Abstract
It has been suggested that corticomotoneuronal drive to ankle dorsiflexors is greater than to ankle plantar flexor muscles, despite the finding that plantar flexors are no less active than TA during walking and standing. The present study was undertaken to determine whether there was differential involvement of distal lower limb muscles in amyotrophic lateral sclerosis (ALS), to elucidate pathophysiological mechanisms of selective muscle involvement. Prospective studies were undertaken in 52 ALS patients, including clinical assessment, disease staging (revised ALS functional rating scale), Medical Research Council sum score, and a scale of upper motor neurone (UMN) dysfunction. Motor unit number estimates (MUNE) and compound muscle action potentials (CMAP) from ankle dorsiflexors and plantar flexors were used to provide objective measures. A novel ‘split leg index’ was calculated as follows: SLI = CMAPDF ÷ CMAPPF. In ALS, there was significantly greater reduction of MUNE and CMAP amplitude recorded from plantar flexors when compared to dorsiflexors, suggesting preferential involvement of plantar flexor muscles, underpinning a ‘split leg’ appearance. The SLI correlated with clinical plantar flexor strength (R= −0.56, p < 0.001). In no patient did the SLI suggest preferential dorsiflexor involvement. In subgroup analyses, mean SLI was greatest in lower limb-onset ALS. In conclusion, the present study has established dissociated involvement of muscles acting around the ankle in ALS. We suggest this reflects underlying differences in cortical, descending or local spinal modulation of these muscles.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The onset of amyotrophic lateral sclerosis (ALS) is typically focal, with muscle weakness becoming more widespread with disease progression [1]. The pattern of disease involvement and subsequent progression in ALS delineate the underlying process of neurodegeneration [1–3]. One such feature, the ALS split hand, is a distinctive clinical and neurophysiological phenomenon in ALS, characterised by dissociated wasting of the thenar muscles and first dorsal interosseous when compared with the hypothenar muscles [4, 5].
The nature of lower limb functional activities, predominantly walking and standing, differs from the fine-fractionated movements seen in upper limb tasks. There is a discrepancy in the density of corticospinal projections to the anterior horn cells innervating the leg muscles, such that soleus, an ankle plantar flexor receives only 10–30 % as many direct corticospinal projections as tibialis anterior (TA), the main ankle dorsiflexor [6].
The pattern of lower limb involvement in ALS differs from that in other body regions. Clinically, involvement of the lower limbs may be relatively symmetrical earlier in the course of disease [2, 7] and lower limb-onset ALS spreads to the contralateral lower limb more frequently than to the upper limbs [8]. However, specific patterns of lower limb muscle involvement in ALS remain to be elucidated. Previously described patterns of muscle weakness, such as ‘pyramidal weakness’ following upper motor neurone injury, may not apply in ALS [9] because there is concurrent destruction of propriospinal and corticospinal motor pathways, and also of the motoneuronal and interneuronal network at segmental cord level in the anterior horns, causing a combination of UMN and LMN dysfunction. Our study was undertaken to analyse the pattern of relative involvement of ankle dorsiflexor and plantar flexor muscles, to study the pathophysiology of selective muscle involvement in ALS.
Patients and methods
Clinical and neurophysiological data were acquired prospectively from 52 consecutive ALS patients (mean age 57.5 ± 1.6). Patients were included in the study if they were classified as suffering clinically probable or definite ALS according to the Awaji-Shima criteria [10]. Clinically detectable lower limb muscle involvement was not a prerequisite for inclusion. All patients provided written informed consent and the study was approved by the South East Sydney Area Health Service Human Research Ethics Committee.
Clinical measures
Standardised clinical assessments were recorded for each patient before neurophysiological evaluation. Motor functional status was assessed using the revised ALS Functional Rating Scale (ALSFRS-R) [11]. The region of clinical onset and symptomatic body regions at the time of clinical review were determined. Hand dominance was recorded.
Muscle strength was assessed using the standard Medical Research Council (MRC) rating scale [12]. Ankle dorsiflexion and plantar flexion (tested with the knee flexed) was graded for each patient.
Upper motor neuron (UMN) signs in the lower limb were assessed using a score developed to assess clinical UMN dysfunction in patients with ALS [13]. Knee and ankle reflexes were individually scored on a two-point scale with a score of one given for a hyperactive reflex without spread or a preserved reflex in a wasted muscle, and a score of two for a reflex with evidence of pathological spread. A score of one point each was given for the presence of the Babinski response and ankle clonus (>4 beats) for a maximal score of six per lower limb.
