and imaging features of APBD and to suspect this disease particularly in adults with lower urinary tract symptoms and gait difficulties accompanied by suggestive NCS and MRI findings. Early correct diagnosis could reduce costly investigations, eliminate potentially harmful non-indicated therapeutic interventions, enable appropriate counseling, and form the basis for clinical trials.
References
Robitaille Y, Carpenter S, Karpati G, DiMauro SD (1980) A distinct form of adult polyglucosan body disease with massive involvement of central and peripheral neuronal processes and astrocytes: a report of four cases and a review of the occurrence of polyglucosan bodies in other conditions such as Lafora’s disease and normal ageing. Brain 103:315–336
Lossos A, Meiner Z, Barash V et al (1998) Adult polyglucosan body disease in Ashkenazi Jewish patients carrying the Tyr329Ser mutation in the glycogen branching enzyme gene. Ann Neurol 44:867–872
Mochel F, Schiffmann R, Steenweg ME et al (2012) Adult polyglucosan body disease: natural history and key magnetic resonance imaging findings. Ann Neurol 72:433–441
Krim E, Vital A, Macia F, Yekhlef F, Tison F (2005) Atypical parkinsonism combining alpha-synuclein inclusions and polyglucosan body disease. Mov Disord 20:200–204
Boulan-Predseil P, Vital A, Brochet B, Darriet D, Henry P, Vital C (1995) Dementia of frontal lobe type due to adult polyglucosan body disease. J Neurol 242:512–516
McDonald TD, Faust PL, Bruno C, DiMauro S, Goldman JE (1993) Polyglucosan body disease simulating amyotrophic lateral sclerosis. Neurology 43:785–790
Billot S, Herve D, Akman HO et al (2013) Acute but transient deterioration revealing adult polyglucosan body disease. J Neurol Sci 324:179–182
Paradas C, Akman HO, Ionete C et al (2014) Branching enzyme deficient. Expanding the clinical spectrum. JAMA Neurol 71:41–47
Akman HO, Kakhlon O, Coku J et al (2014) Deep intronic GBE1 mutation in manifesting heterozygous patients with adult polyglucosan body disease. JAMA Naurol 72:441–445
Hussain A, Armistead J, Gushulak L et al (2012) The adult polyglucosan body disease mutation GBE1 c.1076A>C occurs at high frequency in persons of Ashkenazi Jewish background. Biochem Biophys Res Commun 426:286–288
Lossos A, Klein CJ, McEvoy KM, Keegan BM (2009) A 63-year-old woman with urinary incontinence and progressive gait disorder. Neurology 72:1607–1613
Pantoni L (2010) Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol 9:689–701
Alter M, Kahana E, Zilber N, Miller A (2006) Multiple sclerosis frequency in Israel’s diverse populations. Neurology 66:1061–1066
Rice CM, Cottrell D, Wilkins A, Scolding NJ (2013) Primary progressive multiple sclerosis: progress and challenges. J Neurol Neurosurg Psychiatry 84:1100–1106
Kim H-J, Jeon BS, Jellinger KA (2015) Diagnosis and differential diagnosis of MSA: boundary issues. J Neurol. doi:10.1007/s00415-015-7654-2
Flanagan EP, Krecke KN, Marsh RW et al (2014) Specific pattern of gadolinium enhancement in spondylotic myelopathy. Ann Neurol 76:54–65
Lepor H (2004) Pathophysiology, epidemiology, and natural history of benign prostatic hyperplasia. Rev Urol 6(S9):3–10
Acknowledgments
Dr. Kakhlon is supported in part by the Adult Polyglucosan Body Disease Research Foundation research grant for studies in APBD and in part by the AFM (Association Française contre les Myopathies)-Telethon Grant for studies in neuropolyglucosanoses. Dr. Giladi incumbents the Sieratzki Chair in Neurology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors report no conflicts of interest. Funders of Dr. Kakhlon’s research had no role in the design and conduct of the study, collection and interpretation of the data, and preparation or approval of the manuscript.
Ethical standard
The study was approved by the Hadassah-Hebrew University Medical Center Institutional Review Board, and patients gave their informed consent prior to their inclusion in the study.
Rights and permissions
About this article
Cite this article
Hellmann, M.A., Kakhlon, O., Landau, E.H. et al. Frequent misdiagnosis of adult polyglucosan body disease. J Neurol 262, 2346–2351 (2015). https://doi.org/10.1007/s00415-015-7859-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-015-7859-4