A lower limb was considered to be unaffected (1) if the patient did not report specific symptoms related to lower limb function, (2) if there were no points lost on lower limb tasks of the ALSFRS-R (items 8 and 9), (3) if there were no significant neurological abnormalities detected on lower limb clinical examination and (4) if EMG studies of the lower limb did not identify evidence of neurogenic motor unit rearrangement, fibrillations or fasciculations. Conversely, a limb was defined as affected if any of these criteria were met.
Neurophysiological studies
The ankle dorsiflexor (DF) compound muscle action potential (CMAP) was elicited by stimulating the common peroneal nerve at the fibular head and recording with the active (G1) electrode placed one-third of the way along a line joining the tibial tuberosity and the ankle joint, and 2 cm lateral to the anterior tibial crest, and the reference electrode (G2) placed over the TA tendon at the ankle. Ankle plantar flexor (PF) CMAP amplitudes were obtained from the same limb after stimulation of the tibial nerve in the popliteal fossa, recording from the active electrode (G1) placed in the midline of the calf at a point immediately inferior to the distal margin of the gastrocnemius. The reference electrode (G2) was placed over the Achilles tendon at the ankle [14]. Stimulus intensity was increased (up to 100 mA) with a pulse width of 1 ms so that supramaximal responses were obtained. The amplitude of the resulting CMAP was recorded from baseline to negative peak, in accordance with standard conventions. In the case of bipeaked dorsiflexor CMAPs, the amplitude was measured to the tallest peak. The split leg index (SLI) was calculated using the following formula:
Motor unit number estimation (MUNE) studies, were performed on ankle dorsiflexor and plantar flexor muscles using the electrode positions described above. MUNE was performed on both lower limbs of ALS patients, and one lower limb of control subjects. A software modification supplied by Nicolet Biomedical (Madison, WI) was used to collect stimulus–response curves, by automatically evoked incremental stimuli commencing at the minimal intensity necessary to elicit a single unit motor response and terminating at intensity 10–20 % higher than the stimulus required to elicit the maximal CMAP response [15]. Stimulation frequency was 2 Hz. Stimulation duration was 0.2 ms for the peroneal nerve and 1 ms for the tibial nerve. 500 stimuli were delivered to patients and 1000 stimuli to control subjects. CMAP amplitude measurements were automatically calculated from baseline to negative peak. To account for differences in CMAP morphology, CMAP area and duration were measured from onset to baseline crossing. Bayesian MUNE analysis was applied to the CMAP area stimulus–response curves, as previously published [16, 17].
Needle EMG studies were performed on lower limb muscles, including medial gastrocnemius and tibialis anterior, to identify neurogenic changes indicating disease involvement.
These neurophysiological studies in ALS patients were compared with values obtained from 22 age-matched healthy controls (mean age 55.5 ± 2.9 years).
Reliability of the test procedure
Separate studies to address test–retest reliability were performed in five healthy control subjects to exclude variation of CMAP amplitudes due to discrepancies in nerve stimulation and electrode placement. Supramaximal CMAP amplitudes were recorded as described above from five separate sessions. Electrodes were removed in between sessions, as were any marks. Reliability of the test procedure was confirmed by calculating intraclass correlation coefficients (ICCs) for both dorsiflexor CMAP amplitude (CMAPDF ICC = 0.997) and plantar flexor CMAP amplitude (CMAPPF ICC = 0.974).
Statistical analysis
All values were expressed as mean ± standard error of the mean (SEM). One-way ANOVA was performed to evaluate differences between groups. Spearman ρ correlations were used to assess the relationship between variables. The Bonferroni correction for multiple comparisons was applied to minimise the risk of chance findings.
Results
In the 52 ALS patients, disease onset was bulbar in 21 %, upper limb in 47 %, and lower limb in 32 % (Table 1). The mean disease duration from symptom onset was 23.5 ± 2.7 months (range 4–72 months). The mean ALSFRS-R score was 41.0 ± 0.6 suggesting a mild-to-moderate degree of disability. There was no significant difference in the ALSFRS-R scores between ALS patients with lower limb dysfunction and those in whom lower limb function was normal.
In the 52 patients, 73 % of lower limbs were classified as affected, and 26 % as unaffected. In 2 patients one lower limb was affected and one was unaffected. In affected lower limbs, median MRC score was 4/5 for dorsiflexion and 5/5 for plantar flexion. In affected limbs, dorsiflexion strength was normal (5/5) in 26 % of limbs, and plantar flexion strength was normal in 41 % of limbs.
In terms of clinically detectable weakness, dorsiflexion and plantar flexion strength were graded as equal on the MRC rating scale in 59 % of limbs, with normal strength for both muscles in 51 % (Fig. 1). Ankle dorsiflexion was weaker than plantar flexion in 31 % of limbs. In 46 % of these limbs, there was normal plantar flexion strength. Plantar flexion was weaker than dorsiflexion in 18 % of limbs (14 % with normal dorsiflexion strength; Fisher exact test, p = 0.27). The ratio of ankle dorsiflexion to ankle plantar flexion MRC scores was 1.0 (range 0.5–2.0) although it is noted that MRC scores are not linear and ankle plantar flexors are 5–10 fold stronger than dorsiflexors [18]. Hence the strength of these muscle groups may not be directly comparable. UMN signs were apparent in 69 % of ALS lower limbs.
Neurophysiological characteristics
There was a significant reduction in the CMAP amplitudes recorded from both the dorsiflexor (p < 0.001) and plantar flexor muscles (p < 0.001) in the affected limbs of ALS patients when compared to controls (Table 2; Fig. 2). The CMAP amplitudes from the unaffected lower limbs in the ALS group were not significantly different from control values.
Dorsiflexor and plantar flexor compound muscle action potential amplitudes. Mean compound muscle action potential (CMAP) amplitudes recorded from dorsiflexor and plantar flexor muscle groups in ALS patients (affected limbs black bars, unaffected limbs light grey bars and control subjects white bars). * p < 0.05, *** p < 0.0001
When the cohort was divided into region of onset, the mean CMAPPF amplitude was lower in the bulbar and lower limb-onset ALS cohorts when compared to controls (Table 2), although the reduction was only significant for the lower limb-onset group (p < 0.001). In addition, the CMAPPF amplitude was significantly reduced in the lower limb-onset patients when compared with upper limb-onset (p < 0.001) and bulbar-onset ALS patients (p = 0.05). CMAPDF amplitude was significantly reduced in the lower limb-onset group when compared with control values (p < 0.001), bulbar-onset (p = 0.002) and upper limb-onset (p < 0.001) groups.
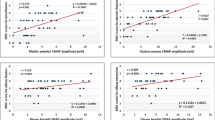
There were significant correlations between the CMAPPF amplitude and ankle plantar flexion strength (r = 0.71, p < 0.001) and the CMAPDF amplitude and ankle dorsiflexion strength (r = 0.71, p < 0.001) confirming that the finding of reduced CMAP amplitude was clinically relevant.
There was a significant increase in the mean SLI in the ALS cohort when compared to controls (p = 0.001, Table 2; Fig. 3), suggesting dissociated involvement of lower limb muscles with greater reduction of CMAPPF amplitude, which we termed the ‘split leg’ phenomenon. This increase in SLI occurred in patients with affected lower limbs. In contrast, the mean SLI in unaffected ALS lower limbs was similar to control limbs, and significantly lower when compared to affected ALS lower limbs (Table 2; Fig. 3, p = 0.001). Further, the SLI was significantly increased in limbs with plantar flexor weakness (SLI = 1.44 ± 0.22) compared with those patients without plantar flexion weakness (SLI = 0.76 ± 0.08; p < 0.001). Patients with lower limb-onset disease had a higher SLI than patients with disease onset in other regions, which was significant when compared with the upper limb-onset group (p < 0.01) and controls (p < 0.001).
Correlations between the SLI and clinical variables were performed. The SLI correlated significantly with plantar flexion strength (r = −0.53, p < 0.001) but not dorsiflexion strength (r = −0.14, p = 0.53). There was no correlation between the UMN scores from affected ALS limbs and the SLI (Spearman’s ρ = −0.09).
MUNE studies were undertaken in the lower limbs in 10 ALS patients (mean age 61.5 ± 3.3 years) with each lower limb classified as affected, and results were compared to age-matched controls (mean age 56.3 ± 5.3 years, p = 0.44). All lower limbs studied with MUNE were classified as affected. In ALS patients, there was a significant reduction of MUNE in the dorsiflexor (p < 0.001) and plantar flexor (p = 0.001) muscle groups (Fig. 4; Table 2). The mean ratio of MUNEDF to MUNEPF was increased in the ALS group (p = 0.03). When compared with SLI values, in the 10 limbs with increased SLI values, MUNEDF:MUNEPF was always greater than 1, thus supporting the notion of dissociated neuronal loss in the lower limbs, with preferential involvement of motor neurons innervating the plantar flexor muscles.
Motor unit number estimates (MUNE) in ALS and control subjects. Illustrative examples of MUNE in a patient with ALS (a). Estimated dorsiflexor motor unit number was 24, and plantar flexor motor unit number was 15. This compares with the SLI in this patient which was 2.2. The relationship between dorsiflexor and plantar flexor MUNE values in control and ALS patients is demonstrated (b). ALS patients black bars, control subjects white bars. ** p = 0.001, *** p < 0.001
Subgroup analysis
The SLI was increased (defined as >control mean plus 2 standard deviations) in 49 % of all ALS lower limbs, including 65 % of affected lower limbs and 9 % of unaffected lower limbs. When the region of onset was considered, the SLI was increased in 67 % of lower limbs from patients with bulbar-onset disease, 33 % with UL-onset and 61 % with LL-onset. In no patient did the SLI fall below control values; i.e., in none was there greater involvement of the CMAPDF than the CMAPPF, including in those patients who appeared to have greater weakness of ankle dorsiflexion than plantar flexion.
The ALS cohort was divided into patients with early disease (≤12 months, 37 % of the cohort) and later disease (>12 months, 63 % of the cohort). The SLI was increased in the shorter disease duration group relative to control subjects (SLI = 0.72 ± 0.09, p = 0.004). SLI was significantly higher in the longer disease duration group relative to the shorter duration group (SLI = 1.18 ± 0.14, p = 0.01). In the longer disease duration group, there was a commensurate increase in the proportion of lower limbs with greater plantar flexion weakness than dorsiflexion weakness, and fewer limbs with greater dorsiflexion weakness (Table 1). These findings suggest that preferential loss of axons innervating plantar flexor muscles increases with disease progression.
Further analysis identified that SLI values were similar between the dominant and non-dominant sides (dominant SLI = 0.94 ± 0.14, non-dominant SLI = 1.05 ± 0.16). In terms of side-to-side differences, 74 % of leg pairs demonstrated similar SLI values between the right and left side (43 % bilaterally increased, 31 % bilaterally normal). In the remaining 26 % of leg pairs, SLI values were asymmetric, with a normal SLI in one leg and increased SLI in the other. Clinical weakness was asymmetric in 47 % of these patients.
Of those limbs with normal SLI, 48 % were from unaffected limbs. In affected limbs with normal SLI, 20 % demonstrated normal strength and CMAP amplitudes, and the remainder demonstrated reduced CMAP amplitudes (mean CMAPPF = 4.7 ± 0.5 mV; mean CMAPDF = 2.1 ± 0.2 mV) and greater weakness of dorsiflexion (median MRC score = 3) than plantar flexion (median MRC score = 4.5). UMN signs were present in 76 % of affected limbs with a normal SLI, (mean 2.0 out of 6 on the UMN score), versus 74 % of affected limbs with an increased SLI.
Discussion
The present study has identified dissociated involvement of distal lower limb muscles in patients with ALS. Specifically, a ‘split leg’ pattern has been established with preferential reduction of motor neurons innervating the plantar flexor muscles, as indicated by significant reduction of motor amplitudes and motor unit numbers. Identification of dissociated lower limb muscle involvement may suggest disparities in lower limb muscle activation during physical activity, differences in cortical modulation of corticomotoneurones innervating lower limb muscles, or variation in descending motor control tracts such as reticulospinal inputs.
Our finding of preferential involvement of soleus may at first seems unexpected given that patients with ALS commonly report foot drop as a symptom [19], and foot drop may be a prominent feature of corticospinal tract injury [20]. However, dorsiflexion weakness tends to be more obvious to patients than weakness of plantar flexion [21], and this may be partly related to the anti-gravity nature of ankle dorsiflexion. In addition, plantar flexion weakness may be underestimated by clinicians, because of difficulties in detecting plantar flexion strength with standard manual muscle testing [22].
Previous epidemiological studies have suggested a link between vigorous exercise and the development of ALS [23]. Lower limb activity in humans generally involves tonic activation of the glutei, vasti and plantar flexor muscles while standing [24] and alternating activation of ankle dorsiflexors and plantar flexors during gait [25], but with more prolonged activation of plantar flexors during the gait cycle. As such, the relatively greater contribution of soleus to walking and standing may further predispose the axons supplying soleus to neurodegenerative processes.
Our findings may also be considered in light of the ALS split hand phenomenon [26]. In the split hand there is greater disease involvement of thenar muscles and first dorsal interosseous, than of the hypothenar muscles [5]. The origin of the split hand pattern is debated with two predominant hypotheses. A primary corticomotoneuronal influence on the development of the ALS split hand [27] is supported by transcranial magnetic stimulation studies, which have suggested that the corticospinal input to the thenar muscles is preferentially involved in ALS, and that this preferential involvement relates to the density of corticospinal projections to thenar muscles [28]. However, in humans, physical activity involving the thenar muscles is greater than the hypothenar muscles and, conceivably, this may result in greater oxidative stress in axons innervating thenar muscles, resulting in preferential degeneration at a spinal or peripheral level. A split hand pattern in normal ageing [29], and differences in axonal excitability of nerves innervating thenar and hypothenar muscles suggest differential susceptibility to degeneration [30].
In the present study, there was greater involvement of ankle plantar flexor than dorsiflexor muscles, which receive greater direct corticospinal excitation [6]. Data in macaque models have suggested more inhibitory cortical modulation of plantar flexors compared with more excitatory modulation of TA [31]. Human data on the cortical control of plantar flexor and dorsiflexor motoneurone pools is more limited, largely based on the monosynaptic excitation produced by rapidly conducting axons excited by transcranial stimulation (which comprise <5 % of corticospinal axons). Facilitatory influences on TA are consistently identified [6, 32], while the cortical effects on plantar flexor motoneurons may be dependent on posture [33]. Thus a discrepancy between the density and nature of the cortical motoneuronal projections to plantar flexor and dorsiflexor muscles may be an additional contribution to the pathogenesis of the split leg pattern. However, the absence of a correlation between the SLI and clinical UMN signs may suggest independence of LMN and UMN pathology.
Discrepancies in the nature of cortical modulation are evident with other muscle pairs in ALS. There is lesser clinical involvement of flexor pollicis longus (FPL) than APB in ALS [34], and transcranial magnetic stimulation studies have identified greater cortical inhibition of APB than FPL motor output in healthy subjects [35], and relatively greater reduction of cortical inhibition in APB than FPL in ALS [36]. This is similar to the findings in hand muscles, with greater cortical inhibitory modulation of APB and FDI in healthy subjects [37], and greater reduction of cortical inhibitory modulation of APB and FDI in ALS [38]. As such, the nature of cortical modulation of individual muscle output, rather than the extent of direct corticospinal tract drive may be more relevant in ALS pathogenesis, with loss of the normal inhibitory cortical influence associated with greater muscle involvement. This hypothesis links with studies highlighting the pathogenic contribution of altered inhibitory interneuronal function in ALS [39].
Finally, descending internuncial connexions in the spinal cord may also contribute to the phenomenon [40]. There is evidence of dysfunction of segmental motoneurones projecting to soleus, related to the extent of UMN dysfunction, suggesting modulation of segmental motoneuronal function by descending inputs [13]. Following UMN injury, the lower limb is typically held in extension with predominant plantar flexion at the ankle, with this phenomenon mediated by damage to descending fibres originating in the pons [41]. These descending pathways include the reticulospinal tract, which projects predominantly onto extensor muscles in the lower limb [42]. Of interest, there are also substantial excitatory reticulospinal projections to intrinsic hand muscles, which are markedly augmented following injury to the corticospinal tract [43]. Dysequilibrium of excitatory inputs onto specific muscles following corticomotoneuronal injury may be an additional consideration to explain the patterns of muscle involvement seen in ALS.
References
Ravits JM, La Spada AR (2009) ALS motor phenotype heterogeneity, focality, and spread: deconstructing motor neuron degeneration. Neurology 73(10):805–811
Simon NG, Lomen-Hoerth C, Kiernan MC (2014) Patterns of clinical and electrodiagnostic abnormalities in early amyotrophic lateral sclerosis. Muscle Nerve. doi:10.1002/mus.24244
Devine MS, Kiernan MC, Heggie S, McCombe PA, Henderson RD (2014) Study of motor asymmetry in ALS indicates an effect of limb dominance on onset and spread of weakness, and an important role for upper motor neurons. Amyotroph Lateral Scler Frontotemporal Degen. doi:10.3109/21678421.2014.906617
Wilbourn AJ (2000) The split hand syndrome. Muscle Nerve 23:138
Kuwabara S, Mizobuchi K, Ogawara K, Hattori T (1999) Dissociated small hand muscle involvement in amyotrophic lateral sclerosis detected by motor unit number estimates. Muscle Nerve 22(7):870–873
Brouwer B, Ashby P (1992) Corticospinal projections to lower limb motoneurons in man. Exp Brain Res 89(3):649–654
Ravits J, Paul P, Jorg C (2007) Focality of upper and lower motor neuron degeneration at the clinical onset of ALS. Neurology 68(19):1571–1575
Turner MR, Brockington A, Scaber J, Hollinger H, Marsden R, Shaw PJ et al (2010) Pattern of spread and prognosis in lower limb-onset ALS. Amyotroph Lateral Scler. 11(4):369–373
Brooks BR (1996) Natural history of ALS: symptoms, strength, pulmonary function, and disability. Neurology 47(4 Suppl 2):S71–S81
de Carvalho M, Dengler R, Eisen A, England JD, Kaji R, Kimura J et al (2008) Electrodiagnostic criteria for diagnosis of ALS. Clin Neurophysiol 119(3):497–503
Cedarbaum JM, Stambler N, Malta E, Fuller C, Hilt D, Thurmond B et al (1999) The ALSFRS-R: a revised ALS functional rating scale that incorporates assessments of respiratory function. BDNF ALS Study Group (Phase III). J Neurol Sci 169(1–2):13–21
Medical Research Council (1976) Aid to the examination of the peripheral nervous system. Her Majesty’s Stationary Office, London
Simon NG, Lin CS-Y, Lee M, Howells J, Vucic S, Burke D et al (2014) Segmental motoneuronal dysfunction is a feature of amyotrophic lateral sclerosis. Clin Neurophysiol. doi:10.1016/j.clinph.2014.07.029
Lin CS, Chan JH, Pierrot-Deseilligny E, Burke D (2002) Excitability of human muscle afferents studied using threshold tracking of the H reflex. J Physiol 545(Pt 2):661–669
Blok JH, Ruitenberg A, Maathuis EM, Visser GH (2007) The electrophysiological muscle scan. Muscle Nerve 36(4):436–446
Ridall PG, Pettitt AN, Henderson RD, McCombe PA (2006) Motor unit number estimation—a Bayesian approach. Biometrics 62(4):1235–1250
Henderson RD, Ridall PG, Hutchinson NM, Pettitt AN, McCombe PA (2007) Bayesian statistical MUNE method. Muscle Nerve 36(2):206–213
Morse CI, Tolfrey K, Thom JM, Vassilopoulos V, Maganaris CN, Narici MV (2008) Gastrocnemius muscle specific force in boys and men. J Appl Physiol (1985) 104(2):469–474
Mitchell JD, Borasio GD (2007) Amyotrophic lateral sclerosis. Lancet 369:2031–2041
Twitchell TE (1951) The restoration of motor function following hemiplegia in man. Brain 74(4):443–480
Stewart JD (2008) Foot drop: where, why and what to do? Pract Neurol 8:158–169
Lunsford BR, Perry J (1995) The standing heel-rise test for ankle plantar flexion: criterion for nornal. Phys Ther 75:694–698
Scarmeas N, Shih T, Stern Y, Ottman R, Rowland LP (2002) Premorbid weight, body mass, and varsity athletics in ALS. Neurology 59:773–775
Liu MQ, Anderson FC, Pandy MG, Delp SL (2006) Muscles that support the body also modulate forward progression during walking. J Biomech 39(14):2623–2630
Courtine G, Papaxanthis C, Schiepatti M (2006) Coordinated modulation of locomotor muscle synergies constructs straight ahead and curvilinear walking in humans. Exp Brain Res 170:320–335
Eisen A, Kuwabara S (2012) The split hand syndrome in amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry 83(4):399–403
Eisen A, Kim S, Pant B (1992) Amyotrophic lateral sclerosis (ALS): a phylogenetic disease of the corticomotoneuron? Muscle Nerve 15:219–224
Weber M, Eisen A, Stewart H, Hirota N (2000) The split hand in ALS has a cortical basis. J Neurol Sci 180:66–70
Voermans NC, Schelhaas HJ, Munneke M, Zwarts MJ (2006) Dissociated small hand muscle atrophy in aging: the ‘senile hand’ is a split hand. Eur J Neurol 13:1381–1384
Bae JS, Sawai S, Misawa S, Kanai K, Isose S, Kuwabara S (2009) Differences in excitability properties of FDI and ADM motor axons. Muscle Nerve 39(3):350–354
Hudson HM, Griffin DM, Belhaj-Saif A, Cheney PD (2013) Cortical output to fast and slow muscles of the ankle in the rhesus macaque. Front Neural Circuit 7:33
Brouwer B, Ashby P (1990) Corticospinal projections to upper and lower limb spinal motoneurons in man. Electroencephalogr Clin Neurol. 76(6):509–519
Valls-Sole J, Alvarez R, Tolosa ES (1994) Responses of the soleus muscle to transcranial magnetic stimulation. Electroencephalogr Clin Neurol 93(6):421–427
Menon P, Bae JS, Mioshi E, Kiernan MC, Vucic S (2013) Split-hand plus sign in ALS: differential involvement of the flexor pollicis longus and intrinsic hand muscles. Amyotroph Lateral Scler Frontotemporal Degen 14(4):315–318
Bae JS, Menon P, Mioshi E, Kiernan MC, Vucic S (2013) Cortical excitability differences between flexor pollicis longus and APB. Neurosci Lett 29(541):150–154
Bae JS, Menon P, Mioshi E, Kiernan MC, Vucic S (2014) Cortical hyperexcitability and the split-hand plus phenomenon: pathophysiological insights in ALS. Amyotroph Lateral Scler Frontotemporal Degen 15(3–4):250–256
Menon P, Kiernan MC, Vucic S (2014) Cortical excitability differences in hand muscles follow a split-hand pattern in healthy controls. Muscle Nerve 49(6):836–844
Menon P, Kiernan MC, Vucic S (2014) Cortical dysfunction underlies the development of the split-hand in amyotrophic lateral sclerosis. PLoS One 9(1):e87124
Turner MR, Kiernan MC (2012) Does interneuronal dysfunction contribute to neurodegeneration in amyotrophic lateral sclerosis? Amyotroph Lateral Scler 13(3):245–250
Swash M (2012) Why are upper motor neuron signs difficult to elicit in amyotrophic lateral sclerosis? J Neurol Neurosurg Psychiatry 83(6):659–662
Walshe FMR (1914) The physiological significance of the reflex phenomena in spastic paralysis of the lower limbs. Brain 37:269–336
Isa T, Kinoshita M, Nishimura Y (2013) Role of direct vs. indirect pathways from the motor cortex to spinal motoneurons in the control of hand dexterity. Front Neurol 4:191
Zaaimi B, Edgley SA, Soteropoulos DS, Baker SN (2012) Changes in descending motor pathway connectivity after corticospinal tract lesion in macaque monkey. Brain 135:2277–2289
Acknowledgments
Dr. Simon gratefully acknowledges funding from the National Health and Medical Research Council of Australia and the Motor Neurone Disease Research Institute of Australia (grant #1039520). This work was supported by funding to Forefront, a collaborative research group dedicated to the study of motor neurone disease, from the National Health and Medical research Council of Australia Program Grant (#1037746). We are grateful to the research participants involved with the ForeFront research studies. Preliminary results from this study were presented in abstract form at the American Academy of Neurology Annual Meeting, San Diego, CA, March 21, 2013: Simon N, Bae JS, Mioshi E, Lin C, Vucic S, Kiernan M. The split leg in amyotrophic lateral sclerosis. Neurology February 12, 2013; 80 (Meeting Abstracts 1): P07.083.
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Simon, N.G., Lee, M., Bae, J.S. et al. Dissociated lower limb muscle involvement in amyotrophic lateral sclerosis. J Neurol 262, 1424–1432 (2015). https://doi.org/10.1007/s00415-015-7721-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-015-7721-8